Inomax: Package Insert / Prescribing Info
Package insert / product label
Generic name: nitric oxide
Dosage form: gas, for inhalation
Drug class: Miscellaneous respiratory agents
Medically reviewed by Drugs.com. Last updated on Dec 15, 2024.
On This Page
- Indications and Usage
- Dosage and Administration
- Dosage Forms and Strengths
- Contraindications
- Warnings and Precautions
- Adverse Reactions/Side Effects
- Drug Interactions
- Use In Specific Populations
- Overdosage
- Description
- Clinical Pharmacology
- Nonclinical Toxicology
- Clinical Studies
- How Supplied/Storage and Handling
- Storage and Handling
Highlights of Prescribing Information
INOMAX® (nitric oxide) gas, for inhalation
Initial U.S. Approval: 1999
Indications and Usage for Inomax
INOmax is a vasodilator indicated to improve oxygenation and reduce the need for extracorporeal membrane oxygenation in term and near-term (>34 weeks gestation) neonates with hypoxic respiratory failure associated with clinical or echocardiographic evidence of pulmonary hypertension in conjunction with ventilatory support and other appropriate agents. (1)
Inomax Dosage and Administration
The recommended dose is 20 ppm, maintained for up to 14 days or until the underlying oxygen desaturation has resolved (2.1).
Doses greater than 20 ppm are not recommended (2.1, 5.2)
Administration:
Dosage Forms and Strengths
INOmax (nitric oxide) is a gas available in 800 and 4,880 ppm concentrations (3).
Contraindications
Neonates dependent on right-to-left shunting of blood (4).
Warnings and Precautions
Rebound: Abrupt discontinuation of INOmax may lead to worsening oxygenation and increasing pulmonary artery pressure (5.1).
Methemoglobinemia: Methemoglobin increases with the dose of nitric oxide; following discontinuation or reduction of nitric oxide, methemoglobin levels return to baseline over a period of hours (5.2).
Elevated NO2 Levels: Monitor NO2 levels (5.3).
Heart Failure: In patients with pre-existing left ventricular dysfunction, INOmax may increase pulmonary capillary wedge pressure leading to pulmonary edema (5.4).
Adverse Reactions/Side Effects
The most common adverse reaction is hypotension. (6).
To report SUSPECTED ADVERSE REACTIONS, contact INO Therapeutics at 1-877-566-9466 and http://www.inomax.com/ or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
Nitric oxide donor compounds may increase the risk of developing methemoglobinemia (7).
Revised: 4/2023
Full Prescribing Information
1. Indications and Usage for Inomax
INOmax® is indicated to improve oxygenation and reduce the need for extracorporeal membrane oxygenation in term and near-term (>34 weeks gestation) neonates with hypoxic respiratory failure associated with clinical or echocardiographic evidence of pulmonary hypertension in conjunction with ventilatory support and other appropriate agents.
2. Inomax Dosage and Administration
2.1 Dosage
Term and near-term neonates with hypoxic respiratory failure
The recommended dose of INOmax is 20 ppm. Maintain treatment up to 14 days or until the underlying oxygen desaturation has resolved and the neonate is ready to be weaned from INOmax therapy.
Doses greater than 20 ppm are not recommended [see Warnings and Precautions (5.2)].
2.2 Administration
Nitric Oxide Delivery Systems
INOmax must be administered using a calibrated, FDA-cleared Nitric Oxide Delivery System (NODS). There are various FDA-cleared NODS; refer to the NODS labeling to determine which NODS to use with this drug product and for needed information on training and technical support for users of this drug product with the NODS.
When utilizing a nitric oxide delivery system specifically cleared for use in the MRI suite (e.g., the INOmax DSIR® Plus MRI) only use INOmax MR conditional cylinders at 100 gauss or less [see How Supplied/Storage and Handling (16)].
Keep available a backup battery power supply and an independent reserve nitric oxide delivery system to address power and system failures.
Monitoring
Measure methemoglobin within 4-8 hours after initiation of treatment with INOmax and periodically throughout treatment [see Warnings and Precautions (5.2)].
Monitor for PaO2 and inspired NO2 during INOmax administration [see Warnings and Precautions (5.3)].
Weaning and Discontinuation
Avoid abrupt discontinuation of INOmax [see Warnings and Precautions (5.1)]. To wean INOmax, downtitrate in several steps, pausing several hours at each step to monitor for hypoxemia.
3. Dosage Forms and Strengths
INOmax (nitric oxide) gas is available in 800 and 4,880 ppm concentrations.
4. Contraindications
INOmax is contraindicated in neonates dependent on right-to-left shunting of blood.
5. Warnings and Precautions
5.1 Rebound Pulmonary Hypertension Syndrome following Abrupt Discontinuation
Wean from INOmax [see Dosage and Administration (2.2)]. Abrupt discontinuation of INOmax may lead to worsening oxygenation and increasing pulmonary artery pressure, i.e., Rebound Pulmonary Hypertension Syndrome. Signs and symptoms of Rebound Pulmonary Hypertension Syndrome include hypoxemia, systemic hypotension, bradycardia, and decreased cardiac output. If Rebound Pulmonary Hypertension occurs, reinstate INOmax therapy immediately.
5.2 Hypoxemia from Methemoglobinemia
Nitric oxide combines with hemoglobin to form methemoglobin, which does not transport oxygen. Methemoglobin levels increase with the dose of INOmax; it can take 8 hours or more before steady-state methemoglobin levels are attained. Monitor methemoglobin and adjust the dose of INOmax to optimize oxygenation.
If methemoglobin levels do not resolve with decrease in dose or discontinuation of INOmax, additional therapy may be warranted to treat methemoglobinemia [see Overdosage (10)].
5.3 Airway Injury from Nitrogen Dioxide
Nitrogen dioxide (NO2) forms in gas mixtures containing NO and O2. Nitrogen dioxide may cause airway inflammation and damage to lung tissues.
If there is an unexpected change in NO2 concentration, or if the NO2 concentration reaches 3 ppm when measured in the breathing circuit, then the delivery system should be assessed in accordance with the Nitric Oxide Delivery System O&M Manual troubleshooting section, and the NO2 analyzer should be recalibrated. The dose of INOmax and/or FiO2 should be adjusted as appropriate.
5.4 Worsening Heart Failure
Patients with left ventricular dysfunction treated with INOmax may experience pulmonary edema, increased pulmonary capillary wedge pressure, worsening of left ventricular dysfunction, systemic hypotension, bradycardia and cardiac arrest. Discontinue INOmax while providing symptomatic care.
6. Adverse Reactions/Side Effects
The following adverse reactions are discussed elsewhere in the label;
Hypoxemia [see Warnings and Precautions (5.2)]
Worsening Heart Failure [see Warnings and Precautions (5.4)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. The adverse reaction information from the clinical studies does, however, provide a basis for identifying the adverse events that appear to be related to drug use and for approximating rates.
Controlled studies have included 325 patients on INOmax doses of 5 to 80 ppm and 251 patients on placebo. Total mortality in the pooled trials was 11% on placebo and 9% on INOmax, a result adequate to exclude INOmax mortality being more than 40% worse than placebo.
In both the NINOS and CINRGI studies, the duration of hospitalization was similar in INOmax and placebo-treated groups.
From all controlled studies, at least 6 months of follow-up is available for 278 patients who received INOmax and 212 patients who received placebo. Among these patients, there was no evidence of an adverse effect of treatment on the need for rehospitalization, special medical services, pulmonary disease, or neurological sequelae.
In the NINOS study, treatment groups were similar with respect to the incidence and severity of intracranial hemorrhage, Grade IV hemorrhage, periventricular leukomalacia, cerebral infarction, seizures requiring anticonvulsant therapy, pulmonary hemorrhage, or gastrointestinal hemorrhage.
In CINRGI, the only adverse reaction (>2% higher incidence on INOmax than on placebo) was hypotension (14% vs. 11%).
8. Use In Specific Populations
8.4 Pediatric Use
The safety and efficacy of nitric oxide for inhalation has been demonstrated in term and near-term neonates with hypoxic respiratory failure associated with evidence of pulmonary hypertension [see Clinical Studies (14.1)]. Additional studies conducted in premature neonates for the prevention of bronchopulmonary dysplasia have not demonstrated substantial evidence of efficacy [see Clinical Studies (14.3)]. No information about its effectiveness in other age populations is available.
10. Overdosage
Overdosage with INOmax is manifest by elevations in methemoglobin and pulmonary toxicities associated with inspired NO2. Elevated NO2 may cause acute lung injury. Elevations in methemoglobin reduce the oxygen delivery capacity of the circulation. In clinical studies, NO2 levels >3 ppm or methemoglobin levels >7% were treated by reducing the dose of, or discontinuing, INOmax.
Methemoglobinemia that does not resolve after reduction or discontinuation of therapy can be treated with intravenous vitamin C, intravenous methylene blue, or blood transfusion, based upon the clinical situation.
11. Inomax Description
INOmax (nitric oxide gas) is a drug administered by inhalation. Nitric oxide, the active substance in INOmax, is a pulmonary vasodilator. INOmax 800 ppm is a gaseous blend of nitric oxide (0.08%) and nitrogen (99.92%). INOmax 4,880™ ppm is a gaseous blend of nitric oxide (0.488%) and nitrogen (99.51%). INOmax 800 ppm is supplied in aluminum cylinders as a compressed gas under high pressure (2,000 pounds per square inch [psi]). INOmax 4,880 ppm is supplied in aluminum cylinders as a compressed gas under high pressure (3,000 psi).
The structural formula of nitric oxide (NO) is shown below:
12. Inomax - Clinical Pharmacology
12.1 Mechanism of Action
Nitric oxide relaxes vascular smooth muscle by binding to the heme moiety of cytosolic guanylate cyclase, activating guanylate cyclase and increasing intracellular levels of cyclic guanosine 3',5'-monophosphate, which then leads to vasodilation. When inhaled, nitric oxide selectively dilates the pulmonary vasculature, and because of efficient scavenging by hemoglobin, has minimal effect on the systemic vasculature.
INOmax appears to increase the partial pressure of arterial oxygen (PaO2) by dilating pulmonary vessels in better ventilated areas of the lung, redistributing pulmonary blood flow away from lung regions with low ventilation/perfusion (V/Q) ratios toward regions with normal ratios.
12.2 Pharmacodynamics
Effects on Pulmonary Vascular Tone in PPHN
Persistent pulmonary hypertension of the newborn (PPHN) occurs as a primary developmental defect or as a condition secondary to other diseases such as meconium aspiration syndrome (MAS), pneumonia, sepsis, hyaline membrane disease, congenital diaphragmatic hernia (CDH), and pulmonary hypoplasia. In these states, pulmonary vascular resistance (PVR) is high, which results in hypoxemia secondary to right-to-left shunting of blood through the patent ductus arteriosus and foramen ovale. In neonates with PPHN, INOmax improves oxygenation (as indicated by significant increases in PaO2).
Absorption and Distribution
Nitric oxide is absorbed systemically after inhalation. Most of it traverses the pulmonary capillary bed where it combines with hemoglobin that is 60% to 100% oxygen-saturated. At this level of oxygen saturation, nitric oxide combines predominantly with oxyhemoglobin to produce methemoglobin and nitrate. At low oxygen saturation, nitric oxide can combine with deoxyhemoglobin to transiently form nitrosylhemoglobin, which is converted to nitrogen oxides and methemoglobin upon exposure to oxygen. Within the pulmonary system, nitric oxide can combine with oxygen and water to produce nitrogen dioxide and nitrite, respectively, which interact with oxyhemoglobin to produce methemoglobin and nitrate. Thus, the end products of nitric oxide that enter the systemic circulation are predominantly methemoglobin and nitrate.
Metabolism
Methemoglobin disposition has been investigated as a function of time and nitric oxide exposure concentration in neonates with respiratory failure. The methemoglobin (MetHb) concentration-time profiles during the first 12 hours of exposure to 0, 5, 20, and 80 ppm INOmax are shown in Figure 1.
Figure 1: Methemoglobin Concentration-Time Profiles Neonates Inhaling 0, 5, 20 or 80 ppm INOmax
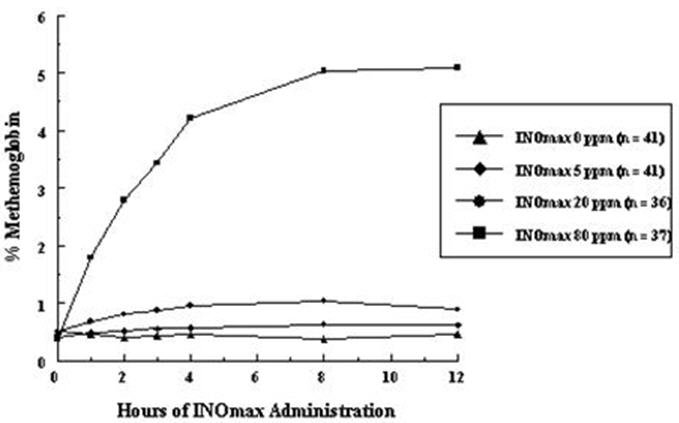
Methemoglobin concentrations increased during the first 8 hours of nitric oxide exposure. The mean methemoglobin level remained below 1% in the placebo group and in the 5 ppm and 20 ppm INOmax groups but reached approximately 5% in the 80 ppm INOmax group. Methemoglobin levels >7% were attained only in patients receiving 80 ppm, where they comprised 35% of the group. The average time to reach peak methemoglobin was 10 ± 9 (SD) hours (median, 8 hours) in these 13 patients, but one patient did not exceed 7% until 40 hours.
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
No evidence of a carcinogenic effect was apparent, at inhalation exposures up to the recommended dose (20 ppm), in rats for 20 hr/day for up to two years. Higher exposures have not been investigated.
Nitric oxide has demonstrated genotoxicity in Salmonella (Ames Test), human lymphocytes, and after in vivo exposure in rats. There are no animal or human studies to evaluate nitric oxide for effects on fertility.
14. Clinical Studies
14.1 Treatment of Hypoxic Respiratory Failure (HRF)
The efficacy of INOmax has been investigated in term and near-term newborns with hypoxic respiratory failure resulting from a variety of etiologies. Inhalation of INOmax reduces the oxygenation index (OI= mean airway pressure in cm H2O × fraction of inspired oxygen concentration [FiO2]× 100 divided by systemic arterial concentration in mm Hg [PaO2]) and increases PaO2 [see Clinical Pharmacology (12.1)].
NINOS Study
The Neonatal Inhaled Nitric Oxide Study (NINOS) was a double-blind, randomized, placebo-controlled, multicenter trial in 235 neonates with hypoxic respiratory failure. The objective of the study was to determine whether inhaled nitric oxide would reduce the occurrence of death and/or initiation of extracorporeal membrane oxygenation (ECMO) in a prospectively defined cohort of term or near-term neonates with hypoxic respiratory failure unresponsive to conventional therapy. Hypoxic respiratory failure was caused by meconium aspiration syndrome (MAS; 49%), pneumonia/sepsis (21%), idiopathic primary pulmonary hypertension of the newborn (PPHN; 17%), or respiratory distress syndrome (RDS; 11%). Infants ≤14 days of age (mean, 1.7 days) with a mean PaO2 of 46 mm Hg and a mean oxygenation index (OI) of 43 cm H2O / mm Hg were initially randomized to receive 100% O2 with (n=114) or without (n=121) 20 ppm nitric oxide for up to 14 days. Response to study drug was defined as a change from baseline in PaO2 30 minutes after starting treatment (full response = >20 mm Hg, partial = 10–20 mm Hg, no response = <10 mm Hg). Neonates with a less than full response were evaluated for a response to 80 ppm nitric oxide or control gas. The primary results from the NINOS study are presented in Table 1.
| Control (n=121) | NO (n=114) | P value | |
|---|---|---|---|
| Death or ECMO*,† | 77 (64%) | 52 (46%) | 0.006 |
| Death | 20 (17%) | 16 (14%) | 0.60 |
| ECMO | 66 (55%) | 44 (39%) | 0.014 |
Although the incidence of death by 120 days of age was similar in both groups (NO, 14%; control, 17%), significantly fewer infants in the nitric oxide group required ECMO compared with controls (39% vs. 55%, p = 0.014). The combined incidence of death and/or initiation of ECMO showed a significant advantage for the nitric oxide treated group (46% vs. 64%, p = 0.006). The nitric oxide group also had significantly greater increases in PaO2 and greater decreases in the OI and the alveolar-arterial oxygen gradient than the control group (p<0.001 for all parameters). Significantly more patients had at least a partial response to the initial administration of study drug in the nitric oxide group (66%) than the control group (26%, p<0.001). Of the 125 infants who did not respond to 20 ppm nitric oxide or control, similar percentages of NO-treated (18%) and control (20%) patients had at least a partial response to 80 ppm nitric oxide for inhalation or control drug, suggesting a lack of additional benefit for the higher dose of nitric oxide. No infant had study drug discontinued for toxicity. Inhaled nitric oxide had no detectable effect on mortality. The adverse events collected in the NINOS trial occurred at similar incidence rates in both treatment groups [see Adverse Reactions (6.1)]. Follow-up exams were performed at 18–24 months for the infants enrolled in this trial. In the infants with available follow-up, the two treatment groups were similar with respect to their mental, motor, audiologic, or neurologic evaluations.
CINRGI Study
This study was a double-blind, randomized, placebo-controlled, multicenter trial of 186 term and near-term neonates with pulmonary hypertension and hypoxic respiratory failure. The primary objective of the study was to determine whether INOmax would reduce the receipt of ECMO in these patients. Hypoxic respiratory failure was caused by MAS (35%), idiopathic PPHN (30%), pneumonia/sepsis (24%), or RDS (8%). Patients with a mean PaO2 of 54 mm Hg and a mean OI of 44 cm H2O / mm Hg were randomly assigned to receive either 20 ppm INOmax (n=97) or nitrogen gas (placebo; n=89) in addition to their ventilatory support. Patients who exhibited a PaO2 >60 mm Hg and a pH < 7.55 were weaned to 5 ppm INOmax or placebo. The primary results from the CINRGI study are presented in Table 2.
| Placebo | INOmax | P value | |
|---|---|---|---|
| ECMO*,† | 51/89 (57%) | 30/97 (31%) | <0.001 |
| Death | 5/89 (6%) | 3/97 (3%) | 0.48 |
Significantly fewer neonates in the INOmax group required ECMO compared to the control group (31% vs. 57%, p<0.001). While the number of deaths were similar in both groups (INOmax, 3%; placebo, 6%), the combined incidence of death and/or receipt of ECMO was decreased in the INOmax group (33% vs. 58%, p<0.001).
In addition, the INOmax group had significantly improved oxygenation as measured by PaO2, OI, and alveolar-arterial gradient (p<0.001 for all parameters). Of the 97 patients treated with INOmax, 2 (2%) were withdrawn from study drug due to methemoglobin levels >4%. The frequency and number of adverse events reported were similar in the two study groups [see Adverse Reactions (6.1)].
In clinical trials, reduction in the need for ECMO has not been demonstrated with the use of inhaled nitric oxide in neonates with congenital diaphragmatic hernia (CDH).
14.2 Ineffective in Adult Respiratory Distress Syndrome (ARDS)
In a randomized, double-blind, parallel, multicenter study, 385 patients with adult respiratory distress syndrome (ARDS) associated with pneumonia (46%), surgery (33%), multiple trauma (26%), aspiration (23%), pulmonary contusion (18%), and other causes, with PaO2/FiO2 <250 mm Hg despite optimal oxygenation and ventilation, received placebo (n=193) or INOmax (n=192), 5 ppm, for 4 hours to 28 days or until weaned because of improvements in oxygenation. Despite acute improvements in oxygenation, there was no effect of INOmax on the primary endpoint of days alive and off ventilator support. These results were consistent with outcome data from a smaller dose ranging study of nitric oxide (1.25 to 80 ppm). INOmax is not indicated for use in ARDS.
14.3 Ineffective in Prevention of Bronchopulmonary Dysplasia (BPD)
The safety and efficacy of INOmax for the prevention of chronic lung disease [bronchopulmonary dysplasia, (BPD)] in neonates ≤ 34 weeks gestational age requiring respiratory support has been studied in four large, multi-center, double-blind, placebo-controlled clinical trials in a total of 2,600 preterm infants. Of these, 1,290 received placebo, and 1,310 received inhaled nitric oxide at doses ranging from 5-20 ppm, for treatment periods of 7-24 days duration. The primary endpoint for these studies was alive and without BPD at 36 weeks postmenstrual age (PMA). The need for supplemental oxygen at 36 weeks PMA served as a surrogate endpoint for the presence of BPD. Overall, efficacy for the prevention of bronchopulmonary dysplasia in preterm infants was not established. There were no meaningful differences between treatment groups with regard to overall deaths, methemoglobin levels, or adverse events commonly observed in premature infants, including intraventricular hemorrhage, patent ductus arteriosus, pulmonary hemorrhage, and retinopathy of prematurity.
The use of INOmax for prevention of BPD in preterm neonates ≤ 34 weeks gestational age is not recommended.
16. How is Inomax supplied
INOmax (nitric oxide) is available in the following sizes:
| Size D | Portable aluminum cylinders containing 353 liters at STP of nitric oxide gas in 800 ppm concentration in nitrogen (delivered volume 344 liters) (NDC 64693-002-01) |
| Size 88 | Aluminum cylinders containing 1963 liters at STP of nitric oxide gas in 800 ppm concentration in nitrogen (delivered volume 1918 liters) (NDC 64693-002-02) |
| 0.4 liter | Portable aluminum cylinders containing 78 liters at STP of nitric oxide gas in 4,880 ppm concentration in nitrogen (delivered volume 70 liters) (NDC 64693-003-01) |
Store at 25°C (77°F) with excursions permitted between 15° to 30°C (59° to 86°F) [see USP Controlled Room Temperature].
All regulations concerning handling of pressure vessels must be followed.
Protect the cylinders from shocks, falls, oxidizing and flammable materials, moisture, and sources of heat or ignition.
INOmax MR conditional labeled cylinders (i.e., size 88 aluminum cylinder) may be used at 100 gauss or less. Use of any other cylinders (e.g., size D or 0.4 liter aluminum cylinder) may create a projectile hazard.
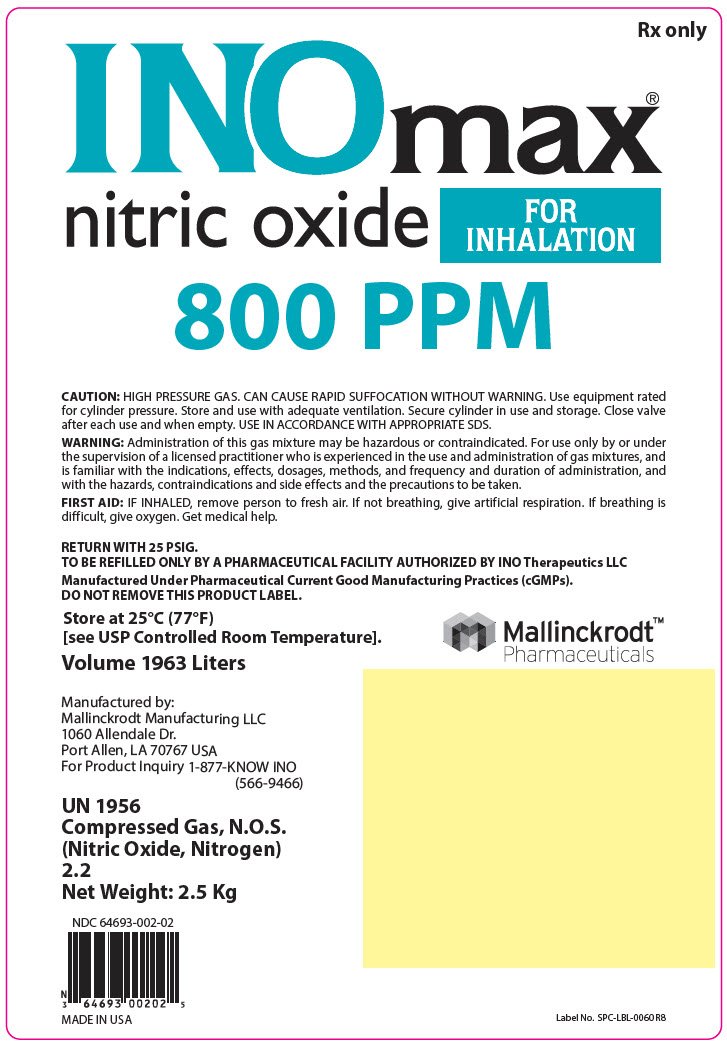
PRINCIPAL DISPLAY PANEL - 1963 Liter Cylinder Label
Rx only
INOmax®
nitric oxide
FOR
INHALATION
800 PPM
CAUTION: HIGH PRESSURE GAS. CAN CAUSE RAPID SUFFOCATION WITHOUT WARNING. Use equipment rated
for cylinder pressure. Store and use with adequate ventilation. Secure cylinder in use and storage. Close valve
after each use and when empty. USE IN ACCORDANCE WITH APPROPRIATE SDS.
WARNING: Administration of this gas mixture may be hazardous or contraindicated. For use only by or under
the supervision of a licensed practitioner who is experienced in the use and administration of gas mixtures, and
is familiar with the indications, effects, dosages, methods, and frequency and duration of administration, and
with the hazards, contraindications and side effects and the precautions to be taken.
FIRST AID: IF INHALED, remove person to fresh air. If not breathing, give artificial respiration. If breathing is
difficult, give oxygen. Get medical help.
RETURN WITH 25 PSIG.
TO BE REFILLED ONLY BY A PHARMACEUTICAL FACILITY AUTHORIZED BY INO Therapeutics LLC
Manufactured Under Pharmaceutical Current Good Manufacturing Practices (cGMPs).
DO NOT REMOVE THIS PRODUCT LABEL.
Store at 25°C (77°F)
[see USP Controlled Room Temperature].
Volume 1963 Liters
Mallinckrodt™
Pharmaceuticals
Manufactured by:
Mallinckrodt Manufacturing LLC
1060 Allendale Dr.
Port Allen, LA 70767 USA
For Product Inquiry 1-877-KNOW INO
(566-9466)
UN 1956
Compressed Gas, N.O.S.
(Nitric Oxide, Nitrogen)
2.2
Net Weight: 2.5 Kg
NDC 64693-002-02
MADE IN USA
Label No. SPC-LBL-0060 R8
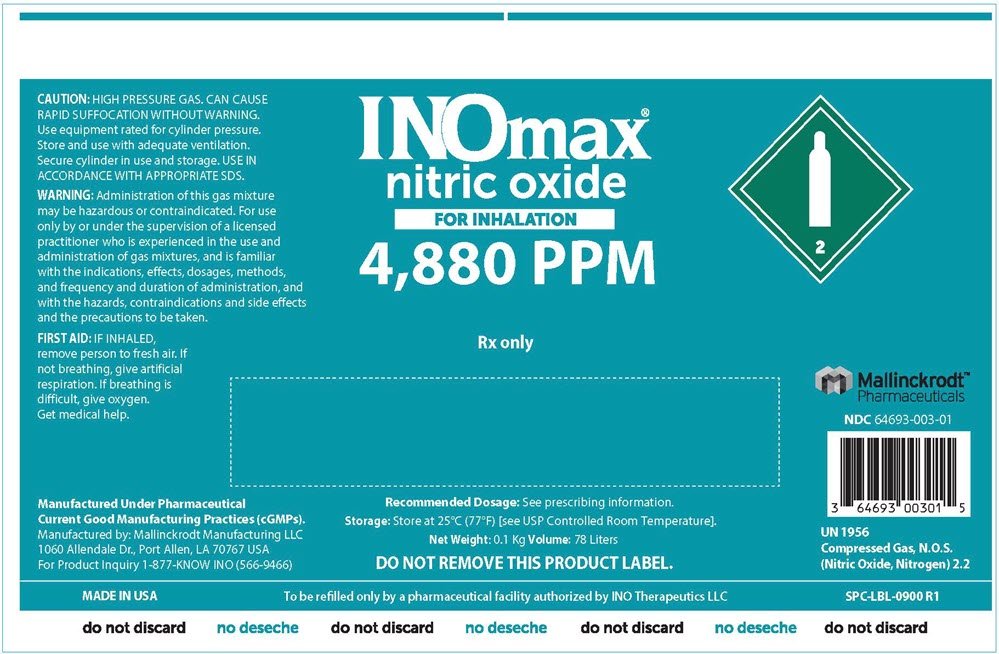
PRINCIPAL DISPLAY PANEL - 78 Liter Cylinder Label
INOmax®
nitric oxide
FOR INHALATION
4,880 PPM
2
Rx only
CAUTION: HIGH PRESSURE GAS. CAN CAUSE
RAPID SUFFOCATION WITHOUT WARNING.
Use equipment rated for cylinder pressure.
Store and use with adequate ventilation.
Secure cylinder in use and storage. USE IN
ACCORDANCE WITH APPROPRIATE SDS.
WARNING: Administration of this gas mixture
may be hazardous or contraindicated. For use
only by or under the supervision of a licensed
practitioner who is experienced in the use and
administration of gas mixtures, and is familiar
with the indications, effects, dosages, methods,
and frequency and duration of administration, and
with the hazards, contraindications and side effects
and the precautions to be taken.
FIRST AID: IF INHALED,
remove person to fresh air. If
not breathing, give artificial
respiration. If breathing is
difficult, give oxygen.
Get medical help.
Manufactured Under Pharmaceutical
Current Good Manufacturing Practices (cGMPs).
Manufactured by: Mallinckrodt Manufacturing LLC
1060 Allendale Dr., Port Allen, LA 70767 USA
For Product Inquiry 1-877-KNOW INO (566-9466)
Recommended Dosage: See prescribing information.
Storage: Store at 25°C (77°F) [see USP Controlled Room Temperature].
Net Weight: 0.1 Kg Volume: 78 Liters
DO NOT REMOVE THIS PRODUCT LABEL.
Mallinckrodt™
Pharmaceuticals
NDC 64693-003-01
UN 1956
Compressed Gas, N.O.S.
(Nitric Oxide, Nitrogen) 2.2
MADE IN USA
To be refilled only by a pharmaceutical facility authorized by INO Therapeutics LLC
SPC-LBL-0900 R1
do not discard
| INOMAX
nitric oxide gas |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| INOMAX
nitric oxide gas |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| Labeler - INO Therapeutics LLC (090546628) |
More about INOmax (nitric oxide)
- Check interactions
- Compare alternatives
- Side effects
- Dosage information
- During pregnancy
- Generic availability
- Drug class: miscellaneous respiratory agents
- Breastfeeding
- En español
