Zyclara: Package Insert / Prescribing Info
Package insert / product label
Generic name: imiquimod
Dosage form: cream
Drug classes: Topical anti-infectives, Topical antineoplastics
Medically reviewed by Drugs.com. Last updated on Oct 6, 2024.
On This Page
- Indications and Usage
- Dosage and Administration
- Dosage Forms and Strengths
- Contraindications
- Warnings and Precautions
- Adverse Reactions/Side Effects
- Use In Specific Populations
- Overdosage
- Description
- Clinical Pharmacology
- Nonclinical Toxicology
- Clinical Studies
- How Supplied/Storage and Handling
- Storage and Handling
- Patient Counseling Information
Highlights of Prescribing Information
ZYCLARA ®(imiquimod) cream, for topical use
Initial U.S. Approval: 1997
Indications and Usage for Zyclara
- ZYCLARA 2.5% and 3.75% is indicated for the topical treatment of clinically typical, visible, or palpable actinic keratoses (AK) of the face or balding scalp in immunocompetent adults. ( 1.1)
- ZYCLARA, 3.75% is indicated for the topical treatment of external genital and perianal warts (EGW) in immunocompetent patients 12 years of age or older. ( 1.2)
Zyclara Dosage and Administration
- For topical use only; not for oral, ophthalmic, intra-anal or intravaginal use. ( 2.1 )
- AK: Apply a thin layer once daily at bedtime to affected area (either entire face or balding scalp) for two 2-week treatment cycles separated by a 2-week no-treatment period. Apply up to 0.5 grams at each application. ( 2.2)
- EGW: Apply a thin layer once daily at bedtime until total clearance or up to 8 weeks. Apply up to 0.25 grams at each application. ( 2.3)
Dosage Forms and Strengths
Cream: 2.5% in pump bottles; 3.75% in pump bottles or unit-dose packets ( 3)
Contraindications
None. ( 4)
Warnings and Precautions
- Local Skin Reactions: Intense local inflammatory reactions can occur (e.g., skin weeping, erosion). Dosage interruption may be required. Severe vulvar swelling may occur and lead to urinary retention; interrupt dosing or discontinue for severe vulvar swelling. ( 2.2, 2.3, 5.1)
- Systemic Reactions: Flu-like signs and symptoms have occurred. Consider dosage interruption for systemic reactions. ( 5.2)
- Ultraviolet Light Exposure Risks:Avoid or minimize exposure to sunlight and sunlamps. Wear protective clothing. ( 5.3)
Adverse Reactions/Side Effects
Most common adverse reactions (≥4%) are local skin reactions (erythema, scabbing/crusting, flaking/scaling/dryness, edema, erosion/ulceration, exudate), headache, application site pain, application site irritation, application site pruritus, fatigue, influenza-like illness, and nausea. ( 6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Bausch Health US, LLC at 1-800-321-4576 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 9/2024
Full Prescribing Information
1. Indications and Usage for Zyclara
2. Zyclara Dosage and Administration
2.1 Important Dosage and Administration Instructions
ZYCLARA is for topical use only. ZYCLARA is not for oral, ophthalmic, intra-anal or intravaginal use. Instruct patients on proper application technique.
Wash hands before and after applying ZYCLARA.
Prime the ZYCLARA pump bottle before first use by repeatedly depressing the actuator until the cream is dispensed. It is not necessary to repeat this priming process during treatment.
If a ZYCLARA dose is missed, apply the next dose at the regularly scheduled time.
Avoid contact with the eyes, lips, nostrils, or inside the anus and vagina.
Prescribe no more than 2 boxes (56 packets) or two 7.5 g bottle pumps of ZYCLARA for the entire treatment course for AK or EGW.
Discard partially used packets and do not reuse. Discard pump bottles after completion of a full treatment course.
2.2 Dosage and Administration for Actinic Keratosis
Use ZYCLARA, 2.5% or 3.75% for the treatment of AK. Apply a thin layer of ZYCLARA once daily before bedtime to the area with AK (either entire face or balding scalp) for two 2-week treatment cycles separated by a 2-week no-treatment period. Rub in until the cream is no longer visible. Apply up to 0.5 grams (two packets or two full actuations of the pump) of ZYCLARA at each application. Leave ZYCLARA on the skin for approximately 8 hours and then remove with mild soap and water.
For local skin reactions, a dosage interruption of several days may be taken if required based on the patient’s discomfort or severity of the local skin reaction [see Warnings and Precautions (5.1)]. Do not extend either 2-week treatment cycle due to missed doses or rest periods .Assess response to treatment after resolution of local skin reactions.
A transient increase in lesion counts may be observed during treatment; however, continue dosing as prescribed. Continue treatment for the full treatment course even if all AK appear to be gone.
2.3 Dosage and Administration for External Genital Warts
Use ZYCLARA, 3.75% for the treatment of EGW. Apply a thin layer of ZYCLARA cream once daily before bedtime to EGW until total clearance or for up to 8 weeks. To treat the wart area, use up to 0.25 grams (one packet or one full actuation of the pump) at each application. Leave ZYCLARA on the skin for approximately 8 hours and then remove with mild soap and water.
For local skin reactions, a dosage interruption of several days may be taken if required by the patient's discomfort or severity of the local skin reaction; resume treatment once the reaction subsides [see Warnings and Precautions (5.1)] .
Non-occlusive dressings such as cotton gauze or cotton underwear may be used in the management of skin reactions.
Inform uncircumcised patients treating warts under the foreskin to retract the foreskin and clean the area daily.
ZYCLARA may weaken condoms and vaginal diaphragms, therefore, concurrent use is not recommended.
3. Dosage Forms and Strengths
ZYCLARA is a white to faintly yellow cream available as:
- Cream: 2.5%, in pump bottles. Each pump bottle, when actuated after priming, delivers 0.235 grams of cream.
- Cream: 3.75%, in unit-dose packets and pump bottles. Each packet contains 0.25 grams of cream and each pump bottle, when actuated after priming, delivers 0.235 grams of cream.
5. Warnings and Precautions
5.1 Local Skin Reactions
Local skin reactions including skin weeping or erosion have been reported with use of ZYCLARA and can occur after a few applications [see Adverse Reactions (6)]. Concomitant use of ZYCLARA and any other imiquimod products, in the same treatment area, may increase the risk for and severity of local skin reactions.
ZYCLARA Cream has the potential to exacerbate inflammatory conditions of the skin, including chronic graft versus host disease.
Severe local inflammatory reactions of the female external genitalia can lead to severe vulvar swelling and to urinary retention.
Avoid sexual (genital, anal, oral) contact while ZYCLARA is on the skin.
To reduce the risk of local skin reactions and manage local skin reactions that occur with ZYCLARA treatment:
- Avoid concomitant use of ZYCLARA with any other imiquimod product in the same treatment area.
- Avoid application of ZYCLARA to skin that is not intact (i.e., any area with an abrasion, cut, burn, rash, infection, or other condition that has altered skin integrity).
- An interruption of dosing may be required for local skin reactions [ see Dosage and Administration (2.2, 2.3)], Interrupt dosing or discontinue ZYCLARA for severe vulvar swelling [see Dosage and Administration (2.3)].
- If severe local skin reactions occur, instruct patients to remove ZYCLARA by washing the treatment area with mild soap and water.
5.2 Systemic Reactions
Flu-like signs and symptoms have been reported with use of ZYCLARA and may accompany, or even precede, local skin reactions [see Adverse Reactions (6)] . Signs and symptoms may include fatigue, nausea, fever, myalgias, arthralgias, malaise and chills. Concomitant use of ZYCLARA and any other imiquimod products may increase the risk for and severity of systemic reactions.
Lymphadenopathy occurred in 2% of subjects with AK treated with ZYCLARA, 3.75% and in 3% of subjects treated with ZYCLARA, 2.5% and in no patients in the vehicle arm [see Adverse Reactions (6.1)]. This reaction resolved in all subjects by 4 weeks after completion of treatment.
Consider an interruption of dosing if systemic reactions occur .
5.3 Ultraviolet Light Exposure Risks
ZYCLARA may cause heightened sunburn susceptibility. Avoid or minimize exposure to sunlight (including sunlamps) during use of ZYCLARA. Instruct patients to use sunscreen and wear protective clothing (e.g., a hat). Advise patients not to use ZYCLARA until fully recovered from a sunburn.
5.4 Immune Cell Activation in Autoimmune Disease
Imiquimod activates immune cells [see Clinical Pharmacology (12.2)] . Carefully monitor patients with pre-existing autoimmune conditions who are using ZYCLARA.
6. Adverse Reactions/Side Effects
The following clinically significant adverse reactions are described elsewhere in the labeling:
- Local Skin Reactions [see Warnings and Precautions (5.1)]
- Systemic Reactions [see Warnings and Precautions (5.2)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Actinic Keratosis
The data described below reflect exposure to ZYCLARA or vehicle in 479 subjects with AK enrolled in two double-blind, vehicle-controlled trials (Studies AK1 and AK2) [see Clinical Studies (14.1)] . Subjects applied up to two packets of ZYCLARA, 3.75%, ZYCLARA, 2.5%, or vehicle once daily, to the skin of the affected area (either entire face or balding scalp) for two 2-week treatment cycles separated by a 2-week no treatment period. Selected adverse reactions are listed in Table 1.
| Adverse Reaction | ZYCLARA, 3.75%
(N=160) | ZYCLARA, 2.5%
(N=160) | Vehicle
(N=159) |
|---|---|---|---|
|
Headache |
10 (6%) |
3 (2%) |
5 (3%) |
|
Application site pruritus |
7 (4%) |
6 (4%) |
1 (<1%) |
|
Fatigue |
7 (4%) |
2 (1%) |
0 |
|
Nausea |
6 (4%) |
1 (1%) |
2 (1%) |
|
Application site irritation |
5 (3%) |
4 (3%) |
0 |
|
Application site pain |
5 (3%) |
2 (1%) |
0 |
|
Pyrexia |
5 (3%) |
0 |
0 |
|
Anorexia |
4 (3%) |
0 |
0 |
|
Dizziness |
4 (3%) |
1 (<1%) |
0 |
|
Herpes simplex |
4 (3%) |
0 |
1 (<1%) |
|
Lymphadenopathy |
3 (2%) |
4 (3%) |
0 |
|
Diarrhea |
3 (2%) |
2 (1%) |
0 |
|
Arthralgia |
2 (1%) |
4 (3%) |
0 |
|
Influenza like illness |
1 (<1%) |
6 (4%) |
0 |
|
Oral herpes |
0 |
4 (3%) |
0 |
|
Cheilitis |
0 |
3 (2%) |
0 |
Local skin reactions were recorded as adverse reactions if they extended beyond the treatment area, or required any medical intervention, or resulted in patient discontinuation from the trial. The incidence and severity of selected local skin reactions are shown in Table 2.
| All Grades* (%)
Severe (%) | ZYCLARA, 3.75%
(N=160) | ZYCLARA, 2.5%
(N=160) | Vehicle
(N=159) |
|---|---|---|---|
|
|||
|
Erythema
*
|
96%
|
96%
|
78%
|
|
Scabbing/Crusting
*
|
93%
|
84%
|
45%
|
|
Flaking/Scaling/Dryness
*
|
91%
|
88%
|
77%
|
|
Edema
*
|
75%
|
63%
|
19%
|
|
Erosion/Ulceration
*
|
62%
|
52%
|
9%
|
|
Exudate
*
|
51%
|
39%
|
4%
|
In the AK trials, 11% (17/160) of subjects in the ZYCLARA, 3.75% arm, 7% (11/160) of subjects in the ZYCLARA, 2.5% arm, and 0% in the vehicle arm required rest periods due to adverse local skin reactions.
Other adverse reactions observed in subjects treated with ZYCLARA included: application site bleeding, application site swelling, chills, dermatitis, herpes zoster, insomnia, lethargy, myalgia, pancytopenia, pruritus, squamous cell carcinoma, and vomiting.
External Genital Warts
In two double-blind, placebo-controlled trials 602 subjects with EGW applied up to one packet of ZYCLARA, 3.75% or vehicle to all warts once daily for up to 8 weeks (Studies EGW1 and EGW2) [see Clinical Studies (14.2)] .
The most frequently reported adverse reactions were application site reactions and local skin reactions. Selected adverse reactions are listed in Table 3.
|
Adverse Reaction |
ZYCLARA, 3.75%
|
Vehicle
|
|
Application site pain |
28 (7%) |
1 (<1%) |
|
Application site irritation |
24 (6%) |
2 (1%) |
|
Application site pruritus |
11 (3%) |
2 (1%) |
|
Vaginitis bacterial* |
6 (3%) |
2 (2%) |
|
Headache |
6 (2%) |
|
*Percentage based on female population of 6/216 for ZYCLARA, 3.75% and 2/106 for vehicle
Local skin reactions were recorded as adverse reactions if they extended beyond the treatment area, or required any medical intervention, or resulted in patient discontinuation from the trial. The incidence and severity of selected local skin reactions are shown in Table 4.
| All Grades* (%)
Severe (%) | ZYCLARA, 3.75%
(N=400) | Vehicle
(N=202) |
|---|---|---|
|
||
|
Erythema
*
|
70%
|
27%
|
|
Edema
*
|
41%
|
8%
|
|
Erosion/ulceration
*
|
36%
|
4%
|
|
Exudate
*
|
34%
|
2%
|
The frequency and severity of local skin reactions were similar in both sexes, with the following exceptions: a) flaking/scaling occurred in 40% of males and in 26% of females and b) scabbing/crusting occurred in 34% of males and in 18% of females.
In Studies EGW1 and EGW2, 32% (126/400) of subjects who used ZYCLARA, 3.75% and 2% (4/202) of subjects who used vehicle discontinued treatment temporarily (required rest periods) due to adverse local skin reactions, and 1% (3/400) of subjects who used ZYCLARA, 3.75% discontinued treatment permanently due to local skin/application site reactions.
Other adverse reactions reported in subjects treated with ZYCLARA, 3.75% included: rash, back pain, application site rash, application site cellulitis, application site excoriation, application site bleeding, scrotal pain, scrotal erythema, scrotal ulcer, scrotal edema, sinusitis, nausea, pyrexia, and influenza-like symptoms.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of imiquimod. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Application Site Disorders: tingling at the application site
Body as a Whole: angioedema
Cardiovascular: capillary leak syndrome, cardiac failure, cardiomyopathy, pulmonary edema, arrhythmias (tachycardia, supraventricular tachycardia, atrial fibrillation, palpitations), chest pain, ischemia, myocardial infarction, syncope
Endocrine: thyroiditis
Gastrointestinal System Disorders: abdominal pain
Hematological: decreases in red cell, white cell and platelet counts (including idiopathic thrombocytopenic purpura), lymphoma
Hepatic: abnormal liver function
Infections and Infestations: herpes simplex
Musculoskeletal System Disorders: arthralgia
Neuropsychiatric: agitation, cerebrovascular accident, convulsions (including febrile convulsions), depression, insomnia, multiple sclerosis aggravation, paresis, suicide
Respiratory: dyspnea
Urinary System Disorders: proteinuria, urinary retention, dysuria
Skin and Appendages: exfoliative dermatitis, erythema multiforme, hyperpigmentation, hypertrophic scar, hypopigmentation
Vascular: Henoch-Schönlein purpura syndrome
8. Use In Specific Populations
8.1 Pregnancy
Risk Summary
Available data from case reports and case series have not established a drug-associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes when imiquimod is used during pregnancy. There are no controlled or large-scale epidemiologic studies and no exposure registries with imiquimod use in pregnant women. In animal reproduction studies, there were no adverse developmental effects observed after oral administration of imiquimod in pregnant rats and intravenous administration of imiquimod in pregnant rabbits during organogenesis at doses up to 28 times and 115 times, respectively, the maximum recommended human dose (MRHD) (see Data).
The background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defects, loss, and other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Data
Animal Data
The MRHD was set at two packets per treatment of ZYCLARA, 3.75%, (18.75 mg imiquimod) for the animal multiples of human exposure presented in this label.
Systemic embryofetal development studies were conducted in rats and rabbits. Oral doses of 1, 5, and 20 mg/kg/day imiquimod were administered during the period of organogenesis to pregnant female rats. In the presence of maternal toxicity, fetal effects noted at 20 mg/kg/day (163 times the MRHD based on AUC comparison) included increased resorptions, decreased fetal body weights, delays in skeletal ossification, bent limb bones, and two fetuses in one litter (2 of 1567 fetuses) demonstrated exencephaly, protruding tongues, and low-set ears. No treatment-related effects on embryofetal toxicity or malformation were noted at 5 mg/kg/day (28 times the MRHD based on AUC comparison).
Intravenous doses of 0.5, 1, and 2 mg/kg/day imiquimod were administered during the period of organogenesis to pregnant female rabbits. No treatment-related effects on embryofetal toxicity or malformation were noted at 2 mg/kg/day (2.1 times the MRHD based on BSA comparison), the highest dose evaluated in this study, or 1 mg/kg/day (115 times the MRHD based on AUC comparison).
A combined fertility and peri- and postnatal development study was conducted in rats. Oral doses of 1, 1.5, 3, and 6 mg/kg/day imiquimod were administered to male rats from 70 days prior to mating through the mating period and to female rats from 14 days prior to mating through parturition and lactation. No effects on growth, fertility, reproduction, or postnatal development were noted at doses up to 6 mg/kg/day (25 times the MRHD based on AUC comparison), the highest dose evaluated in this study. In the absence of maternal toxicity, bent limb bones were noted in the F1 fetuses at a dose of 6 mg/kg/day (25 times the MRHD based on AUC comparison). This fetal effect was also noted in the oral rat embryofetal development study conducted with imiquimod. No treatment-related malformations were noted at 3 mg/kg/day (12 times the MRHD based on AUC comparison).
8.2 Lactation
Risk Summary
There is no information regarding the presence of topically administered imiquimod in human milk, the effects on the breastfed infant, or the effects on milk production. Systemic concentration following topical administration of imiquimod cream is low; therefore, transfer of ZYCLARA into breastmilk is likely to be low [see Clinical Pharmacology (12.3)].
The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for ZYCLARA and any potential adverse effects on the breastfed infant from ZYCLARA or from the underlying maternal condition.
Clinical Considerations
Avoid application of ZYCLARA to areas with increased risk for potential ingestion by or ocular exposure to the breastfeeding child.
8.4 Pediatric Use
Actinic Keratosis
The safety and effectiveness of ZYCLARA for the treatment of AK in pediatric patients have not been established.
External Genital Warts
The safety and effectiveness of ZYCLARA for the treatment of EGW in pediatric patients 12 years of age and older have been established. Use of ZYCLARA for this indication is supported by evidence from adequate and well controlled trials in adults and pediatric subjects [see Clinical Studies (14.2)] . The safety and effectiveness of ZYCLARA for the treatment of EGW in pediatric patients less than 12 years of age have not been established.
Molluscum Contagiosum
The safety and effectiveness of ZYCLARA for the treatment of molluscum contagiosum (MC) in pediatric patients have not been established. Safety and effectiveness of imiquimod cream, 5% was not demonstrated in two randomized, vehicle-controlled, double-blind trials involving 702 pediatric subjects with MC (470 exposed to imiquimod cream; median age 5 years, range 2-12 years).
Adverse reactions reported in pediatric subjects with MC (and not previously reported) included otitis media (5% imiquimod cream vs. 3% vehicle) and conjunctivitis (3% imiquimod cream vs. 2% vehicle).
In a pharmacokinetics trial in subjects aged 2 to 12 years with extensive MC involving a least 10% of total body surface area; among the 20 subjects with evaluable laboratory assessments, the median white blood cell (WBC) count decreased by 1.4 x 10 9/L and the median absolute neutrophil count decreased by 1.42 x 10 9/L.
8.5 Geriatric Use
Of the 320 subjects treated with ZYCLARA in the AK clinical trials, 150 subjects (47%) were 65 years of age or older. No overall differences in safety or effectiveness of ZYCLARA have been observed between subjects 65 years of age and older and younger adult subjects.
Of the 400 subjects treated with ZYCLARA in the EGW clinical studies, 5 subjects (1%) were 65 years or older. Clinical studies of ZYCLARA for EGW did not include sufficient numbers of subjects aged 65 years of age and older to determine whether they respond differently from younger adult subjects.
10. Overdosage
Topical overdosing of ZYCLARA could result in an increased incidence of severe local skin reactions and may increase the risk for systemic reactions.
Hypotension was reported in a clinical trial following multiple oral imiquimod doses of >200 mg (equivalent to ingestion of the imiquimod content of more than 21 packets or pump actuations of ZYCLARA, 3.75% or more than 32 pump actuations of ZYCLARA, 2.5%). The hypotension resolved following oral or intravenous fluid administration. Consider contacting the Poison Help line (1-800-222-1222) or a medical toxicologist for additional overdosage management recommendations.
11. Zyclara Description
ZYCLARA (imiquimod) cream, 2.5% or 3.75% is for topical administration. Each gram contains 25 mg or 37.5 mg of imiquimod, respectively, in a white to faintly yellow oil-in-water cream base consisting of benzyl alcohol, cetyl alcohol, glycerin, isostearic acid, methylparaben, polysorbate 60, propylparaben, purified water, sorbitan monostearate, stearyl alcohol, white petrolatum, and xanthan gum.
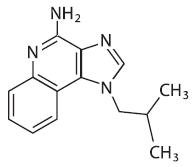
Chemically, imiquimod is 1-(2-methylpropyl)-1 H-imidazol[4,5-c]quinolin-4-amine. Imiquimod has a molecular formula of C 14H 16N 4and a molecular weight of 240.3. Its structural formula is:
12. Zyclara - Clinical Pharmacology
12.1 Mechanism of Action
The mechanism of action of ZYCLARA in the treatment of AK and EGW is unknown.
12.2 Pharmacodynamics
The pharmacodynamics of ZYCLARA are unknown.
Imiquimod is a Toll-like receptor 7 agonist that activates immune cells. Topical application to skin is associated with increases in markers for cytokines and immune cells.
12.3 Pharmacokinetics
Absorption
Following dosing with two packets of ZYCLARA, 3.75% once daily (18.75 mg imiquimod/day) for up to 3 weeks, systemic absorption of imiquimod was observed in all subjects when ZYCLARA was applied to the face and/or scalp in 17 subjects with at least 10 AK lesions. The mean peak serum imiquimod concentration at the end of the trial was approximately 0.323 ng/mL. The median time to maximal concentrations (T max) occurred at 9 hours after dosing. Based on the plasma half-life of imiquimod observed at the end of the trial, 29.3±17.0 hours, steady-state concentrations can be anticipated to occur by Day 7 with once-daily dosing.
Systemic absorption of imiquimod (up to 9.4 mg [one packet]) across the affected skin of 18 subjects with EGW was observed with once daily dosing for 3 weeks in all subjects. The subjects had either a minimum of 8 warts (range 8-93) or a surface area involvement of greater than 100 mm 2(range 15-620 mm 2) at trial entry. The mean peak serum imiquimod concentration at Day 21 was 0.488 +/- 0.368 ng/mL. The median time to maximal concentrations (T max) occurred 12 hours after dosing. Based on the plasma half-life of imiquimod observed at the end of the trial, 24.1 +/- 12.4 hours, steady-state concentrations can be anticipated to occur by Day 7 with once daily dosing. Because of the small number of subjects present (13 males, 5 females) it was not possible to select out or do an analysis of absorption based on sex/site of application.
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
In an oral (gavage) rat carcinogenicity study, imiquimod was administered to Wistar rats on a 2 times per week (up to 6 mg/kg/day) or daily (3 mg/kg/day) dosing schedule for 24 months. No treatment-related tumors were noted in the oral rat carcinogenicity study up to the highest doses tested in this study of 6 mg/kg administered 2 times per week in female rats (7.1 times the MRHD based on weekly AUC comparison), 4 mg/kg administered 2 times per week in male rats (6.1 times the MRHD based on weekly AUC comparison) or 3 mg/kg administered 7 times per week to male and female rats (12 times the MRHD based on weekly AUC comparison).
In a dermal mouse carcinogenicity study, imiquimod cream (up to 5 mg/kg/application imiquimod or 0.3% imiquimod cream) was applied to the backs of mice 3 times per week for 24 months. A statistically significant increase in the incidence of liver adenomas and carcinomas was noted in high dose male mice compared to control male mice (21 times the MRHD based on weekly AUC comparison). An increased number of skin papillomas was observed in vehicle cream control group animals at the treated site only.
Imiquimod revealed no evidence of mutagenic or clastogenic potential based on the results of five in vitro genotoxicity tests (Ames assay, mouse lymphoma L5178Y assay, Chinese hamster ovary cell chromosome aberration assay, human lymphocyte chromosome aberration assay and SHE cell transformation assay) and three in vivo genotoxicity tests (rat and hamster bone marrow cytogenetics assay and a mouse dominant lethal test).
Daily oral administration of imiquimod to rats, throughout mating, gestation, parturition and lactation, demonstrated no effects on growth, fertility or reproduction, at doses up to 25 times the MRHD based on AUC comparison.
14. Clinical Studies
14.1 Actinic Keratosis
In two double-blind, randomized, vehicle-controlled clinical trials, 479 subjects with AK were treated with ZYCLARA, 3.75%, ZYCLARA, 2.5%, or vehicle (Studies AK1 and AK2). Trials enrolled subjects 18 years of age or older with 5 to 20 typical visible or palpable AK lesions of the face or scalp. ZYCLARA or vehicle was applied to either the entire face (excluding ears) or balding scalp once daily for two 2-week treatment cycles separated by a 2-week no-treatment period. Subjects then continued in the trial for an 8-week follow-up period during which they returned for clinical observations and safety monitoring. Trial subjects ranged from 36 to 90 years of age and 54% had Fitzpatrick skin type I or II. All ZYCLARA-treated subjects were White.
On a scheduled dosing day, up to two packets of the trial cream were applied to the entire treatment area prior to normal sleeping hours and left on for approximately 8 hours. Efficacy was assessed by AK lesion counts at the 8-week post-treatment visit. All AKs in the treatment area were counted, including baseline lesions as well as lesions which appeared during therapy.
Complete clearance required absence of any lesions including those that appeared during therapy in the treatment area. Complete and partial clearance rates are shown in Tables 5 and 6 below. Partial clearance rate was defined as the percentage of subjects in whom the number of baseline AKs was reduced by 75% or more. The partial clearance rate was measured relative to the numbers of AK lesions at baseline.
| ZYCLARA, 3.75% | ZYCLARA, 2.5% | Vehicle
|
|
|---|---|---|---|
|
Study AK1 |
26% (21/81) |
23% (19/81) |
3% (2/80) |
|
Study AK2 |
46% (36/79) |
38% (30/79) |
10% (8/79) |
| ZYCLARA, 3.75% | ZYCLARA, 2.5% | Vehicle
|
|
|---|---|---|---|
|
Study AK1 |
46% (37/81) |
42% (34/81) |
19% (15/80) |
|
Study AK2 |
73% (58/79) |
54% (43/79) |
27% (21/79) |
During treatment, 86% (138/160) of ZYCLARA 3.75% subjects and 84% (135/160) of ZYCLARA, 2.5% subjects experienced a transient increase in lesions evaluated as AK relative to the number present at baseline within the treatment area.
14.2 External Genital Warts
In two double-blind, randomized, placebo-controlled clinical trials, 601 subjects with EGW were treated with ZYCLARA, 3.75% or a matching vehicle (Studies EGW1 and EGW2). Trials enrolled subjects aged from 15 to 81 years. The baseline wart area ranged from 6 to 5,579 mm 2(median 60 mm 2) and the baseline wart count ranged from 2 to 48 warts. Most subjects had two or more treated anatomic areas at baseline. Anatomic areas included: inguinal, perineal, and perianal areas (both sexes); the glans penis, penis shaft, scrotum, and foreskin (in males); and the vulva (in females). Up to one packet of trial cream was applied once daily. The trial cream was applied to all warts prior to normal sleeping hours and left on for approximately 8 hours. Subjects continued applying the trial cream for up to 8 weeks, stopping if they achieved complete clearance of all (baseline and new) warts in all anatomic areas. Subjects who achieved complete clearance of all warts at any time up to the Week 16 visit entered a 12-week follow-up period to assess recurrence.
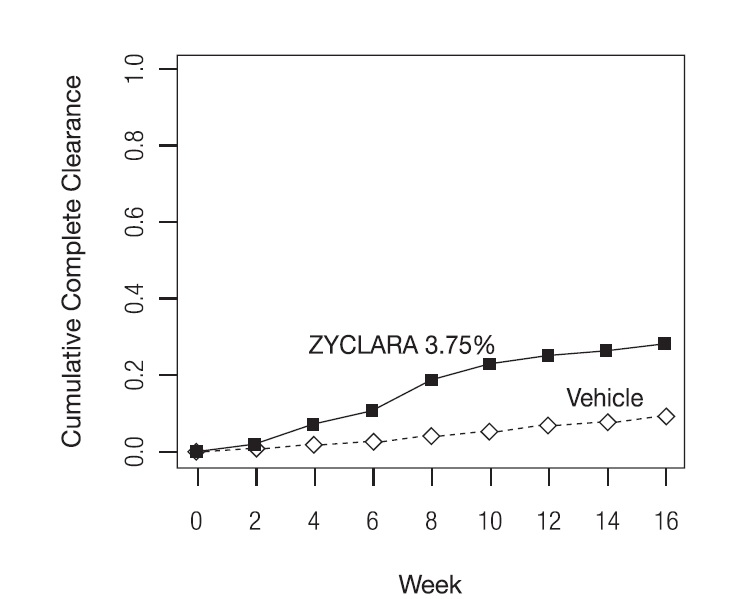
Complete clearance was defined as clearance of all warts (baseline and new) in all anatomic areas within 16 weeks from baseline. The complete clearance rates are shown in Table 7. The proportions of subjects who achieved complete clearance at or before a given week (cumulative proportion) for the combined studies are shown in Figure 1. Complete clearance rates by sex for the combined studies are shown in Table 8.
| ZYCLARA, 3.75% | Vehicle | |
|---|---|---|
|
Study EGW1 |
53/195 (27%) |
10/97 (10%) |
|
Study EGW2 |
60/204 (29%) |
9/105 (9%) |
Figure 1: Cumulative Proportion of Subjects Achieving Complete Clearance of EGW by a Given Week (Studies EGW1 and EGW2)
| ZYCLARA, 3.75% | Vehicle | |
|---|---|---|
|
Females |
79/216 (37%) |
15/106 (14%) |
|
Males |
34/183 (19%) |
4/96 (4%) |
Of the 113 ZYCLARA, 3.75%-treated subjects who achieved complete clearance in the two trials, 17 (15%) subjects had a recurrence within 12 weeks.
No trials were conducted directly comparing the 3.75% and 5% concentrations of imiquimod cream in the treatment of external genital warts.
16. How is Zyclara supplied
How Supplied
ZYCLARA (imiquimod) cream is white to faintly yellow in color.
ZYCLARA, 2.5% and 3.75% is supplied as white plastic 30 mL pump bottles, equipped with a white cap. The 7.5 g pump bottle delivers no fewer than 28 full actuations:
- 2.5% cream, NDC 99207-276-75
- 3.75% cream, NDC 99207-271-75
ZYCLARA, 3.75% is also supplied in unit-dose plastic laminate packets which contain 0.25 g of cream:
- 3.75% cream, box of 28 packets, NDC 99207-270-28
17. Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Important Administration Instructions
Inform all patients of the following [see Dosage and Administration (2.1)] :
-
- ZYCLARA is for topical use only and avoid contact with the eyes, lips, nostrils, or inside the anus and vagina. Instruct patients to rinse their mouth or eyes with water right away if contact with these areas occur.
- Wash their hands before and after applying ZYCLARA.
- If a ZYCLARA dose is missed, apply the next dose at the regularly scheduled time.
- Discard and do not reuse partially used packets.
- Discard pump bottles after completion of a full treatment course.
Inform patients with EGW of the following [see Dosage and Administration 2.3and Warnings and Precautions (5.1)] :
-
- Uncircumcised patients treating warts under the foreskin should retract the foreskin and clean the area daily.
- ZYCLARA may weaken condoms and vaginal diaphragms; therefore, concurrent use is not recommended.
- Avoid sexual (genital, anal, oral) contact while ZYCLARA is on the skin.
- Do not bandage or otherwise occlude the treatment area.
Lactation
Advise breastfeeding women to avoid application of ZYCLARA to areas with increased risk for potential ingestion by or ocular exposure to the breastfeeding child [see Use in Specific Populations (8.2)].
Local Skin Reactions
Inform patients of the following [see Dosage and Administration (2.2, 2.3), and Warnings and Precautions (5.1)] :
-
- Local skin reactions may occur during treatment with ZYCLARA, ranging from mild to severe in intensity and extending beyond the application site onto the surrounding skin, and may require an interruption of dosing.
- For female patients being treated for EGW, apply ZYCLARA at the opening of the vagina, avoiding intravaginal application because local skin reactions may cause difficulty in passing urine.
- If severe local skin reactions occur, remove ZYCLARA by washing the treatment area with mild soap and water.
- Contact their healthcare provider promptly if they experience any sign or symptom at the application site that restricts or prohibits their daily activity or makes continued application of ZYCLARA difficult.
- Because of local skin reactions, during treatment and until healed, the treatment area is likely to appear noticeably different from normal skin.
Local Hypopigmentation and Hyperpigmentation
Inform patients that localized hypopigmentation and hyperpigmentation have been reported following use of imiquimod cream and these skin color changes may be permanent in some patients [see Adverse Reactions (6.2)] .
Systemic Reactions
Inform patients that they may experience flu-like systemic signs and symptoms during treatment with ZYCLARA and these symptoms may require an interruption of dosing [see Warnings and Precautions (5.2)] .
Ultraviolet Light Exposure Risks
Instruct patients to avoid or minimize exposure to natural or artificial sunlight (tanning beds or UVA/B treatment) while using ZYCLARA. Instruct patients to use protective clothing and to not use ZYCLARA if sunburned [see Warnings and Precautions (5.3)] .
Distributed by:
Bausch Health US, LLC
Bridgewater, NJ 08807 USA
Manufactured by:
3M Health Care Limited
Loughborough, Leicestershire, LE11 5Sd
United Kingdom
Patented. See https://patents.ortho-dermatologics.com for US patent information.
ZYCLARA is a trademark of Bausch Health Companies Inc. or its affiliates.
© 2024 Bausch Health Companies Inc. or its affiliates
9740701
Patient Information
This Patient Information has been approved by the U.S. Food and Drug Administration. Revised: 09/2024
9740701
PRINCIPAL DISPLAY PANEL - 28 Single-Use Packets Carton
NDC99207-270-28
Rx only
Zyclara®
(imiquimod) Cream
3.75%
Box of 28 Single Use Packets
Net Wt. Per Packet
0.25 g
Net Wt. Per Box
7 g
For Topical Use Only
Not for Ophthalmic, Oral or Intravaginal Use
9741900
20002922A
| ZYCLARA
imiquimod cream |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| ZYCLARA
imiquimod cream |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| ZYCLARA
imiquimod cream |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| Labeler - Bausch Health US, LLC (831922468) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Kindeva Drug Delivery Limited | 225650929 | manufacture(99207-270, 99207-271, 99207-276) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Bausch Health Companies Inc. | 245141858 | manufacture(99207-270, 99207-271, 99207-276) | |
Frequently asked questions
- What are the most common skin conditions? (with photos)
- Does Zyclara work for genital warts?
- Who makes Zyclara and where is it manufactured?
- Does duct tape really remove warts?
- Is imiquimod the same as Aldara?
- What are the side effects of the HPV vaccine?
More about Zyclara (imiquimod topical)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (49)
- Side effects
- Dosage information
- During pregnancy
- Generic availability
- FDA approval history
- Drug class: topical anti-infectives
- Breastfeeding