Ambrisentan Side Effects
Medically reviewed by Drugs.com. Last updated on Jan 4, 2025.
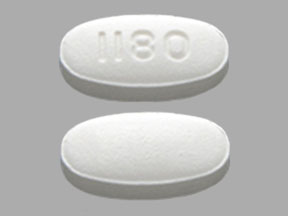
Applies to ambrisentan: oral tablet.
Important warnings
This medicine can cause some serious health issues
Oral route (tablet)
Embryo-fetal toxicityDo not administer ambrisentan to a pregnant female because it may cause fetal harm.
Ambrisentan is very likely to produce serious birth defects if used by pregnant females, as this effect has been seen consistently when it is administered to animals.Exclude pregnancy before the initiation of treatment with ambrisentan.
Females of reproductive potential must use acceptable methods of contraception during treatment with ambrisentan and for one month after treatment.
Obtain monthly pregnancy tests during treatment and 1 month after discontinuation of treatment.Because of the risks of embryo-fetal toxicity, for all female patients, ambrisentan is only available through a restricted program under a Risk Evaluation and Mitigation (REMS) called the Ambrisentan REMS.
Serious side effects of ambrisentan
Along with its needed effects, ambrisentan may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking ambrisentan:
More common side effects
- bloating or swelling of the face, arms, hands, lower legs, or feet
- rapid weight gain
- tingling of the hands or feet
- unusual weight gain or loss
Less common side effects
Incidence not known
- chest pain
- clay colored stools
- dark urine
- decrease in the amount of urine
- decreased appetite
- dilated neck veins
- extreme tiredness or weakness
- irregular breathing
- large, hive-like swelling on the face, eyelids, lips, tongue, throat, hands, legs, feet, or genitals
- loss of appetite
- nausea
- noisy, rattling breathing
- pale skin
- skin rash, itching
- stomach pain or tenderness
- troubled breathing at rest
- troubled breathing with exertion
- vomiting
- yellow skin or eyes
Get emergency help immediately if any of the following symptoms of overdose occur while taking ambrisentan:
Symptoms of overdose
- blurred vision
- confusion
- dizziness, faintness, or lightheadedness when getting up suddenly from a lying or sitting position
- sweating
Other side effects of ambrisentan
Some side effects of ambrisentan may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
Less common side effects
- difficulty having a bowel movement
- feeling of warmth
- redness of the face, neck, arms, and occasionally, upper chest
For healthcare professionals
Applies to ambrisentan: oral tablet.
General adverse events
The most common adverse reactions included: peripheral edema, nasal congestion, sinusitis, and flushing.[Ref]
Hematologic
- Common (1% to 10%): Hemoglobin decreased, anemia
- Postmarketing reports: Decreases in hemoglobin and hematocrit resulting in anemia requiring transfusion[Ref]
Decreases in hemoglobin and hematocrit were observed during the first few weeks of treatment and appeared to stabilize thereafter. Mean decreases in hemoglobin were 0.8 mg/dL with marked decreases in hemoglobin (greater than 15% decrease from baseline resulting in a value below the lower limit of normal) occurring in 7% of all patients. The frequency of a marked decrease in hemoglobin was greater with the 10 mg dose. The mechanism involved is unknown, but does not appear to be the result of hemorrhage or hemolysis.[Ref]
Cardiovascular
- Very common (10% or more): Peripheral edema (up to 28.4%)
- Common (1% to 10%): Flushing, palpitations, hypotension, right ventricular failure, chest pain, cardiac failure[Ref]
The incidence of peripheral edema in younger patients was similar to placebo (14% vs 13%) while the incidence in patients 65 years or older was greater in patients receiving drug (29% vs 4%).[Ref]
Respiratory
- Very common (10% or more): Nasal congestion (up to 10.4%)
- Common (1% to 10%): Sinusitis, nasopharyngitis, rhinitis, cough, upper respiratory infection, bronchitis, dyspnea, dyspnea exacerbated, pulmonary hypertension, epistaxis[Ref]
The occurrence of nasal congestion was dose-dependent.[Ref]
Gastrointestinal
- Common (1% to 10%): Abdominal pain, constipation, nausea, vomiting
- Postmarketing reports: Diarrhea[Ref]
Nervous system
- Very common (10% or more): Headache (19.4%)
- Common (1% to 10%): Dizziness, syncope
- Frequency not reported: Tinnitus[Ref]
Hypersensitivity
- Common (1% to 10%): Hypersensitivity[Ref]
Genitourinary
- Common (1% to 10%): Urinary tract infection[Ref]
Hepatic
- Common (1% to 10%): Hepatic transaminase increased
- Frequency not reported: Autoimmune hepatitis, hepatic injury[Ref]
The cumulative incidence of hepatic transaminases elevations greater than 3 times the upper limit of normal was 3.5% with a mean exposure duration of 79.5 weeks. The 12-week incidence was 0.8% (placebo-treated patients 2.3%). Hepatic transaminase elevations of greater than 8 times the upper limit of normal were reported in 0.2% of patients at 12 weeks and hepatic transaminase elevations greater than 6 times the upper limit of normal were reported in 0.5% at 1-year. An elevation of bilirubin to 2 times the upper limit of normal was reported in 1 case.[Ref]
Metabolic
- Very common (10% or more): Fluid retention[Ref]
Musculoskeletal
- Common (1% to 10%): Arthralgia[Ref]
Ocular
- Common (1% to 10%): Blurred vision, visual impairment
- Postmarketing reports: Visual disturbance[Ref]
Other
- Common (1% to 10%): Fatigue, asthenia
- Frequency not reported: Sudden hearing loss[Ref]
Psychiatric
Dermatologic
- Common (1% to 10%): Rash[Ref]
References
1. Cerner Multum, Inc. "UK Summary of Product Characteristics."
2. (2007) "Product Information. Letairis (ambrisentan)." Gilead Sciences
3. Cerner Multum, Inc. "Australian Product Information."
More about ambrisentan
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (15)
- Drug images
- Dosage information
- During pregnancy
- Drug class: agents for pulmonary hypertension
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Ambrisentan side effects can vary depending on the individual. Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Note: Medication side effects may be underreported. If you are experiencing side effects that are not listed, submit a report to the FDA by following this guide.