Zaldyon: Package Insert / Prescribing Info
Package insert / product label
Generic name: mesalamine
Dosage form: tablet, delayed release
Drug class: 5-aminosalicylates
Medically reviewed by Drugs.com. Last updated on Aug 20, 2023.
On This Page
- Indications and Usage
- Dosage and Administration
- Dosage Forms and Strengths
- Contraindications
- Warnings and Precautions
- Adverse Reactions/Side Effects
- Drug Interactions
- Use In Specific Populations
- Overdosage
- Description
- Clinical Pharmacology
- Nonclinical Toxicology
- Clinical Studies
- How Supplied/Storage and Handling
- Patient Counseling Information
Highlights of Prescribing Information
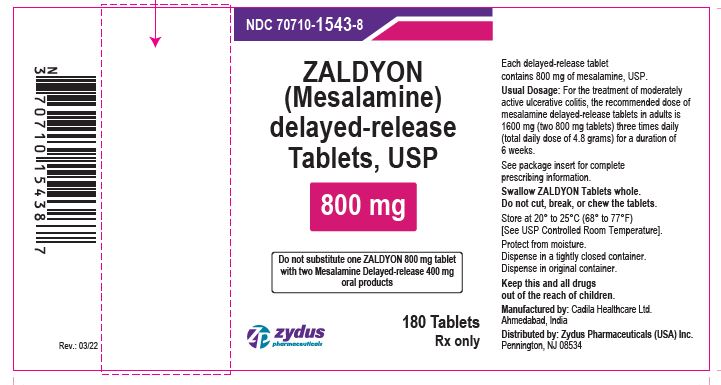
ZALDYON (mesalamine) delayed-release tablets, for oral use
Initial U.S. Approval: 1987
Recent Major Changes
| |
| Renal Impairment (5.1) | 11/2022 |
Indications and Usage for Zaldyon
Zaldyon Dosage and Administration
Important Administration Instructions:
- Do not substitute one ZALDYON 800 mg tablet for two mesalamine delayed-release 400 mg oral products. (2.1)
- Evaluate renal function prior to initiation of ZALDYON. (2.1,5.1)
- Take on an empty stomach, at least 1 hour before and 2 hours after a meal. (2.1)
- Swallow whole; do not cut, break or chew the tablets. (2.1)
- Drink an adequate amount of fluids. (2.1,5.7)
Treatment of Moderately Active Ulcerative Colitis:
- Recommended dosage is 1600 mg (two 800 mg tablets) three times daily for 6 weeks. (2.2)
Dosage Forms and Strengths
- Delayed-release tablets: 800 mg (3)
Contraindications
Warnings and Precautions
- Renal Impairment: Assess renal function at the beginning of treatment and periodically during treatment. Evaluate the risks and benefits in patients with known renal impairment or taking nephrotoxic drugs; monitor renal function. Discontinue ZALDYON if renal function deteriorates. (5.1, 7.1, 8.6)
- Mesalamine-induced Acute Intolerance Syndrome: Symptoms may be difficult to distinguish from an ulcerative colitis exacerbation; monitor for worsening symptoms; discontinue if acute intolerance syndrome suspected. (5.2)
- Hypersensitivity Reactions, including Myocarditis and Pericarditis: Evaluate patients immediately and discontinue if a hypersensitivity reaction is suspected. (5.3)
- Hepatic Failure: Evaluate the risks and benefits in patients with known liver impairment. (5.4)
- Severe Cutaneous Adverse Reactions:Discontinue at the first signs or symptoms of severe cutaneous adverse reactions or other signs of hypersensitivity and consider further evaluation. (5.5)
- Photosensitivity:Advise patients with pre-existing skin conditions to avoid sun exposure, wear protective clothing, and use a broad-spectrum sunscreen when outdoors. (5.6)
- Nephrolithiasis:Mesalamine-containing stones are undetectable by standard radiography or computed tomography (CT). Ensure adequate hydration during treatment. (5.7)
- Interference with Laboratory Tests:Use of mesalamine may lead to spuriously elevated test results when measuring urinary normetanephrine by liquid chromatography with electrochemical detection. (5.9)
Adverse Reactions/Side Effects
- The most common adverse reactions (≥ 2%) are headache, nausea, nasopharyngitis, abdominal pain, and worsening of ulcerative colitis (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Zydus Pharmaceuticals (USA) Inc. at 1-877-993-8779, or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
Use In Specific Populations
Geriatric Patients: Increased risk of blood dyscrasias; monitor complete blood cell counts and platelet counts (8.5)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 8/2023
Full Prescribing Information
2. Zaldyon Dosage and Administration
2.1 Important Administration Instructions
- Do not substitute one ZALDYON 800 mg tablet for two mesalamine delayed-release 400 mg oral products [see Clinical Pharmacology (12.3)].
- Evaluate renal function prior to initiation of ZALDYON.
- Take ZALDYON tablets on an empty stomach, at least 1 hour before and 2 hours after a meal [see Clinical Pharmacology (12.3)] .
- Swallow ZALDYON tablets whole. Do not cut, break or chew the tablets.
- Drink an adequate amount of fluids [see Warnings and Precautions (5.7)].
- Intact, partially intact, and/or tablet shells have been reported in the stool; Instruct patients to contact their healthcare provider if this occurs repeatedly.
- Protect ZALDYON tablets from moisture. Close the container tightly and leave desiccant pouches in the bottle along with the tablets.
5. Warnings and Precautions
5.1 Renal Impairment
Renal impairment, including minimal change disease, acute and chronic interstitial nephritis, and, rarely, renal failure, has been reported in patients taking products such as mesalamine delayed-release tablets that contain or are converted to mesalamine [see Adverse Reactions (6.2)]. In animal studies, the kidney was the principal organ of mesalamine toxicity [see Adverse Reactions (6.2), Nonclinical Toxicology (13.2)].
Evaluate renal function prior to initiation of mesalamine delayed-release tablets and periodically while on therapy. Evaluate the risks and benefits of using mesalamine delayed-release tablets in patients with known renal impairment or history of renal disease or taking concomitant nephrotoxic drugs. Discontinue ZALDYON if renal function deteriorates while on therapy [see Drug Interactions (7.1), Use in Specific Populations (8.6)].
5.2 Mesalamine-Induced Acute Intolerance Syndrome
Mesalamine has been associated with an acute intolerance syndrome that may be difficult to distinguish from an exacerbation of ulcerative colitis. Exacerbation of the symptoms of colitis has been reported in 2.3% of mesalamine-treated patients in controlled clinical trials. This acute reaction, characterized by cramping, abdominal pain, bloody diarrhea, and occasionally by fever, headache, malaise, pruritus, rash, and conjunctivitis, has been reported after the initiation of mesalamine delayed-release tablets as well as other mesalamine products. Symptoms usually abate when mesalamine delayed-release tablets are discontinued. Monitor patients for worsening of these symptoms while on treatment. If acute intolerance syndrome is suspected, promptly discontinue treatment with mesalamine delayed-release tablets.
5.3 Hypersensitivity Reactions
Hypersensitivity reactions have been reported in patients taking sulfasalazine. Some patients may have a similar reaction to mesalamine delayed-release tablets or to other compounds that contain or are converted to mesalamine.
As with sulfasalazine, mesalamine-induced hypersensitivity reactions may present as internal organ involvement, including myocarditis, pericarditis, nephritis, hepatitis, pneumonitis, and hematologic abnormalities. Evaluate patients immediately if signs or symptoms of a hypersensitivity reaction are present. Discontinue mesalamine delayed-release tablets if an alternative etiology for the signs or symptoms cannot be established.
5.4 Hepatic Failure
There have been reports of hepatic failure in patients with pre-existing liver disease who have been administered mesalamine. Evaluate the risks and benefits of using mesalamine delayed-release tablets in patients with known liver impairment.
5.5 Severe Cutaneous Adverse Reactions
Severe cutaneous adverse reactions including Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN), drug reaction with eosinophilia and systemic symptoms (DRESS), and acute generalized exanthematous pustulosis (AGEP) have been reported with use of mesalamine [see Adverse Reactions (6.2)]. Discontinue mesalamine delayed-release tablets at the first appearance of signs or symptoms of severe cutaneous adverse reactions, or other signs of hypersensitivity and consider further evaluation.
5.6 Photosensitivity
Patients treated with mesalamine or sulfasalazine who have pre-existing skin conditions such as atopic dermatitis and atopic eczema have reported more severe photosensitivity reactions. Advise patients to avoid sun exposure, wear protective clothing, and use a broad-spectrum sunscreen when outdoors.
5.7 Nephrolithiasis
Cases of nephrolithiasis have been reported with the use of mesalamine, including stones of 100% mesalamine content. Mesalamine-containing stones are radiotransparent and undetectable by standard radiography or computed tomography (CT). Ensure adequate fluid intake during treatment with mesalamine delayed-release tablets.
5.9 Interference with Laboratory Tests
Use of mesalamine delayed-release tablets may lead to spuriously elevated test results when measuring urinary normetanephrine by liquid chromatography with electrochemical detection because of the similarity in the chromatograms of normetanephrine and the main metabolite of mesalamine, N-acetyl-5-aminosalicylic acid (N-Ac-5-ASA). Consider an alternative, selective assay for normetanephrine.
6. Adverse Reactions/Side Effects
The following serious or clinically significant adverse described elsewhere in labeling are:
- Renal Impairment [see Warnings and Precautions (5.1)]
- Mesalamine-Induced Acute Intolerance Syndrome [see Warnings and Precautions (5.2)]
- Hypersensitivity Reactions [see Warnings and Precautions (5.3)]
- Hepatic Failure [see Warnings and Precautions (5.4)]
- Severe Cutaneous Adverse Reactions [see Warnings and Precautions (5.5)]
- Photosensitivity [see Warnings and Precautions (5.6)]
- Nephrolithiasis [see Warnings and Precautions (5.7)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Mesalamine has been evaluated in 896 patients with ulcerative colitis in controlled studies. Three six-week, active-controlled studies were conducted comparing mesalamine 4.8 grams per day with mesalamine-delayed release tablets 2.4 grams per day in patients with mildly to moderately active ulcerative colitis. In these studies, 727 patients were dosed with mesalamine delayed-release tablets and 732 patients were dosed with mesalamine delayed-release tablets, 400 mg.
The most common reactions reported in the mesalamine group were headache (4.7%), nausea (2.8%), nasopharyngitis (2.5%), abdominal pain (2.3%), diarrhea (1.7%), and dyspepsia (1.7%); Table 1 enumerates adverse reactions that occurred in the three studies. The most common reactions in patients with moderately active ulcerative colitis (602 patients dosed with mesalamine delayed-release tablet and 618 patients dosed with the mesalamine delayed-release tablet, 400 mg) were the same as all treated patients.
Discontinuations due to adverse reactions occurred in 3.9% of patients in the mesalamine delayed-release tablet, 800 mg group and in 4.2% of patients in the mesalamine delayed-release tablet, 400 mg comparator group. The most common cause for discontinuation was gastrointestinal symptoms associated with ulcerative colitis.
Serious adverse reactions occurred in 0.8% of patients in the mesalamine delayed-release tablet, 800 mg group and in 1.8% of patients in the mesalamine delayed-release tablet, 400 mg comparator group. The majority involved the gastrointestinal system.
|
N = number of patients within specified treatment group |
||
|
Percent = percentage of patients in category and treatment group |
||
| Adverse Reaction
| Mesalamine Delayed-Release Tablets
2.4 grams per day (400 mg Tablet) (N = 732) | Mesalamine Delayed-Release Tablets
4.8 grams per day (800 mg Tablet) (N = 727) |
| Headache | 4.9 % | 4.7 % |
| Nausea | 2.9 % | 2.8 % |
| Nasopharyngitis | 1.4 % | 2.5 % |
| Abdominal pain | 2.3 % | 2.3 % |
| Diarrhea | 1.9 % | 1.7 % |
| Dyspepsia | 0.8 % | 1.7 % |
| Vomiting | 1.6 % | 1.4 % |
| Flatulence | 0.7 % | 1.2 % |
| Influenza | 1.2 % | 1 % |
| Pyrexia | 1.2 % | 0.7 % |
| Cough | 1.4 % | 0.3 % |
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of mesalamine delayed-release tablets or other mesalamine-containing products or products that are metabolized to mesalamine. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Body as a Whole
Facial edema, edema, peripheral edema, asthenia, chills, infection, malaise, pain, neck pain, chest pain, back pain, abdominal enlargement, lupus-like syndrome, drug fever (rare).
Cardiovascular
Pericarditis (rare) and myocarditis (rare) [see Warnings and Precautions (5.3)], pericardial effusion, vasodilation, migraine.
Endocrine: Nephrogenic diabetes insipidus.
Gastrointestinal
Dry mouth, stomatitis, oral ulcers, anorexia, increased appetite, eructation, pancreatitis, cholecystitis, gastritis, gastroenteritis, gastrointestinal bleeding, perforated peptic ulcer (rare), constipation, hemorrhoids, rectal hemorrhage, bloody diarrhea, tenesmus, stool abnormality.
Hepatic
There have been rare reports of hepatotoxicity, including jaundice, cholestatic jaundice, hepatitis, and possible hepatocellular damage including liver necrosis and liver failure. Some of these cases were fatal. Asymptomatic elevations of liver enzymes which usually resolve during continued use or with discontinuation of the drug have also been reported. One case of Kawasaki-like syndrome, that included changes in liver enzymes, was also reported [see Warnings and Precautions (5.4)].
Hematologic
Agranulocytosis (rare), aplastic anemia (rare), anemia, thrombocytopenia, leukopenia, eosinophilia, lymphadenopathy.
Musculoskeletal
Gout, rheumatoid arthritis, arthritis, arthralgia, joint disorder, myalgia, hypertonia.
Neurological/Psychiatric
Anxiety, depression, somnolence, insomnia, nervousness, confusion, emotional lability, dizziness, vertigo, tremor, paresthesia, hyperesthesia, peripheral neuropathy (rare), Guillain-Barre syndrome (rare), transverse myelitis (rare) and intracranial hypertension.
Respiratory/Pulmonary
Sinusitis, rhinitis, pharyngitis, asthma exacerbation, pleuritis/pleurisy, bronchitis, eosinophilic pneumonia, interstitial pneumonitis.
Skin
Alopecia, psoriasis (rare), pyoderma gangrenosum (rare), erythema nodosum, acne, dry skin, sweating, pruritus, urticaria, rash, SJS/TEN, DRESS, and AGEP [see Warnings and Precautions (5.5)].
Special Senses
Ear pain, tinnitus, ear congestion, ear disorder, conjunctivitis, eye pain, blurred vision, vision abnormality, taste perversion.
Renal/Urogenital
Renal failure (rare), interstitial nephritis, minimal change disease, nephrolithiasis [see Warnings and Precautions (5.1), (5.7)], dysuria, urinary frequency and urgency, hematuria, epididymitis, decreased libido, dysmenorrhea, menorrhagia. Urine discoloration occurring ex-vivo caused by contact of mesalamine, including inactive metabolite, with surfaces or water treated with hypochlorite containing bleach.
Laboratory Abnormalities
Elevated AST (SGOT) or ALT (SGPT), elevated alkaline phosphatase, elevated GGT, elevated LDH, elevated bilirubin, elevated serum creatinine and BUN.
7. Drug Interactions
7.1 Nephrotoxic Agents, Including Non-Steroidal Anti-Inflammatory Drugs
The concurrent use of mesalamine with known nephrotoxic agents, including nonsteroidal anti-inflammatory drugs (NSAIDs) may increase the risk of nephrotoxicity. Monitor patients taking nephrotoxic drugs for changes in renal function and mesalamine-related adverse reactions [see Warnings and Precautions (5.1)].
7.2 Azathioprine or 6-Mercaptopurine
The concurrent use of mesalamine with azathioprine or 6-mercaptopurine and/or other drugs known to cause myelotoxicity may increase the risk for blood disorders, bone marrow failure, and associated complications. If concomitant use of ZALDYON and azathioprine or 6-mercaptopurine cannot be avoided, monitor blood tests, including complete blood cell counts and platelet counts.
7.3 Interference With Urinary Normetanephrine Measurements
Use of ZALDYON may lead to spuriously elevated test results when measuring urinary normetanephrine by liquid chromatography with electrochemical detection [see Warnings and Precautions (5.9)]. Consider an alternative, selective assay for normetanephrine.
8. Use In Specific Populations
8.1 Pregnancy
Limited published data on mesalamine use in pregnant women are insufficient to inform a drug-associated risk. No fetal harm was observed in animal reproduction studies of mesalamine in rats and rabbits at oral doses approximately 0.97 times (rat) and 1.95 times (rabbit) the recommended human dose [see Data].
The estimated background risk of major birth defects and miscarriage for the indicated populations is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Data
Animal Data
Reproduction studies with mesalamine were performed during organogenesis in rats and rabbits at oral doses up to 480 mg/kg/day. There was no evidence of harm to the fetus. These mesalamine doses were about 0.97 times (rat) and 1.95 times (rabbit) the recommended human dose of 4.8 grams per day, based on body surface area.
8.2 Lactation
Mesalamine and its N-acetyl metabolite are present in human milk in undetectable to small amounts [see Data]. There are limited reports of diarrhea in breastfed infants.
There is no information on the effects of the drug on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for mesalamine and any potential adverse effects on the breastfed infant from the drug or from the underlying maternal condition.
Clinical Considerations
Monitor breastfed infants for diarrhea.
Data
Human Data
In published lactation studies, maternal mesalamine doses from various oral and rectal formulations and products ranged from 500 mg to 3 g daily. The concentration of mesalamine in milk ranged from non-detectable to 0.11 mg/L. The concentration of the N-acetyl-5-aminosalicylic acid metabolite ranged from 5 to 18.1 mg/L. Based on these concentrations, estimated infant daily dosages for an exclusively breastfed infant are 0 to 0.017 mg/kg/day of mesalamine and 0.75 to 2.72 mg/kg/day of N-acetyl-5-aminosalicylic acid.
8.4 Pediatric Use
Safety and effectiveness of mesalamine in pediatric patients have not been established. See the prescribing information for other approved mesalamine products for the safety and effectiveness of these products in pediatric patients.
8.5 Geriatric Use
Clinical studies of mesalamine delayed-release tablets did not include sufficient numbers of patients aged 65 years and over to determine whether they respond differently than younger patients. Reports from uncontrolled clinical studies and postmarketing reporting systems suggested a higher incidence of blood dyscrasias (agranulocytosis, neutropenia, and pancytopenia) in patients who were 65 years or older compared to younger patients taking mesalamine containing products such as mesalamine delayed-release tablets. Monitor complete blood cell counts and platelet counts in elderly patients during therapy with mesalamine delayed-release tablets.
In general, consider the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy in elderly patients when prescribing mesalamine delayed-release tablets [see Use in Specific Populations (8.6)].
8.6 Renal Impairment
Mesalamine is known to be substantially excreted by the kidney, and the risk of adverse reactions may be greater in patients with impaired renal function. Evaluate renal function in all patients prior to initiation and periodically while on mesalamine delayed-release tablets therapy. Monitor patients with known renal impairment or history of renal disease or taking nephrotoxic drugs for decreased renal function and mesalamine-related adverse reactions. Discontinue ZALDYON if renal function deteriorates while on therapy [see Warnings and Precautions (5.1), Drug Interactions (7.1) and Adverse Reactions (6.2)].
10. Overdosage
ZALDYON is an aminosalicylate, and symptoms of salicylate toxicity include nausea, vomiting and abdominal pain, tachypnea, hyperpnea, tinnitus, and neurologic symptoms (headache, dizziness, confusion, seizures). Severe salicylate intoxication may lead to electrolyte and blood pH imbalance and potentially to other organ (e.g., renal and liver) involvement. There is no specific antidote for mesalamine overdose; however, conventional therapy for salicylate toxicity may be beneficial in the event of acute overdosage and may include gastrointestinal tract decontamination to prevent of further absorption. Correct fluid and electrolyte imbalance by the administration of appropriate intravenous therapy and maintain adequate renal function.
ZALDYON is a pH dependent delayed-release product and this factor should be considered when treating a suspected overdose.
11. Zaldyon Description
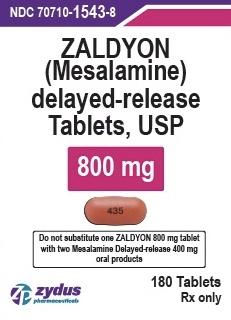
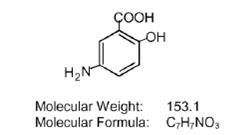
Each ZALDYON delayed-release tablet for oral administration contains 800 mg of mesalamine USP, an aminosalicylate. Mesalamine, USP is light tan to pink colored, needle-shaped crystals. Color may darken on exposure to air. It is odorless or may have a slight characteristic odor, slightly soluble in water; very slightly soluble in methanol, in dehydrated alcohol, and in acetone; practically insoluble in n-butyl alcohol, in chloroform, in ether, in ethyl acetate, in n-hexane, in methylene chloride, and in n-propyl alcohol and soluble in dilute hydrochloric acid and in dilute alkali hydroxides. ZALDYON have single layered coating consisting of an acrylic based resin Eudragit S (methacrylic acid copolymer B, NF), which dissolves at pH 7 or greater, releasing mesalamine for topical anti-inflammatory action in the colon. Mesalamine (also referred to as 5-aminosalicylic acid or 5-ASA) has the chemical name 5-amino-2-hydroxybenzoic acid and its structural formula is:
Each ZALDYON (mesalamine) delayed-release tablet contains 800 mg of mesalamine. In addition, each tablet contains the following inactive ingredients: acetyltributyl citrate, colloidal silicone dioxide, ferric oxide red, magnesium stearate, methacrylic acid copolymer type B, microcrystalline cellulose, povidone, sodium starch glycolate, talc and titanium dioxide. The tablet is printed with opacode black S-1-17823 which contains following ingredients: ammonium hydroxide, butyl alcohol, ferrosoferric oxide, isopropyl alcohol, propylene glycol and shellac.
12. Zaldyon - Clinical Pharmacology
12.1 Mechanism of Action
The mechanism of action of mesalamine is not fully understood, but appears to be a topical anti-inflammatory effect on colonic epithelial cells. Mucosal production of arachidonic acid metabolites, both through the cyclooxygenase pathways, that is, prostanoids, and through the lipoxygenase pathways, that is, leukotrienes and hydroxyeicosatetraenoic acids, is increased in patients with ulcerative colitis, and it is possible that mesalamine diminishes inflammation by blocking cyclooxygenase and inhibiting prostaglandin production in the colon.
12.3 Pharmacokinetics
Plasma concentrations of mesalamine (5-aminosalicylic acid; 5-ASA) and its metabolite, N-acetyl-5-aminosalicylic acid (N-Ac-5-ASA) are highly variable following administration of ZALDYON tablets. Following single dose oral administration of ZALDYON 800 mg tablet in healthy subjects (N = 139) under fasted conditions, the mean Cmax, AUC8-48h and AUC0-tldc values were 208 ng/mL, 2296 ng.h/mL, and 2533 ng.h/mL, respectively. The median [range] Tmax for mesalamine following administration of ZALDYON 800 mg tablet was approximately 24 hours [4 to 72 hours], reflecting the delayed-release characteristics of the formulation.
Based on cumulative urinary recovery of mesalamine and N-Ac-5-ASA from single dose studies in healthy subjects, approximately 20% of the orally administered mesalamine in ZALDYON is systemically absorbed.
Food Effect: A high calorie (800 to 1000 calories), high fat (approximately 50 % of total caloric content) meal increased mesalamine Cmax by 2.4-fold and mesalamine systemic exposure (AUC8-48 and AUC0-tldc) by 2.8-fold; the median lag-time increased by 8 hours and median tmax by 6 hours (from 24 to 30 hours) [see Dosage and Administration (2.1)].
Comparative exposure between one ZALDYON 800 mg tablet and two mesalamine delayed-release 400 mg oral products is unknown [see Dosage and Administration (2.1)].
Elimination
Metabolism
The absorbed mesalamine is acetylated in the gut mucosal wall and by the liver to N-Ac- 5-ASA.
Excretion
Absorbed mesalamine is excreted mainly by the kidneys as N-acetyl-5-aminosalicylic acid. Unabsorbed mesalamine is excreted in feces.
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Dietary mesalamine was not carcinogenic in rats at doses as high as 480 mg/kg/day, or in mice at 2000 mg/kg/day. These doses are approximately 0.97 and 2.0 times the 4.8 grams per day ZALDYON dose (based on body surface area). Mesalamine was not genotoxic in the Ames test, the Chinese hamster ovary cell chromosomal aberration assay, and the mouse micronucleus test. Mesalamine, at oral doses up to 480 mg/kg/day (about 0.97 times the recommended human treatment dose based on body surface area), was found to have no effect on fertility or reproductive performance of male and female rats.
13.2 Animal Toxicology and/or Pharmacology
In animal studies (rats, mice, dogs), the kidney was the principal organ for toxicity. (In the following, comparisons of animal dosing to recommended human dosing are based on body surface area and a 4.8 grams per day dose for a 60 kg person).
Mesalamine causes renal papillary necrosis in rats at single doses of approximately 750 mg/kg to 1000 mg/kg (1.5 to 2.0 times the recommended human dose). Doses of 170 and 360 mg/kg/day (about 0.3 and 0.73 times the recommended human dose) given to rats for six months produced papillary necrosis, papillary edema, tubular degeneration, tubular mineralization, and urothelial hyperplasia.
In mice, oral doses of 4000 mg/kg/day (approximately 4.1 times the recommended human dose) for three months produced tubular nephrosis, multifocal/diffuse tubulo-interstitial inflammation, and multifocal/diffuse papillary necrosis.
In dogs, single doses of 6000 mg (approximately 6.25 times the recommended human dose) of delayed-release mesalamine tablets resulted in renal papillary necrosis but were not fatal. Renal changes have occurred in dogs given chronic administration of mesalamine at doses of 80 mg/kg/day (0.5 times the recommended human dose).
14. Clinical Studies
The efficacy of mesalamine delayed-release tablets at 4.8 grams per day was studied in a six-week, randomized, double-blind, active-controlled study in 772 patients with moderately active ulcerative colitis (UC). Moderately active UC was defined as a Physician's Global Assessment (PGA) score of 2; the PGA is a four-point scale (0 to 3) that encompasses the clinical assessments of rectal bleeding, stool frequency, and sigmoidoscopy findings.
Patients were randomized 1:1 to the mesalamine delayed-release tablets 4.8 grams per day group (two mesalamine delayed-release tablets three times a day) or the mesalamine delayed-release 2.4 grams per day group (two mesalamine delayed-release 400 mg tablets three times a day).
Patients characteristically had a history of previous use of oral 5-ASAs (86%), steroids (41%), and rectal therapies (49%), and demonstrated clinical symptoms of three or more stools over normal per day (87%) and obvious blood in the stool most or all of the time (70%). The study population was primarily Caucasian (97%), had a mean age of 43 years (8% aged 65 years or older), and included slightly more males (56%) than females (44%).
The primary endpoint was treatment success defined as improvement from baseline to Week 6 based on the PGA. Treatment success rates were similar in the two groups: 70% in the mesalamine group and 66% in the mesalamine delayed-release 400 mg tablets group (difference: 5%; 95% CI: [-1.9%, 11.2%]).
A second controlled study supported the efficacy of mesalamine at 4.8 grams per day. Treatment success was 72% in patients with moderately active UC treated with mesalamine.
16. How is Zaldyon supplied
ZALDYON (mesalamine) delayed-release tablets, USP 800 mg are reddish-brown colored, capsule-shaped, biconvex, enteric coated tablets, imprinted with "435" on one side and plain on other side and are supplied as follows:
NDC 70710-1543-8 in bottles of 180 tablets
NDC 70710-1543-4 in cartons of 100 tablets (10 x 10 unit-dose)
Storage
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
Store and dispense in the original bottle, protect from moisture, and keep the bottle tightly closed. Do not remove desiccant pouch (silica gel) from bottle.
17. Patient Counseling Information
Administration [see Dosage and Administration (2.1)]
- Inform patients that if they are switching from a previous oral mesalamine therapy to ZALDYON to discontinue their previous oral mesalamine therapy and follow the dosing instructions for ZALDYON. One ZALDYON 800 mg tablet is not substitutable for two mesalamine delayed-release 400 mg oral products.
- Inform patients to take ZALDYON tablets on an empty stomach, at least 1 hour before and 2 hours after a meal.
- Instruct patients to swallow the ZALDYON tablets whole, taking care not to break, cut, or chew the tablets, because the coating is an important part of the delayed-release formulation.
- Drink an adequate amount of fluids.
- Inform patients that intact, partially intact, and/or tablet shells have been reported in the stool. Instruct patients to contact their healthcare provider if this occurs repeatedly.
- Instruct patients to protect ZALDYON tablets from moisture. Instruct patients to close the container tightly and to leave desiccant pouches in the bottle along with the tablets.
- Inform patients that ZALDYON may decrease their renal function, especially if they have known renal impairment or are taking nephrotoxic drugs, including NSAIDS and periodic monitoring of renal function will be performed while they are on therapy. Advise patients to complete all blood tests ordered by their healthcare provider [see Warnings and Precautions (5.1), Drug Interactions (7.1)] .
Mesalamine-Induced Acute Intolerance Syndrome and Other Hypersensitivity Reactions
- Inform patients of the signs and symptoms of hypersensitivity reactions. Instruct patients to stop taking ZALDYON and report to their healthcare provider if they experience new or worsening symptoms of Acute Intolerance Syndrome (cramping, abdominal pain, bloody diarrhea, fever, headache, malaise, conjunctivitis and rash) or other symptoms suggestive of mesalamine-induced hypersensitivity [see Warnings and Precautions (5.2, 5.3)].
- Inform patients with known liver disease of the signs and symptoms of worsening liver function and advise them to report to their healthcare provider if they experience such signs or symptoms [see Warnings and Precautions (5.4)] .
Severe Cutaneous Adverse Reactions
- Inform patients of the signs and symptoms of severe cutaneous adverse reactions. Instruct patients to stop taking mesalamine delayed-release tablets and report to their healthcare provider at first appearance of a severe cutaneous adverse reaction or other sign of hypersensitivity [see Warnings and Precautions (5.5)] .
- Advise patients with pre-existing skin conditions to avoid sun exposure, wear protective clothing, and use a broad-spectrum sunscreen when outdoors [see Warnings and Precautions (5.6)].
- Instruct patients to maintain an adequate fluid intake in order to minimize the risk of kidney stone formation and to contact their healthcare provider if they experience signs or symptoms of a kidney stone (e.g., severe side or back pain, blood in the urine) [see Warnings and Precautions (5.7)].
- Inform elderly patients and those taking azathioprine or 6-mercaptopurine of the risk for blood disorders and the need for periodic monitoring of complete blood cell counts and platelet counts while on therapy. Advise patients to complete all blood tests ordered by their physician [see Drug Interactions (7.2), Use in Specific Populations (8.5)] .
- Advise patients that urine may become discolored reddish-brown while taking Mesalamine Delayed-Release Tablets when it comes in contact with surfaces or water treated with hypochlorite-containing bleach. If discolored urine is observed, advise patients to observe their urine flow. Report to the healthcare provider only if urine is discolored on leaving the body, before contact with any surface or water (e.g., in the toilet).
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
| ZALDYON
mesalamine tablet, delayed release |
||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||
| Labeler - Zydus Pharmaceuticals USA Inc. (156861945) |
| Registrant - Zydus Pharmaceuticals USA Inc. (156861945) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Zydus Lifesciences Limited | 918596198 | ANALYSIS(70710-1543) , MANUFACTURE(70710-1543) | |
Frequently asked questions
More about Zaldyon (mesalamine)
- Check interactions
- Compare alternatives
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: 5-aminosalicylates
- Breastfeeding
Professional resources
Other brands
Lialda, Pentasa, Apriso, Asacol, ... +4 more