Warfarin Patient Tips
Medically reviewed by Carmen Pope, BPharm. Last updated on July 26, 2023.
1. How it works
- Warfarin may be used to increase the time it takes for the blood to clot, often described as "thinning the blood".
- Warfarin works by blocking the formation of vitamin K-dependent clotting factors, inhibiting a vitamin K-dependent enzyme complex, as well as two anticoagulant proteins.
- Warfarin belongs to the class of drugs known as coumarins. Warfarin is also an anticoagulant.
2. Upsides
- Decreases the body's ability to form blood clots and may be used in the prevention and treatment of deep vein thrombosis (DVT) and pulmonary embolism (PE).
- May also be used to prevent blood clots from developing as a result of atrial fibrillation or cardiac valve replacement.
- May be given to decrease the risk of death following a heart attack (myocardial infarction) or stroke caused by a blood clot.
- No dosage adjustment is required in people with kidney disease but people with kidney disease should monitor their INR more frequently.
- Generic warfarin is available.
3. Downsides
If you are between the ages of 18 and 60, take no other medication or have no other medical conditions, side effects you are more likely to experience include:
- Bleeding is the most common side effect reported. Rarely, it may be severe or fatal. Other side effects reported include hypersensitivity reactions, elevated liver enzymes, nausea, vomiting, abdominal pain, diarrhea, flatulence, rash, itch, and hair loss.
- Warfarin has a narrow therapeutic range - meaning that there is a fine line between too much and too little. For this reason, regular blood monitoring of the international normalized ratio (INR) - a standardized number that determines the ability of your blood to clot - is required. The frequency of monitoring varies; daily monitoring is required initially. The frequency of ongoing monitoring depends on how a person responds but may need to increase for numerous reasons such as during times of illness or with dietary or medication changes.
- No one dosage fits all. The dosage schedule for warfarin needs to be tailored for each individual depending on their INR response to the drug and the condition being treated. Patient factors such as age, weight, race (Asian patients may need lower dosages), body weight, gender, concomitant medications, and comorbidities all affect dosage as do some genetic factors (for example, CYP2C9 and VKORC1 genotypes).
- Warfarin cannot break apart established blood clots, nor can it reverse damage to tissue that has already been starved of oxygen. It can; however, prevent the extension of existing blood clots and reduce the risk of part of that blood clot breaking off and lodging in another artery or vein.
- May not be suitable for some people including those with pre-existing bleeding problems, at high risk of falls, with liver or kidney disease, with diabetes, congestive heart failure, or high blood pressure.
- Should not be used by women who are pregnant or planning to become pregnant, except under specialist advice, as warfarin can harm a developing baby. At least one month should lapse from the last warfarin dose to conception.
- Warfarin interacts with numerous drugs including certain types of antibiotics, heart medications, oral contraceptives, pain medications, and acid suppressants. Warfarin also interacts with several types of botanicals, including coenzyme Q10, St. John’s wort, ginseng, echinacea, ginkgo, golden-seal; as well as grapefruit juice. See here for a full list of interactions.
Note: In general, seniors or children, people with certain medical conditions (such as liver or kidney problems, heart disease, diabetes, seizures) or people who take other medications are more at risk of developing a wider range of side effects. View complete list of side effects
4. Bottom Line
Warfarin tablets are effective at "thinning" the blood; however, several factors affect warfarin blood levels including diet (particularly the intake of vitamin K), ethnicity, other medications or supplements, and illness. Too much warfarin can cause major and potentially fatal bleeding.
5. Tips
- Take exactly as directed by your doctor. It may take several weeks or months to find the right dosage for you because the dosage of warfarin can vary depending on a person's age, weight, race (Asian patients may need lower dosages), body weight, gender, other medications, or medical conditions that they may have and genetic factors (for example, CYP2C9 and VKORC1 genotypes).
- An initial lower starting dose is recommended for seniors or the frail and in people of Asian descent.
- Loading doses (a bigger dose at the start) are no longer routinely recommended as these increase the risk of bleeding without offering any more rapid protection against clot formation.
- If you miss a dose, and it is the same day, you may take that dose. However, if you do not discover the missed dose until the next day, do not double up on the dose (just forgo the missed dose).
- You may need to temporarily stop or change your warfarin dosing schedule if you have planned surgery (including eye surgery) or a dental procedure. Discuss this with your surgeon or dentist before the procedure.
- Be aware that foods containing vitamin K can affect warfarin therapy. Try to eat a normal, balanced diet, to maintain a consistent intake of vitamin K - avoid eating too much of one thing (for example, a whole plate of broccoli, or a big bowl of salad greens). Foods high in vitamin K include kale, collards, broccoli, spinach, and other green leafy vegetables. Cranberry juice and alcohol may also affect warfarin levels so limit intake of these.
- Monitor yourself for signs of bleeding such as blood in your stools or urine, nose-bleeds, bleeding gums, excessive menstrual bleeding, or excessive bruising, and seek immediate medical advice. Also take care to minimize your risk of bleeding - avoid full-contact sports, be careful with knives, and try to minimize your risk of falling.
- Always adhere to your prescribed dosage schedule. Ask your doctor before you take or discontinue ANY other drug, including over-the-counter medicines and botanical (herbal) products. Ensure you get your blood levels monitored as instructed.
- Wear or carry identification that states you are taking warfarin tablets, in case of an emergency.
- Although Coumadin and Jantoven are both brands of warfarin, small changes in their formulation may mean your body reacts differently to each brand. Most experts recommend you always take the same brand of warfarin to help keep your INR levels stable.
- Contact your doctor if you develop severe diarrhea, an infection, or a fever.
- If you are a woman of childbearing capability, you should use adequate contraception while taking warfarin and for one month after the last dose to ensure you do not become pregnant because warfarin can harm a developing fetus. If you do inadvertently become pregnant, tell your doctor immediately. Although research has shown warfarin is not present in human milk, the risks versus benefits of warfarin use during breastfeeding should be considered as there is the potential for serious side effects in the infant. If warfarin is given during breastfeeding then infants should be monitored for bruising and bleeding.
6. Response and effectiveness
- Some slowing of the blood's ability to clot may be noticed within 24 hours; however, it can take from 72 to 96 hours for the full effects to be seen. One dose of warfarin lasts for 2 to 5 days. Effects are likely to accumulate with repeated dosing because of the time it takes for the affected vitamin K-dependent clotting factors to replenish.
- Desired INR range varies depending on condition and specific guidelines; however, the majority of guidelines aim for a target INR of 2.5 (range 2-3).
- Treatment duration also varies, from three months to life-long depending on the condition and other patient factors; generally, until the danger of thrombosis or embolism has passed.
- INR readings greater than 4 are associated with a higher risk of bleeding with no additional therapeutic benefit in most people.
- The hepatic enzyme CYP 2C9 is responsible for metabolizing the S-enantiomer of warfarin to its metabolite. This is a polymorphic enzyme and variants of this enzyme can result in decreased metabolism of warfarin. Patients with these variants may take longer to achieve a maximum INR effect.
7. Interactions
Medicines that interact with warfarin may either decrease its effect, affect how long it works, increase side effects, or have less of an effect when taken with warfarin. An interaction between two medications does not always mean that you must stop taking one of the medications; however, sometimes it does. Speak to your doctor about how drug interactions should be managed.
Common medications that may interact with warfarin include:
- acetaminophen
- amiodarone
- anticonvulsants such as carbamazepine, phenytoin or valproic acid
- antimicrobial agents, such as ciprofloxacin, clarithromycin, erythromycin, metronidazole
- apixaban
- aspirin
- cimetidine
- corticosteroids, such as prednisone and methylprednisone
- dabigatran
- medications that inhibit or induce CYP3A4 enzymes, such as fluconazole, ketoconazole, or ritonavir
- methotrexate
- mifepristone
- NSAIDs, such as ibuprofen, diclofenac, etodolac, and naproxen
- omeprazole
- rifampin
- St John's Wort
- tinzaparin.
In general, any medicine that can increase the risk of bleeding (such as clopidogrel, SSRI antidepressants [eg, citalopram, duloxetine, fluoxetine, venlafaxine], fish oils) may interact with warfarin.
Large amounts of vitamin K in the diet (such as that from spinach, green tea, chard, and kale) can also reduce the effectiveness of warfarin.
Short-term courses of some medications, such as antibiotics, antifungals, or corticosteroids, can affect the INR of warfarin and more frequent monitoring should be undertaken.
Warfarin is metabolized by several CYP450 enzymes, including CYP2C9, 2C19, 2C8, 2C18, 1A2, and 3A4. Inhibitors of CYP2C9, 1A2, or 3A4 can increase the effect of warfarin (increase the INR). Inhibitors of CYP2C9, 1A2, or 3A4 can decrease the effect of warfarin.
Alcohol may increase the risk of stomach bleeding with warfarin.
More frequent INR monitoring should be undertaken when starting or stopping botanicals, such as garlic, Ginkgo biloba, coenzyme Q10, St John's wort, and ginseng.
Note that this list is not all-inclusive and includes only common medications that may interact with warfarin. See here for a full list of interactions.
Related/similar drugs
Propranolol
Propranolol is a beta-blocker that is used to treat tremors, chest pain, high blood pressure, heart ...
Repatha
Repatha (evolocumab) is a PCSK9 inhibitor used to lower high cholesterol alongside dietary changes ...
Spironolactone
Spironolactone is a potassium-sparing diuretic that is primarily used to treat heart failure, high ...
Eliquis
Eliquis (apixaban) is used to reduce the risk of stroke and systemic embolism in patients with ...
Carvedilol
Carvedilol (Coreg) is used to treat heart failure and hypertension (high blood pressure). Includes ...
Aspirin
Aspirin is used to treat mild to moderate pain and to reduce fever or inflammation. Learn about ...
Furosemide
Furosemide is a loop diuretic used to treat fluid retention and high blood pressure by increasing ...
Jardiance
Jardiance (empagliflozin) is used to treat type 2 diabetes, chronic kidney disease and reduce the ...
Frequently asked questions
- Does Green Tea interact with any drugs?
- What is the antidote for warfarin?
- Is warfarin used as rat poison?
- Does Feverfew interact with any drugs?
- Why does warfarin cause purple toe syndrome?
- Does cranberry juice help prevent a UTI?
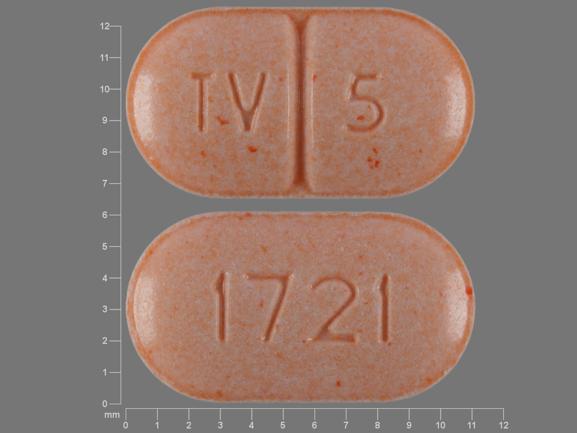
- Why are Warfarin tablets color-coded?
- Is your blood really thinner with warfarin?
More about warfarin
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (56)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Support group
- Drug class: coumarins and indandiones
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
References
- Warfarin. Revised: 03/2023. Golden State. https://www.drugs.com/pro/warfarin.html
Further information
Remember, keep this and all other medicines out of the reach of children, never share your medicines with others, and use warfarin only for the indication prescribed.
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Copyright 1996-2025 Drugs.com. Revision date: July 25, 2023.