Covid-19 Vaccine Pfizer, Bivalent: Package Insert / Prescribing Info
Package insert / product label
Generic name: original and omicron ba.4/ba.5
Dosage form: injection, suspension
Drug class: Viral vaccines
Medically reviewed by Drugs.com. Last updated on Feb 3, 2025.
On This Page
- Indications and Usage
- Dosage and Administration
- Dosage Forms and Strengths
- Contraindications
- Warnings and Precautions
- Adverse Reactions/Side Effects
- Drug Interactions
- Use In Specific Populations
- Description
- Clinical Pharmacology
- How Supplied/Storage and Handling
- Storage and Handling
- Patient Counseling Information
FACT SHEET FOR HEALTHCARE PROVIDERS ADMINISTERING VACCINE: EMERGENCY USE AUTHORIZATION OF PFIZER-BIONTECH COVID-19 VACCINE (2024-2025 FORMULA), FOR 6 MONTHS THROUGH 11 YEARS OF AGE
|
HIGHLIGHTS OF EMERGENCY USE AUTHORIZATION (EUA)
These highlights of the EUA do not include all the information needed to use Pfizer-BioNTech COVID-19 Vaccine under the EUA. See the FULL FACT SHEET FOR HEALTHCARE PROVIDERS for Pfizer-BioNTech COVID-19 Vaccine.
Most Recent EUA Authorized Date: 8/2024
|
Individuals 5 Years Through 11 years of Age Irrespective of COVID-19 Vaccination Status |
||||
|
Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula) Vial Cap and Label Border Color |
Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula) Dosing Regimen, Dose and Schedulea |
||||
|
Blue |
Single dose, 0.3 mL |
||||
|
|
a. For individuals with certain kinds of immunocompromise, see text below tables for dosing information. b. Previous dose refers to a dose of any prior COVID-19 vaccine that is no longer authorized for use in the United States. |
||||
|
Individuals 6 months through 11 years of age with certain kinds of immunocompromise should complete at least a 3-dose series with an age-appropriate dose and dosing schedule of a COVID-19 vaccine. At least 1 dose should be with a COVID-19 vaccine (2024-2025 Formula). Certain kinds of immunocompromise refers to individuals who have undergone solid organ transplantation, or who are diagnosed with conditions that are considered to have an equivalent level of immunocompromise. (2.3)
|
|||||
|
|
--------DOSAGE FORMS AND STRENGTHS--------
|
||||
|
Individuals 6 Months Through 4 Years of Age by Pfizer-BioNTech COVID-19 Vaccination Status |
--------CONTRAINDICATIONS--------
|
||||
|
Number of Previous Doses of Pfizer-BioNTech COVID-19 Vaccine(s)a |
Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula) Vial Cap and Label Border Color |
Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula) Dosing Regimen, Dose and Scheduleb |
--------WARNINGS AND PRECAUTIONS-------
|
||
|
0c |
Yellow |
3 dosesd, 0.3 mL each Dose 1: Week 0 Dose 2: Week 3 Dose 3: ≥8 weeks after Dose 2 |
--------ADVERSE REACTIONS--------
|
||
|
1 |
Yellow |
2 dosesd, 0.3 mL each Dose 1: 3 weeks after receipt of the previous dose of Pfizer-BioNTech COVID-19 Vaccinea Dose 2: ≥8 weeks after Dose 1 |
Vaccination providers must report all vaccine administration errors, all serious adverse events, cases of myocarditis, cases of pericarditis, cases of Multisystem Inflammatory Syndrome (MIS), and cases of COVID-19 that result in hospitalization or death following administration of Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula) to the Vaccine Adverse Event Reporting System (VAERS) by submitting online at https://vaers.hhs.gov/reportevent.html. For further assistance with reporting to VAERS call 1-800-822-7967. The reports should include the words “Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula) EUA” in the description section of the report. To the extent feasible, report adverse events to Pfizer 1-800-438-1985 or provide a copy of the VAERS form to Pfizer https://www.pfizersafetyreporting.com/ (6.3)
|
||
|
≥2 |
Yellow |
Single dose, 0.3 mL ≥8 weeks after receipt of the last previous dose of Pfizer-BioNTech COVID-19 Vaccinea | |||
|
a. Previous dose refers to a dose of any prior Pfizer-BioNTech COVID-19 that is no longer authorized for use in the United States. b. For individuals with certain kinds of immunocompromise previously vaccinated with Pfizer-BioNTech COVID-19 vaccines, see text below tables for dosing information. c. Not previously vaccinated with any COVID-19 vaccine.
d. For individuals turning from 4 to 5 years of age during the vaccination series who have received 1 or 2 doses of Pfizer-BioNTech COVID-19 Vaccine, administer a single dose of with Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula) supplied in vials with blue caps and labels with blue borders, on or after the date the individual turns 5 years of age. | |||||
1. Indications and Usage for Covid-19 Vaccine Pfizer, Bivalent
The U.S. Food and Drug Administration (FDA) has issued an Emergency Use Authorization (EUA) for the emergency use of Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula) for active immunization to prevent coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in individuals 6 months through 11 years of age.
Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula), which is supplied in multiple dose vials with yellow caps and labels with yellow borders, and in single dose vials with blue caps and labels with blue borders, is not licensed for any use.
Justification for Emergency Use of Vaccines During the COVID-19 Pandemic
There is currently an outbreak of COVID-19 caused by SARS-CoV-2. The Secretary of the Department of Health and Human Services (HHS) has:
- •
- Determined that there is a public-health emergency, or a significant potential for a public-health emergency, related to COVID-19.1
- •
- Declared that circumstances exist justifying the authorization of emergency use of drugs and biological products during the COVID-19 pandemic.2
An EUA is an FDA authorization for the emergency use of an unapproved product or unapproved use of an approved product (i.e., drug, biological product, or device) in the United States under certain circumstances including, but not limited to, when the Secretary of HHS declares that use of EUA authority is justified, based on a determination that there is a public-health emergency, or a significant potential for a public-health emergency, that affects, or has a significant potential to affect, national security or the health and security of United States citizens living abroad, and that involves biological agent(s) or a disease or condition that may be attributable to such agent(s). Criteria for issuing an EUA include:
- •
- The biological agent(s) can cause a serious or life-threatening disease or condition;
- •
- Based on the totality of the available scientific evidence (including data from adequate and well-controlled clinical trials, if available), it is reasonable to believe that:
- o
- The product may be effective in diagnosing, treating, or preventing the serious or life-threatening disease or condition;
- o
- The known and potential benefits of the product - when used to diagnose, prevent, or treat such disease or condition - outweigh the known and potential risks of the product, taking into consideration the material threat posed by the biological agent(s); and
- •
- There is no adequate, approved, and available alternative to the product for diagnosing, preventing, or treating the serious or life-threatening disease or condition.
Information Regarding Available Alternative Vaccines for the Prevention of COVID-19 in Individuals 6 Months Through 11 Years of Age
There may be clinical trials or availability under EUA of other COVID-19 vaccines, including vaccines that contain or encode the spike protein of the SARS-CoV-2 Omicron variant lineage KP.2.
- 1
- See U.S. Department of Health and Human Services, Determination of a Public Health Emergency and Declaration that Circumstances Exist Justifying Authorizations Pursuant to Section 564(b) of the Federal Food, Drug, and Cosmetic Act, 21 U.S.C. § 360bbb-3. February 4, 2020; https://www.federalregister.gov/documents/2020/02/07/2020-02496/determination-of-public-health-emergency. See also U.S. Department of Health and Human Services, Amended Determination of a Public Health Emergency or Significant Potential for a Public Health Emergency Pursuant to Section 564(b) of the Federal Food, Drug, and Cosmetic Act, 21 U.S.C. § 360bbb-3(b). March 15, 2023 (“Amended Determination”); https://www.federalregister.gov/documents/2023/03/20/2023-05609/covid-19-emergency-use-authorization-declaration. See U.S. Department of Health and Human Services, Determination of a Public Health Emergency and Declaration that Circumstances Exist Justifying Authorizations Pursuant to Section 564(b) of the Federal Food, Drug, and Cosmetic Act, 21 U.S.C. § 360bbb-3. February 4, 2020; https://www.federalregister.gov/documents/2020/02/07/2020-02496/determination-of-public-health-emergency. See also U.S. Department of Health and Human Services, Amended Determination of a Public Health Emergency or Significant Potential for a Public Health Emergency Pursuant to Section 564(b) of the Federal Food, Drug, and Cosmetic Act, 21 U.S.C. § 360bbb-3(b). March 15, 2023 (“Amended Determination”); https://www.federalregister.gov/documents/2023/03/20/2023-05609/covid-19-emergency-use-authorization-declaration.
- 2
- See U.S. Department of Health and Human Services, Declaration that Circumstances Exist Justifying Authorizations Pursuant to Section 564(b) of the Federal Food, Drug, and Cosmetic Act, 21 U.S.C. § 360bbb-3, 85 FR 18250 (April 1, 2020); https://www.federalregister.gov/documents/2020/04/01/2020-06905/emergency-use-authorization-declaration. See also Amended Determination (“The declarations issued pursuant to section 564(b)(1) of the FD&C Act that circumstances exist justifying the authorization of emergency use of certain in vitro diagnostics, personal respiratory protective devices, other medical devices and drugs and biological products, as set forth in those declarations, and that are based on the February 4, 2020 determination, remain in effect until those declarations are terminated in accordance with section 564 of the FD&C Act.”).
2. Covid-19 Vaccine Pfizer, Bivalent Dosage and Administration
For intramuscular injection only.
2.1 Preparation for Administration
There are 2 presentations of Pfizer-BioNTech COVID-19 Vaccine:
|
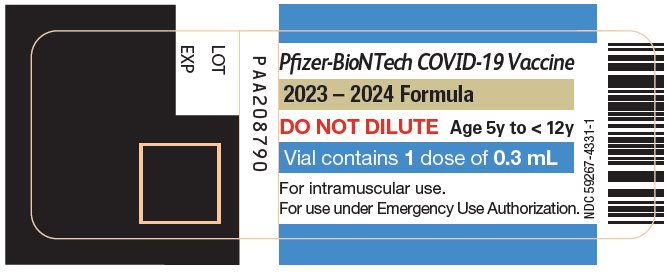
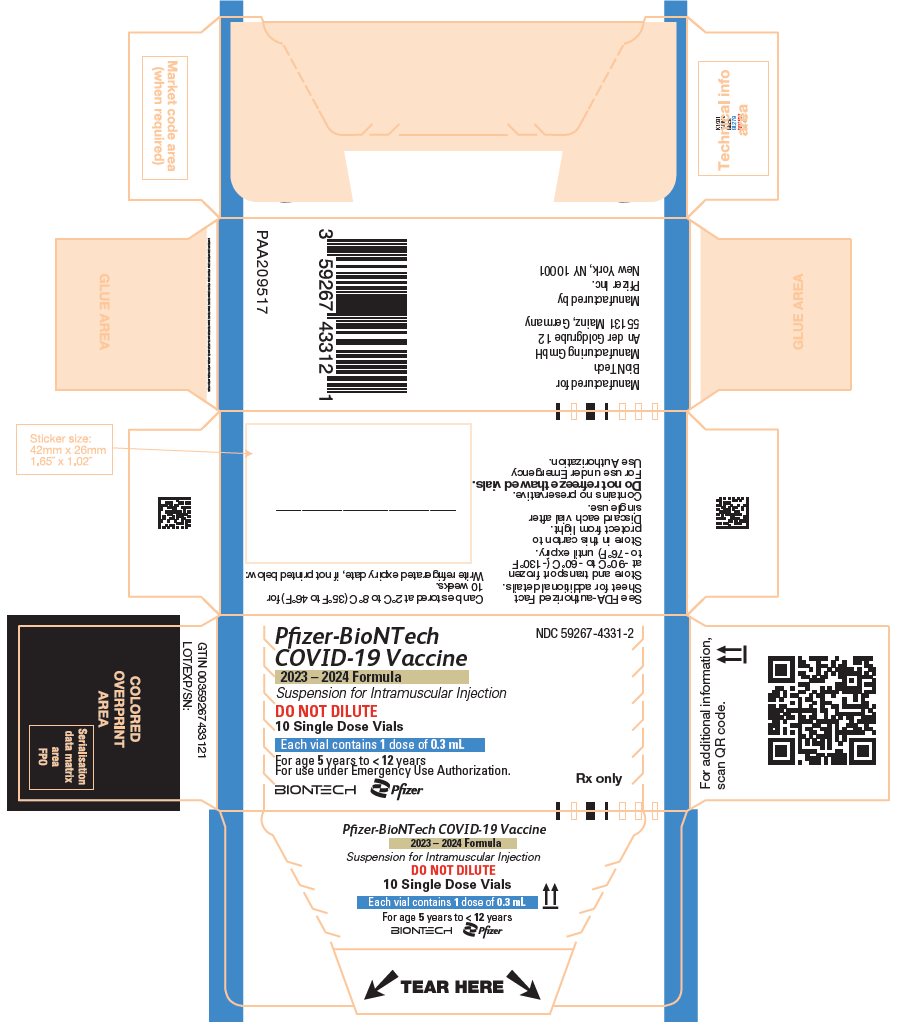
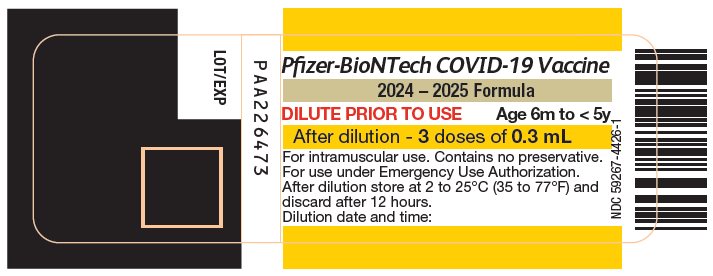
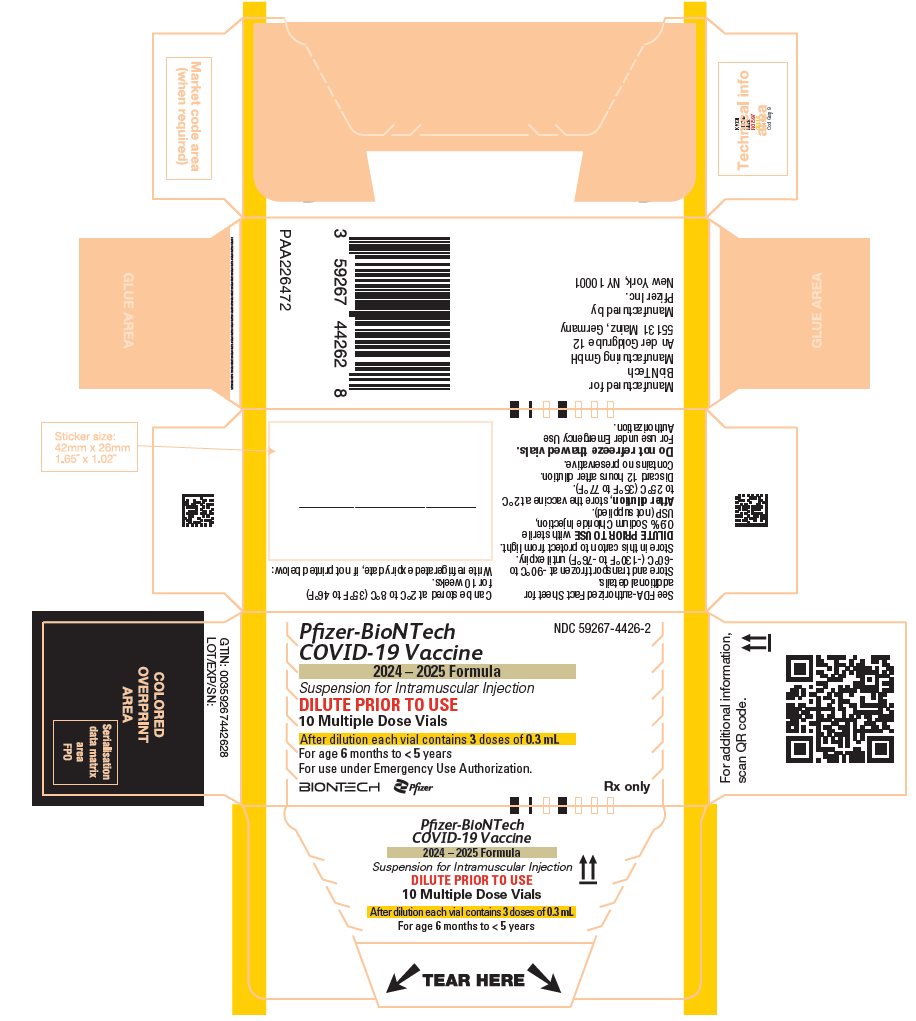
Vial Cap and Vial Label Border Color |
Age of Recipient |
Vial Type |
Dilution Required |
|
Yellow |
6 months through 4 years of age |
Multiple dose |
Yes |
|
Blue |
5 through 11 years of age |
Single dose |
No |
Pfizer-BioNTech COVID-19 Vaccine vials contain a frozen suspension that does not contain a preservative and must be thawed prior to administration.
If vials are frozen, they must be thawed prior to use [for thawing instructions, see How Supplied/Storage and Handling (16)].
For multiple dose vials with yellow caps and labels with yellow borders:
- •
-
Dilute prior to use:
- o
- Verify that the vial states 2024-2025 Formula.
- o
- Check the contents of the vial during preparation. The liquid should be clear to slightly opalescent with no visible particles. Do not use if liquid is discolored or if particles are observed.
- o
- Add 1.1 mL of sterile 0.9% Sodium Chloride Injection, USP into the vaccine vial.
- o
- Before removing the needle from the vial, equalize vial pressure by withdrawing air into the empty diluent syringe.
- o
- Gently invert the vaccine vial 10 times to mix. Do not shake.
- o
- Record the date and time of dilution on the vial label.
- o
- Store at 2ºC to 25°C (35°F to 77°F) and discard after 12 hours.
- •
- After dilution, multiple-dose vials contain 3 doses of 0.3 mL each.
- •
- If the amount of vaccine in the vial cannot provide a full dose of 0.3 mL, discard the vial and any excess volume. Do not pool excess vaccine from multiple vials.
For single dose vials with blue caps and labels with blue borders:
- •
- Verify that the vial states 2024-2025 Formula.
- •
- Do Not Dilute.
- •
- Prior to withdrawing the dose, mix by inverting the vial gently 10 times. Do not shake.
- •
- Withdraw a single 0.3 mL dose.
- •
- Discard vial and any excess volume.
2.2 Administration
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. The vaccine should be clear to slightly opalescent suspension. Do not administer if vaccine is discolored or contains particulate matter.
Administer a single 0.3 mL dose intramuscularly.
2.3 Dose and Schedule
|
||
|
Number of Previous Doses of Pfizer-BioNTech COVID-19 Vaccine(s)* |
Pfizer-BioNTech COVID-19 Vaccine, (2024-2025 Formula) Vial Cap and Label Border Color |
Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula) Dosing Regimen, Dose and Schedule† |
|
0‡ |
Yellow |
3 doses§, 0.3 mL each Dose 1: Week 0 Dose 2: Week 3 Dose 3: ≥8 weeks after Dose 2 |
|
1 |
Yellow |
2 doses§, 0.3 mL each Dose 1: 3 weeks after receipt of the |
|
≥2 |
Yellow |
Single dose, 0.3 mL ≥8 weeks after receipt of the last |
| Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula)
Vial Cap and Label Border Color | Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula)
Dosing Regimen, Dose and Schedule* |
|---|---|
|
Blue |
Single dose, 0.3 mL (If previously vaccinated, administer the dose ≥2 months after receipt of the last previous dose of COVID‑19 vaccine)† |
Individuals 6 Months Through 11 Years of Age with Certain Kinds of Immunocompromise
Individuals 6 months through 11 years of age with certain kinds of immunocompromise3 should complete at least a 3-dose series with an age-appropriate dose and dosing schedule4,5 of a COVID-19 vaccine. At least 1 dose should be with a COVID-19 vaccine (2024-2025 Formula).
- •
- If previously not vaccinated, complete the 3-dose series with age-appropriate doses of Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula).
- •
- If previously vaccinated with 1 or 2 dose(s) of a prior Pfizer-BioNTech COVID-19 Vaccine6, complete the remaining dose(s) in the 3-dose series with age-appropriate doses of Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula).
- •
- If previously vaccinated with 3 or more doses of a prior COVID-19 vaccine6, administer a single age-appropriate dose of Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula) at least 2 months following the last dose.
An age-appropriate additional dose of Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula) may be administered at least 2 months following the last dose of a COVID-19 vaccine (2024-2025 Formula).7,8 Age-appropriate additional doses of Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula) may be administered at the discretion of the healthcare provider, taking into consideration the individual’s clinical circumstances. The timing of the additional doses may be based on the individual’s clinical circumstances.
- 3
- Certain kinds of immunocompromise refers to individuals who have undergone solid organ transplantation, or who are diagnosed with conditions that are considered to have an equivalent level of immunocompromise.
- 4
- Dosing schedule for immunocompromised individuals 6 months through 4 years of age for Pfizer-BioNTech COVID-19 vaccines: Dose 1: Week 0; Dose 2: Week 3; Dose 3: ≥8 Weeks after Dose 2. For individuals turning from 4 to 5 years of age during the vaccination series, complete the series with doses of Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula) supplied in vials with blue caps and labels with blue borders on or after the date the individual turns 5 years of age.
- 5
- Dosing schedule for immunocompromised individuals 5 through 11 years of age for Pfizer-BioNTech COVID-19 vaccines: Dose 1: Week 0; Dose 2: Week 3; Dose 3: ≥4 weeks after Dose 2. For individuals turning from 11 to 12 years of age during the vaccination series, complete the 3-dose series with 1 or 2 doses, as applicable, of COMIRNATY (COVID-19 Vaccine, mRNA) (2024-2025 Formula) on or after the date the individual turns 12 years of age. If the individual turning 12 years of age receives 2 doses of COMIRNATY (COVID-19 Vaccine, mRNA) (2024-2025 Formula) to complete the vaccination series or receives a dose of COMIRNATY (COVID-19 Vaccine, mRNA) (2024-2025 Formula) less than 2 months after receipt of the last previous dose of COVID-19 vaccine to complete the vaccination series, then those uses of COMIRNATY (COVID-19 Vaccine, mRNA) (2024-2025 Formula) are authorized under EUA. The FDA has authorized under EUA these uses of COMIRNATY (COVID-19 Vaccine, mRNA) (2024-2025 Formula), which is an FDA-licensed vaccine indicated for active immunization to prevent COVID-19 in individuals 12 years of age and older. Refer to https://www.cvdvaccine.com for additional information about COMIRNATY (COVID-19 Vaccine, mRNA) (2024-2025 Formula).
- 6
- These prior COVID-19 vaccines are no longer authorized for use in the United States.
- 7
- For immunocompromised individuals 6 months through 4 years of age, the last dose of a COVID-19 vaccine (2024-2025 Formula) refers to a dose with Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula).
- 8
- For immunocompromised individuals 5 through 11 years of age, the last dose of a COVID-19 vaccine (2024-2025 Formula) refers to a dose with Moderna COVID-19 Vaccine (2024-2025 Formula) or Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula).
3. Dosage Forms and Strengths
Pfizer-BioNTech COVID-19 Vaccine is a suspension for injection.
A single dose is 0.3 mL.
4. Contraindications
Do not administer Pfizer-BioNTech COVID-19 Vaccine to individuals with a history of a severe allergic reaction (e.g., anaphylaxis) to any component of the Pfizer-BioNTech COVID-19 Vaccine [see Description (11)] or to individuals who had a severe allergic reaction (e.g., anaphylaxis) following a previous dose of a Pfizer-BioNTech COVID-19 Vaccine.
5. Warnings and Precautions
5.1 Management of Acute Allergic Reactions
Appropriate medical treatment must be immediately available to manage potential anaphylactic reactions following administration of Pfizer-BioNTech COVID-19 Vaccine.
Monitor Pfizer-BioNTech COVID-19 Vaccine recipients for the occurrence of immediate adverse reactions according to the Centers for Disease Control and Prevention (CDC) guidelines (https://www.cdc.gov/vaccines/covid-19/clinical-considerations/managing-anaphylaxis.html).
5.2 Myocarditis and Pericarditis
Postmarketing data with authorized or approved mRNA COVID-19 vaccines demonstrate increased risks of myocarditis and pericarditis, particularly within the first week following vaccination. For the Pfizer-BioNTech COVID-19 Vaccine, the observed risk is highest in males 12 through 17 years of age. Although some cases required intensive care support, available data from short-term follow-up suggest that most individuals have had resolution of symptoms with conservative management. Information is not yet available about potential long-term sequelae.
The CDC has published considerations related to myocarditis and pericarditis after vaccination, including for vaccination of individuals with a history of myocarditis or pericarditis (https://www.cdc.gov/vaccines/covid-19/clinical-considerations/myocarditis.html).
5.3 Syncope
Syncope (fainting) may occur in association with administration of injectable vaccines. Procedures should be in place to avoid injury from fainting.
6. Adverse Reactions/Side Effects
An overview of clinical studies contributing to the safety assessment of Pfizer-BioNTech COVID-19 Vaccine in individuals 6 months through 11 years of age is provided in Table 1. Participants in these clinical studies received a 2- or 3-dose initial series depending on age, with 3 weeks between Dose 1 and Dose 2 and 8 weeks between Dose 2 and Dose 3 (referred to as a primary series) and subsequent doses (referred to as booster dose(s)).
Table 1: Clinical Studies
| Abbreviation: SARS-CoV-2 = severe acute respiratory syndrome coronavirus 2. | ||||
|
||||
|
Study |
Age Group |
Vaccine Strain Composition |
Dosing |
Number of Participants |
|
Primary Series | ||||
|
Study 1 (NCT04380701) |
18 through 55 years |
Original* |
Primary series |
60 |
|
Study 2 (NCT04368728) |
12 through 15 years |
Original* |
Primary series |
1131† |
|
≥16 years |
Original* |
Primary series |
21720† |
|
|
Study 3 (NCT04816643) |
5 through 11 years |
Original* |
Primary series |
3109 |
|
2 through 4 years |
Original* |
Primary series |
606 |
|
|
6 through 23 months |
Original* |
Primary series |
386 |
|
|
Booster Dose | ||||
|
Study 2 (NCT04368728) |
18 through 55 years |
Original* |
1st booster |
306 |
|
Study 3 (NCT04816643) |
5 through 11 years |
Original* |
1st booster |
401 |
|
Study 5 (NCT05472038) |
≥12 years of age |
Original and Omicron BA.4/BA.5‡ |
2nd booster |
316 |
|
Study 6 (NCT05543616) |
5 through 11 years |
Original and Omicron BA.4/BA.5‡ |
2nd booster |
113 |
|
2 through 4 years |
Original and Omicron BA.4/BA.5‡ |
1st booster (4th dose) |
36 |
|
|
6 through 23 months |
Original and Omicron BA.4/BA.5‡ |
1st booster (4th dose) |
24 |
|
|
Study 4 (NCT04955626) |
>55 years |
2nd booster |
610 |
|
The safety data accrued with the Pfizer-BioNTech COVID-19 Vaccine (Original monovalent, no longer authorized for use in the U.S.), Pfizer-BioNTech’s bivalent COVID-19 Vaccine (Original and Omicron BA.1) [not authorized or approved in the U.S., hereafter referred to as bivalent vaccine (Original and Omicron BA.1)] and Pfizer-BioNTech COVID-19 Vaccine, Bivalent (Original and Omicron, BA.4/BA.5) [no longer authorized for use in the U.S.] are relevant to Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula) because these vaccines are manufactured using the same process.
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a vaccine cannot be directly compared with rates in the clinical trials of another vaccine and may not reflect the rates observed in practice.
Pfizer-BioNTech COVID-19 Vaccine (Original Monovalent)
The safety of a primary series Pfizer-BioNTech COVID-19 Vaccine was evaluated in participants 6 months of age and older in 3 clinical studies conducted in the United States, Europe, Turkey, South Africa and South America.
Study BNT162-01 (Study 1) was a Phase 1/2, 2-part, dose-escalation trial that enrolled 60 participants, 18 through 55 years of age. Study C4591001 (Study 2) is a Phase 1/2/3, multicenter, multinational, randomized, saline placebo-controlled, observer-blind, dose finding, vaccine candidate-selection (Phase 1) and efficacy (Phase 2/3) study that has enrolled approximately 46,000 participants, 12 years of age and older. Of these, approximately 43,448 participants [21,720 Pfizer-BioNTech COVID-19 Vaccine (30 mcg modRNA); 21,728 placebo] in Phase 2/3 are 16 years of age or older (including 138 and 145 participants 16 and 17 years of age in the vaccine and placebo groups, respectively) and 2,260 participants are 12 through 15 years of age (1,131 and 1,129 in the vaccine and placebo groups, respectively). Study C4591007 (Study 3) is a Phase 1/2/3 multicenter, randomized, dose finding, open-label (Phase 1) and multinational, saline placebo-controlled, observer-blind, immunogenicity and efficacy (Phase 2/3) study that has enrolled 4,695 participants 5 through 11 years of age, of whom 3,109 participants received Pfizer-BioNTech COVID-19 Vaccine (10 mcg modRNA) and 1,538 participants received placebo in Phase 2/3. Study 3 also enrolled 1,776 participants 6 through 23 months of age, of whom 1,178 participants were in the Pfizer-BioNTech COVID-19 Vaccine (3 mcg modRNA) group and 598 participants in the placebo group; and also enrolled 2,750 participants 2 through 4 years of age, of whom 1,835 participants were in the Pfizer-BioNTech COVID-19 Vaccine group and 915 participants in the placebo group in Phase 2/3.
In Study 2 and Study 3, all participants 6 months through 4 years of age, 5 through 11 years of age, 12 through 15 years of age, and a subset of participants 16 years of age and older, were monitored for solicited local and systemic reactions and use of antipyretic medication after each vaccination in an electronic diary. Participants are being monitored for unsolicited adverse events, including serious adverse events, throughout the study [from Dose 1 through 1 month after the last vaccination (all unsolicited adverse events) or 6 months (serious adverse events) after the last vaccination].
Pfizer-BioNTech COVID-19 Vaccine (Original Monovalent) Administered as a Primary Series
Participants 16 Years of Age and Older (2-Dose Primary Series)
At the time of the analysis of Study 2 for the EUA, 37,586 [18,801 Pfizer-BioNTech COVID-19 Vaccine (30 mcg modRNA) and 18,785 placebo] participants 16 years of age or older had been followed for a median of 2 months after the second dose.
The safety evaluation in Study 2 is ongoing. The safety population includes participants 16 years of age and older enrolled by October 9, 2020, and includes safety data accrued through November 14, 2020.
Demographic characteristics in Study 2 were generally similar with regard to age, gender, race, and ethnicity among participants who received Pfizer-BioNTech COVID-19 Vaccine and those who received placebo. Overall, among the total participants who received either the Pfizer-BioNTech COVID-19 Vaccine or placebo, 50.6% were male and 49.4% were female, 83.1% were White, 9.1% were Black or African American, 28.0% were Hispanic/Latino, 4.3% were Asian, and 0.5% were American Indian/Alaska Native.
Unsolicited Adverse Events
Serious Adverse Events
In Study 2, among participants 16 through 55 years of age who had received at least 1 dose of vaccine or placebo (Pfizer-BioNTech COVID-19 Vaccine = 10,841; placebo = 10,851), serious adverse events from Dose 1 through up to 30 days after Dose 2 in ongoing follow-up were reported by 0.4% of Pfizer-BioNTech COVID-19 Vaccine recipients and by 0.3% of placebo recipients. In a similar analysis, in participants 56 years of age and older (Pfizer-BioNTech COVID-19 Vaccine = 7,960, placebo = 7,934), serious adverse events were reported by 0.8% of Pfizer-BioNTech COVID-19 Vaccine recipients and by 0.6% of placebo recipients who received at least 1 dose of Pfizer-BioNTech COVID-19 Vaccine or placebo, respectively. In these analyses, 91.6% of study participants had at least 30 days of follow-up after Dose 2.
Appendicitis was reported as a serious adverse event for 12 participants, and numerically higher in the vaccine group, 8 vaccine participants and 4 placebo participants. Currently available information is insufficient to determine a causal relationship with the vaccine. There were no other notable patterns or numerical imbalances between treatment groups for specific categories of serious adverse events (including neurologic, neuro-inflammatory, and thrombotic events) that would suggest a causal relationship to Pfizer-BioNTech COVID-19 Vaccine.
Non-Serious Adverse Events
In Study 2 in which 10,841 participants 16 through 55 years of age received Pfizer-BioNTech COVID-19 Vaccine and 10,851 participants received placebo, non-serious adverse events from Dose 1 through up to 30 days after Dose 2 in ongoing follow-up were reported in 29.3% of participants who received Pfizer-BioNTech COVID-19 Vaccine and 13.2% of participants in the placebo group, for participants who received at least 1 dose. Overall, in a similar analysis in which 7,960 participants 56 years of age and older received Pfizer-BioNTech COVID-19 Vaccine, non-serious adverse events within 30 days were reported in 23.8% of participants who received Pfizer-BioNTech COVID-19 Vaccine and 11.7% of participants in the placebo group, for participants who received at least 1 dose. In these analyses, 91.6% of study participants had at least 30 days of follow-up after Dose 2.
The higher frequency of reported unsolicited non-serious adverse events among Pfizer-BioNTech COVID-19 Vaccine recipients compared to placebo recipients was primarily attributed to local and systemic adverse events reported during the first 7 days following vaccination that are consistent with adverse reactions solicited among participants in the reactogenicity subset. From Dose 1 through 30 days after Dose 2, reports of lymphadenopathy were imbalanced with notably more cases in the Pfizer-BioNTech COVID-19 Vaccine group (64) vs. the placebo group (6), which is plausibly related to vaccination. Throughout the safety follow-up period to date, Bell’s palsy (facial paralysis) was reported by 4 participants in the Pfizer-BioNTech COVID-19 Vaccine group. Onset of facial paralysis was Day 37 after Dose 1 (participant did not receive Dose 2) and Days 3, 9, and 48 after Dose 2. No cases of Bell’s palsy were reported in the placebo group. Currently available information is insufficient to determine a causal relationship with the vaccine. There were no other notable patterns or numerical imbalances between treatment groups for specific categories of non-serious adverse events (including other neurologic or neuro-inflammatory, and thrombotic events) that would suggest a causal relationship to Pfizer-BioNTech COVID-19 Vaccine.
Participants 12 Through 15 Years of Age (2-Dose Primary Series)
In an analysis of Study 2, based on data up to the cutoff date of March 13, 2021, 2,260 participants (1,131 Pfizer-BioNTech COVID-19 Vaccine (30 mcg modRNA); 1,129 placebo) were 12 through 15 years of age. Of these, 1,308 (660 Pfizer-BioNTech COVID-19 Vaccine and 648 placebo) participants have been followed for at least 2 months after the second dose. The safety evaluation in Study 2 is ongoing.
Demographic characteristics in Study 2 were generally similar with regard to age, gender, race, and ethnicity among participants who received Pfizer-BioNTech COVID-19 Vaccine and those who received placebo. Overall, among the participants who received the Pfizer-BioNTech COVID-19 Vaccine, 50.1% were male and 49.9% were female, 85.9% were White, 4.6% were Black or African American, 11.7% were Hispanic/Latino, 6.4% were Asian, and 0.4% were American Indian/Alaska Native.
Unsolicited Adverse Events
In the following analyses of Study 2 in participants 12 through 15 years of age (1,131 of whom received Pfizer-BioNTech COVID-19 Vaccine and 1,129 of whom received placebo), 98.3% of study participants had at least 30 days of follow-up after Dose 2.
Serious Adverse Events
Serious adverse events from Dose 1 through up to 30 days after Dose 2 in ongoing follow-up were reported by 0.4% of Pfizer-BioNTech COVID-19 Vaccine recipients and by 0.1% of placebo recipients. There were no notable patterns or numerical imbalances between treatment groups for specific categories of serious adverse events that would suggest a causal relationship to Pfizer-BioNTech COVID-19 Vaccine.
Non-Serious Adverse Events
Non-serious adverse events from Dose 1 through up to 30 days after Dose 2 in ongoing follow-up were reported by 5.8% of Pfizer-BioNTech COVID-19 Vaccine recipients and by 5.8% of placebo recipients. From Dose 1 through 30 days after Dose 2, reports of lymphadenopathy plausibly related to the study intervention were imbalanced, with notably more cases in the Pfizer-BioNTech COVID-19 Vaccine group (7) vs. the placebo group (1). There were no other notable patterns or numerical imbalances between treatment groups for specific categories of non-serious adverse events that would suggest a causal relationship to Pfizer-BioNTech COVID-19 Vaccine.
Participants 5 Through 11 Years of Age (2-Dose Primary Series)
In an analysis of Study 3 Phase 2/3, based on data up to the cutoff date of September 06, 2021, 2,268 participants [1,518 Pfizer-BioNTech COVID-19 Vaccine (10 mcg modRNA); 750 placebo] were 5 through 11 years of age. Of these, 2,158 (95.1%) [1,444 Pfizer-BioNTech COVID-19 Vaccine (10 mcg modRNA) and 714 placebo] participants have been followed for at least 2 months after the second dose. An analysis of Study 3 Phase 2/3 adverse event data also included another 2,379 participants [1,591 Pfizer-BioNTech COVID-19 Vaccine (10 mcg modRNA) and 788 placebo], of whom 71.2% had a follow-up period for at least 2 weeks after Dose 2 up to the cutoff date of October 8, 2021. The safety evaluation in Study 3 is ongoing.
Demographic characteristics in Study 3 were generally similar with regard to age, gender, race, and ethnicity among participants 5 through 11 years of age who received Pfizer-BioNTech COVID-19 Vaccine (10 mcg modRNA) and those who received placebo. Among the 4,647 participants 5 through 11 years of age who received at least 1 dose of the Pfizer-BioNTech COVID-19 Vaccine (10 mcg modRNA) or placebo, 51.8% were male and 48.2% were female, 77.3% were White, 5.8% were Black or African American, 16.9% were Hispanic/Latino, 8.3% were Asian, and 0.4% were American Indian/Alaska Native.
Solicited Local and Systemic Adverse Reactions
The mean duration of pain at the injection site after Dose 2 was 2.3 days (range 1 to 11 days), for redness 2.2 days (range 1 to 10 days), and for swelling 2.2 days (range 1 to 10 days) for children in the Pfizer-BioNTech COVID-19 Vaccine (10 mcg modRNA) group up to the cutoff date of September 06, 2021.
| Pfizer-BioNTech COVID-19 Vaccine†
Dose 1 N‡=1511 n§ (%) | Placebo
Dose 1 N‡,¶=748 n§ (%) | Pfizer-BioNTech COVID-19 Vaccine†
Dose 2 N‡=1501 n§ (%) | Placebo
Dose 2 N‡,¶=740 n§ (%) |
|
|---|---|---|---|---|
| Note: Reactions were collected in an electronic diary (e-diary) from Day 1 to Day 7 after vaccination. | ||||
|
||||
|
Redness# |
||||
|
Any (≥0.5 cm) |
222 (14.7) |
43 (5.7) |
278 (18.5) |
40 (5.4) |
|
Mild |
143 (9.5) |
37 (4.9) |
143 (9.5) |
31 (4.2) |
|
Moderate |
79 (5.2) |
6 (0.8) |
132 (8.8) |
9 (1.2) |
|
Severe |
0 |
0 |
3 (0.2) |
0 |
|
Swelling# |
||||
|
Any (≥0.5 cm) |
158 (10.5) |
20 (2.7) |
229 (15.3) |
20 (2.7) |
|
Mild |
85 (5.6) |
13 (1.7) |
117 (7.8) |
15 (2.0) |
|
Moderate |
72 (4.8) |
7 (0.9) |
112 (7.5) |
5 (0.7) |
|
Severe |
1 (0.1) |
0 |
0 |
0 |
|
Pain at the injection siteÞ |
||||
|
Any |
1119 (74.1) |
234 (31.3) |
1065 (71.0) |
218 (29.5) |
|
Mild |
890 (58.9) |
204 (27.3) |
793 (52.8) |
192 (25.9) |
|
Moderate |
225 (14.9) |
30 (4.0) |
267 (17.8) |
26 (3.5) |
|
Severe |
4 (0.3) |
0 |
5 (0.3) |
0 |
| Note: Events and use of antipyretic or pain medication were collected in an electronic diary (e-diary) from Day 1 to Day 7 after each dose. | ||||
|
||||
|
Fever |
||||
|
≥38.0℃ |
38 (2.5) |
10 (1.3) |
98 (6.5) |
9 (1.2) |
|
≥38.0℃ to 38.4℃ |
23 (1.5) |
4 (0.5) |
51 (3.4) |
5 (0.7) |
|
>38.4℃ to 38.9℃ |
12 (0.8) |
5 (0.7) |
38 (2.5) |
3 (0.4) |
|
>38.9℃ to 40.0℃ |
3 (0.2) |
1 (0.1) |
8 (0.5) |
1 (0.1) |
|
>40.0℃ |
0 |
0 |
1 (0.1) |
0 |
|
Fatigue# |
||||
|
Any |
508 (33.6) |
234 (31.3) |
592 (39.4) |
180 (24.3) |
|
Mild |
333 (22.0) |
150 (20.1) |
321 (21.4) |
96 (13.0) |
|
Moderate |
171 (11.3) |
83 (11.1) |
260 (17.3) |
83 (11.2) |
|
Severe |
4 (0.3) |
1 (0.1) |
11 (0.7) |
1 (0.1) |
|
Headache# |
||||
|
Any |
339 (22.4) |
180 (24.1) |
420 (28.0) |
138 (18.6) |
|
Mild |
249 (16.5) |
131 (17.5) |
281 (18.7) |
93 (12.6) |
|
Moderate |
88 (5.8) |
45 (6.0) |
136 (9.1) |
45 (6.1) |
|
Severe |
2 (0.1) |
4 (0.5) |
3 (0.2) |
0 |
|
Chills# |
||||
|
Any |
70 (4.6) |
35 (4.7) |
147 (9.8) |
32 (4.3) |
|
Mild |
54 (3.6) |
30 (4.0) |
105 (7.0) |
24 (3.2) |
|
Moderate |
16 (1.1) |
5 (0.7) |
40 (2.7) |
7 (0.9) |
|
Severe |
0 |
0 |
2 (0.1) |
1 (0.1) |
|
VomitingÞ |
||||
|
Any |
33 (2.2) |
11 (1.5) |
28 (1.9) |
6 (0.8) |
|
Mild |
26 (1.7) |
11 (1.5) |
27 (1.8) |
6 (0.8) |
|
Moderate |
7 (0.5) |
0 |
1 (0.1) |
0 |
|
Severe |
0 |
0 |
0 |
0 |
|
Diarrheaß |
||||
|
Any |
89 (5.9) |
31 (4.1) |
79 (5.3) |
35 (4.7) |
|
Mild |
79 (5.2) |
31 (4.1) |
72 (4.8) |
32 (4.3) |
|
Moderate |
10 (0.7) |
0 |
7 (0.5) |
3 (0.4) |
|
Severe |
0 |
0 |
0 |
0 |
|
New or worsened muscle pain# |
||||
|
Any |
137 (9.1) |
51 (6.8) |
175 (11.7) |
55 (7.4) |
|
Mild |
96 (6.4) |
35 (4.7) |
116 (7.7) |
38 (5.1) |
|
Moderate |
40 (2.6) |
16 (2.1) |
58 (3.9) |
17 (2.3) |
|
Severe |
1 (0.1) |
0 |
1 (0.1) |
0 |
|
New or worsened joint pain# |
||||
|
Any |
50 (3.3) |
41 (5.5) |
78 (5.2) |
27 (3.6) |
|
Mild |
34 (2.3) |
31 (4.1) |
57 (3.8) |
20 (2.7) |
|
Moderate |
16 (1.1) |
10 (1.3) |
21 (1.4) |
7 (0.9) |
|
Severe |
0 |
0 |
0 |
0 |
|
Use of antipyretic or pain medicationà |
217 (14.4) |
62 (8.3) |
296 (19.7) |
60 (8.1) |
Unsolicited Adverse Events
In the following analyses of Study 3 in children 5 through 11 years of age (1,518 of whom received Pfizer-BioNTech COVID-19 Vaccine (10 mcg modRNA) and 750 of whom received placebo), 99.5% of participants had at least 30 days of follow-up after Dose 2.
Serious Adverse Events
In 1 group of participants (initial enrollment cohort) with a median of 2.3 months follow-up post Dose 2, no serious adverse events were reported that were considered related to vaccination. In a second group of participants (expansion cohort) with a median of 2.4 weeks follow-up post Dose 2, no serious adverse events were reported that were considered related to vaccination.
Non-Serious Adverse Events
In 1 group of participants (initial enrollment cohort), non-serious adverse events from Dose 1 through up to 30 days after Dose 2 up to the cutoff date of September 06, 2021, in ongoing follow-up were reported by 10.9% of Pfizer-BioNTech COVID-19 Vaccine (10 mcg modRNA) recipients and by 9.1% of placebo recipients. In this group of participants, >99% had follow-up 30 days post Dose 2. In a second group of participants (expansion cohort) for which the median follow-up was 2.4 weeks (range 0 to 3.7 weeks), non-serious adverse events from Dose 1 through the cutoff date of October 08, 2021, were reported by 7.1% of Pfizer-BioNTech COVID-19 Vaccine (10 mcg modRNA) recipients and by 6.3% of placebo recipients.
In the initial enrollment cohort, from Dose 1 through 30 days after Dose 2, lymphadenopathy was reported in 13 (0.9%) participants in the Pfizer-BioNTech COVID-19 Vaccine (10 mcg modRNA) group vs. 1 (0.1%) in the placebo group. In the expansion cohort from Dose 1 through the cutoff date, lymphadenopathy was reported in 6 (0.4%) participants in the Pfizer-BioNTech COVID-19 Vaccine (10 mcg modRNA) group vs. 3 (0.4%) in the placebo group. There were no other notable patterns between treatment groups for specific categories of non-serious adverse events that would suggest a causal relationship to Pfizer-BioNTech COVID-19 Vaccine.
Participants 2 Through 4 Years of Age (3-Dose Primary Series)
In an analysis of Study 3 (Phase 2/3), based on data in the blinded placebo-controlled follow-up period up to the cutoff date of April 29, 2022, 886 participants 2 through 4 years of age who received a 3-dose primary series [606 Pfizer-BioNTech COVID-19 Vaccine (3 mcg modRNA); 280 placebo] have been followed a median of 1.4 months after the third dose.
Demographic characteristics in Study 3 were generally similar with regard to age, gender, race, and ethnicity among participants 2 through 4 years of age who received Pfizer-BioNTech COVID-19 Vaccine and those who received placebo. Among the 1,835 participants 2 through 4 years of age who received at least 1 dose of the Pfizer-BioNTech COVID-19 Vaccine, 49.1% were male and 50.9% were female, 80.1% were White, 14.4% were Hispanic/Latino, 7.1% were multi-racial, 6.9% were Asian, 5.1% were Black or African American, and 0.2% were American Indian/Alaska Native.
Solicited Local and Systemic Adverse Reactions
The mean duration of pain at the injection site after Dose 3 was 1.7 days (range 1 to 14 days), for redness 1.5 days (range 1 to 3 days), and for swelling 1.8 days (range 1 to 4 days) for participants 2 through 4 years of age in the Pfizer-BioNTech COVID-19 Vaccine group in the blinded placebo-controlled follow-up period (cutoff date of April 29, 2022).
| Note: Reactions were collected in an electronic diary (e-diary) from Day 1 to Day 7 after vaccination. | ||||||
|
||||||
|
Pfizer-BioNTech COVID-19 Vaccine†
|
Pfizer-BioNTech COVID-19 Vaccine†
|
Pfizer-BioNTech COVID-19 Vaccine†
| ||||
|
Redness¶ | ||||||
|
Any |
160 (8.8) |
77 (8.5) |
202 (11.4) |
50 (5.7) |
60 (10.9) |
9 (3.4) |
|
Mild |
137 (7.5) |
67 (7.4) |
170 (9.6) |
43 (4.9) |
53 (9.6) |
7 (2.7) |
|
Moderate |
22 (1.2) |
9 (1.0) |
31 (1.7) |
7 (0.8) |
7 (1.3) |
2 (0.8) |
|
Severe |
1 (0.1) |
1 (0.1) |
1 (0.1) |
0 |
0 |
0 |
|
Swelling¶ | ||||||
|
Any |
67 (3.7) |
26 (2.9) |
102 (5.7) |
18 (2.1) |
17 (3.1) |
3 (1.1) |
|
Mild |
59 (3.2) |
21 (2.3) |
81 (4.6) |
16 (1.8) |
16 (2.9) |
3 (1.1) |
|
Moderate |
8 (0.4) |
5 (0.6) |
21 (1.2) |
2 (0.2) |
1 (0.2) |
0 |
|
Severe |
0 |
0 |
0 |
0 |
0 |
0 |
|
Pain at the injection site# | ||||||
|
Any |
559 (30.8) |
186 (20.6) |
550 (31.0) |
178 (20.3) |
146 (26.7) |
35 (13.4) |
|
Mild |
522 (28.8) |
178 (19.7) |
514 (29.0) |
169 (19.3) |
130 (23.8) |
33 (12.6) |
|
Moderate |
37 (2.0) |
7 (0.8) |
36 (2.0) |
8 (0.9) |
16 (2.9) |
2 (0.8) |
|
Severe |
0 |
1 (0.1) |
0 |
1 (0.1) |
0 |
0 |
| Note: Events and use of antipyretic or pain medication were collected in an electronic diary (e-diary) from Day 1 to Day 7 after each dose. | ||||||
|
||||||
|
Pfizer-BioNTech COVID-19 Vaccine†
|
Pfizer-BioNTech COVID-19 Vaccine†
|
Pfizer-BioNTech COVID-19 Vaccine†
| ||||
|
Fever | ||||||
|
≥38.0℃ |
95 (5.2) |
48 (5.3) |
88 (4.9) |
46 (5.2) |
28 (5.1) |
11 (4.2) |
|
≥38.0℃ to 38.4℃ |
57 (3.1) |
24 (2.6) |
41 (2.3) |
17 (1.9) |
16 (2.9) |
4 (1.5) |
|
>38.4℃ to 38.9℃ |
24 (1.3) |
16 (1.8) |
26 (1.5) |
21 (2.4) |
8 (1.4) |
4 (1.5) |
|
>38.9℃ to 40.0℃ |
13 (0.7) |
8 (0.9) |
19 (1.1) |
8 (0.9) |
4 (0.7) |
3 (1.1) |
|
>40.0℃ |
1 (0.1) |
0 |
2 (0.1) |
0 |
0 |
0 |
|
Fatigue¶ | ||||||
|
Any |
539 (29.7) |
277 (30.6) |
456 (25.7) |
201 (22.9) |
134 (24.5) |
57 (21.8) |
|
Mild |
335 (18.5) |
176 (19.4) |
267 (15.1) |
120 (13.7) |
87 (15.9) |
35 (13.4) |
|
Moderate |
198 (10.9) |
96 (10.6) |
181 (10.2) |
78 (8.9) |
45 (8.2) |
22 (8.4) |
|
Severe |
6 (0.3) |
5 (0.6) |
8 (0.5) |
3 (0.3) |
2 (0.4) |
0 |
|
Headache¶ | ||||||
|
Any |
81 (4.5) |
44 (4.9) |
81 (4.6) |
36 (4.1) |
27 (4.9) |
11 (4.2) |
|
Mild |
63 (3.5) |
35 (3.9) |
63 (3.6) |
23 (2.6) |
19 (3.5) |
10 (3.8) |
|
Moderate |
18 (1.0) |
8 (0.9) |
18 (1.0) |
12 (1.4) |
8 (1.5) |
1 (0.4) |
|
Severe |
0 |
1 (0.1) |
0 |
1 (0.1) |
0 |
0 |
|
Chills¶ | ||||||
|
Any |
41 (2.3) |
22 (2.4) |
53 (3.0) |
23 (2.6) |
18 (3.3) |
7 (2.7) |
|
Mild |
28 (1.5) |
16 (1.8) |
35 (2.0) |
17 (1.9) |
14 (2.6) |
7 (2.7) |
|
Moderate |
10 (0.6) |
6 (0.7) |
18 (1.0) |
6 (0.7) |
3 (0.5) |
0 |
|
Severe |
3 (0.2) |
0 |
0 |
0 |
1 (0.2) |
0 |
|
Vomiting# | ||||||
|
Any |
54 (3.0) |
24 (2.7) |
61 (3.4) |
29 (3.3) |
9 (1.6) |
10 (3.8) |
|
Mild |
44 (2.4) |
14 (1.5) |
55 (3.1) |
26 (3.0) |
7 (1.3) |
9 (3.4) |
|
Moderate |
10 (0.6) |
10 (1.1) |
6 (0.3) |
3 (0.3) |
2 (0.4) |
1 (0.4) |
|
Severe |
0 |
0 |
0 |
0 |
0 |
0 |
|
DiarrheaÞ | ||||||
|
Any |
139 (7.7) |
72 (8.0) |
118 (6.7) |
64 (7.3) |
28 (5.1) |
13 (5.0) |
|
Mild |
130 (7.2) |
64 (7.1) |
105 (5.9) |
57 (6.5) |
21 (3.8) |
10 (3.8) |
|
Moderate |
9 (0.5) |
8 (0.9) |
12 (0.7) |
7 (0.8) |
7 (1.3) |
3 (1.1) |
|
Severe |
0 |
0 |
1 (0.1) |
0 |
0 |
0 |
|
New or worsened muscle pain¶ | ||||||
|
Any |
43 (2.4) |
15 (1.7) |
46 (2.6) |
21 (2.4) |
11 (2.0) |
4 (1.5) |
|
Mild |
33 (1.8) |
13 (1.4) |
33 (1.9) |
17 (1.9) |
8 (1.5) |
4 (1.5) |
|
Moderate |
9 (0.5) |
2 (0.2) |
13 (0.7) |
4 (0.5) |
3 (0.5) |
0 |
|
Severe |
1 (0.1) |
0 |
0 |
0 |
0 |
0 |
|
New or worsened joint pain¶ | ||||||
|
Any |
14 (0.8) |
18 (2.0) |
24 (1.4) |
9 (1.0) |
7 (1.3) |
2 (0.8) |
|
Mild |
12 (0.7) |
13 (1.4) |
18 (1.0) |
6 (0.7) |
5 (0.9) |
2 (0.8) |
|
Moderate |
2 (0.1) |
5 (0.6) |
6 (0.3) |
3 (0.3) |
1 (0.2) |
0 |
|
Severe |
0 |
0 |
0 |
0 |
1 (0.2) |
0 |
|
Use of antipyretic or pain medicationß |
197 (10.8) |
83 (9.1) |
177 (9.9) |
74 (8.4) |
47 (8.5) |
18 (6.9) |
Unsolicited Adverse Events
In the following analyses of Study 3 in participants 2 through 4 years of age (606 of whom received Pfizer-BioNTech COVID-19 Vaccine and 280 of whom received placebo), 76.6% of participants had at least 30 days of follow-up after Dose 3.
Serious Adverse Events
Serious adverse events from Dose 1 through 1 month after Dose 3, with an overall median of 1.4 months follow-up after Dose 3 were reported by 0.7% of Pfizer-BioNTech COVID-19 Vaccine recipients and by 0.9% of placebo recipients. One serious adverse event of fever (maximum temperature 40.3°C) on Day 3 after Dose 2 in a 4-year-old was considered possibly related to vaccination.
Non-Serious Adverse Events
Non-serious adverse events from Dose 1 through up to 30 days after Dose 3, in ongoing follow-up were reported by 18.5% of Pfizer-BioNTech COVID-19 Vaccine recipients and by 18.5% of placebo recipients.
From Dose 1 through 30 days after Dose 3, lymphadenopathy was reported in 1 (0.1%) participant in the Pfizer-BioNTech COVID-19 Vaccine (3 mcg modRNA) group vs. 0 (0.0%) in the placebo group. There were no other notable patterns between treatment groups for specific categories of non-serious adverse events that would suggest a causal relationship to Pfizer-BioNTech COVID-19 Vaccine.
Participants 6 Through 23 Months of Age (3-Dose Primary Series)
In an analysis of Study 3 (Phase 2/3), based on data in the blinded placebo-controlled follow-up period up to the cutoff date of April 29, 2022, 570 participants 6 through 23 months of age who received a 3-dose primary series [386 Pfizer-BioNTech COVID-19 Vaccine (3 mcg modRNA); 184 placebo] have been followed for a median of 1.3 months after the third dose.
Demographic characteristics in Study 3 were generally similar with regard to age, gender, race, and ethnicity among participants 6 through 23 months of age who received Pfizer-BioNTech COVID-19 Vaccine and those who received placebo. Among the 1,178 participants 6 through 23 months of age who received at least 1 dose of the Pfizer-BioNTech COVID-19 Vaccine, 50.0% were male and 50.0% were female, 78.3% were White, 9.9% were multi-racial, 13.7% were Hispanic/Latino, 7.7% were Asian, 3.6% were Black or African American, and 0.3% were American Indian/Alaska Native.
Solicited Local and Systemic Adverse Reactions
The mean duration of tenderness at the injection site after Dose 3 was 1.5 days (range 1 to 9 days), for redness 1.5 days (range 1 to 5 days), and for swelling 1.8 days (range 1 to 3 days) for participants 6 through 23 months of age in the Pfizer-BioNTech COVID-19 Vaccine group in the blinded placebo-controlled follow-up period (cutoff date of April 29, 2022).
| Note: Reactions were collected in an electronic diary (e-diary) from Day 1 to Day 7 after vaccination. | ||||||
|
||||||
|
Pfizer-BioNTech COVID-19 Vaccine†
|
Pfizer-BioNTech COVID-19 Vaccine†
|
Pfizer-BioNTech COVID-19 Vaccine†
| ||||
|
Redness¶ |
||||||
|
Any |
124 (10.6) |
44 (7.4) |
107 (9.3) |
39 (6.6) |
26 (7.1) |
9 (5.3) |
|
Mild |
114 (9.7) |
41 (6.9) |
97 (8.5) |
36 (6.1) |
17 (4.7) |
8 (4.7) |
|
Moderate |
10 (0.9) |
3 (0.5) |
10 (0.9) |
3 (0.5) |
8 (2.2) |
1 (0.6) |
|
Severe |
0 |
0 |
0 |
0 |
1 (0.3) |
0 |
|
Swelling¶ |
||||||
|
Any |
46 (3.9) |
15 (2.5) |
45 (3.9) |
9 (1.5) |
10 (2.7) |
3 (1.8) |
|
Mild |
40 (3.4) |
13 (2.2) |
39 (3.4) |
8 (1.4) |
7 (1.9) |
3 (1.8) |
|
Moderate |
6 (0.5) |
2 (0.3) |
6 (0.5) |
1 (0.2) |
3 (0.8) |
0 |
|
Severe |
0 |
0 |
0 |
0 |
0 |
0 |
|
Tenderness at the injection site# |
||||||
|
Any |
192 (16.6) |
66 (11.2) |
171 (15.0) |
50 (8.5) |
58 (16.0) |
20 (11.8) |
|
Mild |
181 (15.6) |
61 (10.3) |
154 (13.5) |
42 (7.1) |
51 (14.1) |
17 (10.0) |
|
Moderate |
11 (0.9) |
5 (0.8) |
16 (1.4) |
8 (1.4) |
7 (1.9) |
3 (1.8) |
|
Severe |
0 |
0 |
1 (0.1) |
0 |
0 |
0 |
| Note: Events and use of antipyretic or pain medication were collected in an electronic diary (e-diary) from Day 1 to Day 7 after each dose. | ||||||
|
||||||
|
Pfizer-BioNTech COVID-19 Vaccine†
|
Pfizer-BioNTech COVID-19 Vaccine†
|
Pfizer-BioNTech COVID-19 Vaccine†
| ||||
|
Fever |
||||||
|
≥38.0℃ |
85 (7.2) |
43 (7.2) |
85 (7.4) |
36 (6.1) |
25 (6.8) |
10 (5.9) |
|
≥38.0℃ to 38.4℃ |
42 (3.6) |
22 (3.7) |
41 (3.6) |
18 (3.0) |
14 (3.8) |
7 (4.1) |
|
>38.4℃ to 38.9℃ |
23 (2.0) |
14 (2.4) |
20 (1.7) |
11 (1.9) |
5 (1.4) |
2 (1.2) |
|
>38.9℃ to 40.0℃ |
19 (1.6) |
6 (1.0) |
23 (2.0) |
7 (1.2) |
5 (1.4) |
1 (0.6) |
|
>40.0℃ |
1 (0.1) |
1 (0.2) |
1 (0.1) |
0 |
1 (0.3) |
0 |
|
Decreased appetite¶ |
||||||
|
Any |
257 (22.2) |
125 (21.2) |
252 (22.2) |
106 (18.0) |
73 (20.2) |
23 (13.5) |
|
Mild |
138 (11.9) |
73 (12.4) |
157 (13.8) |
63 (10.7) |
42 (11.6) |
13 (7.6) |
|
Moderate |
116 (10.0) |
51 (8.6) |
91 (8.0) |
42 (7.1) |
27 (7.5) |
10 (5.9) |
|
Severe |
3 (0.3) |
1 (0.2) |
4 (0.4) |
1 (0.2) |
4 (1.1) |
0 |
|
Drowsiness# |
||||||
|
Any |
313 (27.0) |
173 (29.3) |
271 (23.8) |
125 (21.2) |
72 (19.9) |
22 (12.9) |
|
Mild |
251 (21.7) |
130 (22.0) |
201 (17.7) |
98 (16.6) |
50 (13.8) |
15 (8.8) |
|
Moderate |
60 (5.2) |
41 (6.9) |
66 (5.8) |
26 (4.4) |
21 (5.8) |
6 (3.5) |
|
Severe |
2 (0.2) |
2 (0.3) |
4 (0.4) |
1 (0.2) |
1 (0.3) |
1 (0.6) |
|
IrritabilityÞ |
||||||
|
Any |
593 (51.2) |
279 (47.2) |
539 (47.4) |
240 (40.7) |
158 (43.6) |
64 (37.6) |
|
Mild |
245 (21.1) |
106 (17.9) |
213 (18.7) |
89 (15.1) |
56 (15.5) |
27 (15.9) |
|
Moderate |
341 (29.4) |
173 (29.3) |
319 (28.1) |
146 (24.7) |
101 (27.9) |
37 (21.8) |
|
Severe |
7 (0.6) |
0 |
7 (0.6) |
5 (0.8) |
1 (0.3) |
0 |
|
Use of antipyretic or pain medicationß |
281 (24.0) |
117 (19.7) |
243 (21.2) |
111 (18.8) |
70 (19.2) |
28 (16.5) |
Unsolicited Adverse Events
In the following analyses of Study 3 in participants 6 through 23 months of age (386 of whom received Pfizer-BioNTech COVID-19 Vaccine and 184 of whom received placebo), 83.7% of participants had at least 30 days of follow-up after Dose 3.
Serious Adverse Events
Serious adverse events from Dose 1 through 1 month after Dose 3, with an overall median of 1.3 months follow-up after Dose 3 were reported by 1.4% of Pfizer-BioNTech COVID-19 Vaccine recipients and by 2.3% of placebo recipients. No serious adverse events were reported that were considered related to vaccination.
Non-Serious Adverse Events
Non-serious adverse events from Dose 1 through up to 1 month after Dose 3, in ongoing follow-up were reported by 29.1% of Pfizer-BioNTech COVID-19 Vaccine recipients and by 26.3% of placebo recipients.
From Dose 1 through 30 days after Dose 3, lymphadenopathy was reported in 2 (0.2%) participants in the Pfizer-BioNTech COVID-19 Vaccine group vs. 0 (0%) in the placebo group. There were no other notable patterns between treatment groups for specific categories of non-serious adverse events that would suggest a causal relationship to Pfizer-BioNTech COVID-19 Vaccine.
Pfizer-BioNTech COVID-19 Vaccine (Original Monovalent) Administered as a First Booster Dose Following a Primary Series of Pfizer-BioNTech COVID-19 Vaccine (Original Monovalent) or COMIRNATY (COVID-19 Vaccine, mRNA) in Participants 18 through 55 Years of Age
A subset of Study 2 Phase 2/3 participants of 306 participants 18 through 55 years of age received a first booster dose of Pfizer-BioNTech COVID-19 Vaccine (30 mcg modRNA) approximately 6 months (range of 4.8 to 8.0 months) after completing the primary series. Additionally, a total of 23 Study 2 (Phase 1) participants (11 participants 18 through 55 years of age and 12 participants 65 through 85 years of age) received a first booster dose of Pfizer-BioNTech COVID-19 Vaccine approximately 8 months (range 7.9 to 8.8 months) after completing the primary series. Participants are being monitored for unsolicited adverse events through 1 month after vaccination and for serious adverse events for 6 months after the last vaccination.
Among the 306 Phase 2/3 participants, the median age was 42 years (range 19 through 55 years of age), 45.8% were male and 54.2% were female, 81.4% were White, 27.8% were Hispanic/Latino, 9.2% were Black or African American, 5.2% were Asian, and 0.7% were American Indian/Alaska Native. Among the 12 Phase 1 participants 65 through 85 years of age, the median age was 69 years (range 65 through 75 years of age), 6 were male and all were White and Not Hispanic/Latino. Following the booster dose, the median follow-up time was 2.6 months (range 2.1 to 2.9 months) for Phase 1 participants and 2.6 months (range 1.1 to 2.8 months) for Phase 2/3 participants.
Unsolicited Adverse Events
Overall, the 306 participants who received a first booster dose, had a median follow-up time of 2.6 months after the booster dose to the cutoff date (June 17, 2021).
In an analysis of all unsolicited adverse events reported following the first booster dose, through 1 month after the booster dose, in participants 18 through 55 years of age (N=306), those assessed as adverse reactions not already captured by solicited local and systemic reactions were lymphadenopathy (n=16, 5.2%), nausea (n=2, 0.7%), decreased appetite (n=1, 0.3%), rash (n=1, 0.3%), and pain in extremity (n=1, 0.3%).
Serious Adverse Events
Of the 306 participants who received a first booster dose of Pfizer-BioNTech COVID-19 Vaccine, there were no serious adverse events reported from the booster dose through 30 days after the booster dose. One participant reported a serious adverse event 61 days after the booster dose that was assessed as unrelated to vaccination.
First Booster Dose Following a Primary Series of Pfizer-BioNTech COVID-19 Vaccine (Original Monovalent) in Participants 5 Through 11 Years of Age
A subset of Study 3 Phase 2/3 participants 5 through 11 years of age received a first booster dose of Pfizer-BioNTech COVID-19 Vaccine (10 mcg modRNA) at least 5 months after completing the primary series (range 5 to 9 months, 86.8% of participants received a booster dose at least 8 months after Dose 2). Those participants vaccinated prior to February 22, 2022, provided the safety database (n=401), and had a median safety follow-up of 1.3 months from vaccination through the data cutoff date of March 22, 2022.
The median age of these 401 participants was 8.0 years (range 5 through 11 years of age), 52.4% were male and 47.6% were female, 70.1% were White, 7.2% were Black or African American, 22.9% were Hispanic/Latino, 7.7% were Asian, and 2.0% were American Indian/Alaska Native.
Solicited Local and Systemic Adverse Reactions
Table 8 and Table 9 present the frequency and severity of reported solicited local and systemic reactions, respectively, within 7 days of a booster dose of Pfizer-BioNTech COVID-19 Vaccine for Phase 2/3 participants 5 through 11 years of age.
In participants who received a booster dose, the mean duration of pain at the injection site after the booster dose was 2.4 days (range 1 to 35 days), for redness 2.3 days (range 1 to 12 days), and for swelling 2.3 days (range 1 to 9 days).
| Pfizer-BioNTech COVID-19 Vaccine†
Booster N‡=371 n§ (%) |
|
|---|---|
| Note: Reactions were collected in the e-diary and unscheduled clinical assessments from Day 1 through Day 7 after vaccination. | |
|
|
|
Redness¶ |
|
|
Any (≥0.5 cm) |
58 (15.6) |
|
Mild |
38 (10.2) |
|
Moderate |
19 (5.1) |
|
Severe |
1 (0.3) |
|
Swelling¶ |
|
|
Any (≥0.5 cm) |
61 (16.4) |
|
Mild |
30 (8.1) |
|
Moderate |
31 (8.4) |
|
Severe |
0 |
|
Pain at the injection site# |
|
|
Any |
274 (73.9) |
|
Mild |
177 (47.7) |
|
Moderate |
95 (25.6) |
|
Severe |
2 (0.5) |
| Note: Events and use of antipyretic or pain medication were collected in the e-diary and unscheduled clinical assessments from Day 1 through Day 7 after vaccination. | |
|
|
|
Solicited Systemic Reaction | |
|
Fever |
|
|
≥38.0°C |
25 (6.7) |
|
≥38.0°C to 38.4°C |
17 (4.6) |
|
>38.4°C to 38.9°C |
5 (1.3) |
|
>38.9°C to 40.0°C |
3 (0.8) |
|
>40.0°C |
0 |
|
Fatigue¶ |
|
|
Any |
169 (45.6) |
|
Mild |
99 (26.7) |
|
Moderate |
63 (17.0) |
|
Severe |
7 (1.9) |
|
Headache¶ |
|
|
Any |
126 (34.0) |
|
Mild |
76 (20.5) |
|
Moderate |
47 (12.7) |
|
Severe |
0 |
|
Chills¶ |
|
|
Any |
39 (10.5) |
|
Mild |
23 (6.2) |
|
Moderate |
15 (4.0) |
|
Severe |
1 (0.3) |
|
Vomiting# |
|
|
Any |
9 (2.4) |
|
Mild |
6 (1.6) |
|
Moderate |
3 (0.8) |
|
Severe |
0 |
|
DiarrheaÞ |
|
|
Any |
18 (4.9) |
|
Mild |
15 (4.0) |
|
Moderate |
2 (0.5) |
|
Severe |
1 (0.3) |
|
New or worsened muscle pain¶ |
|
|
Any |
68 (18.3) |
|
Mild |
40 (10.8) |
|
Moderate |
28 (7.5) |
|
Severe |
0 |
|
New or worsened joint pain¶ |
|
|
Any |
25 (6.7) |
|
Mild |
14 (3.8) |
|
Moderate |
11 (3.0) |
|
Severe |
0 |
|
Use of antipyretic or pain medicationß |
114 (30.7) |
Unsolicited Adverse Events
Overall, the 401 participants who received a first booster dose of Pfizer-BioNTech COVID-19 Vaccine had a median follow-up time of 1.3 months after the booster dose through the cutoff date.
In an analysis of all unsolicited adverse events reported in participants 5 through 11 years of age (N=401) through up to 1 month after a first booster dose, lymphadenopathy (n=10, 2.5%) was an adverse reaction not already captured by solicited local and systemic reactions.
Serious Adverse Events
No serious adverse events were reported after the first booster dose through the cutoff date.
Pfizer-BioNTech COVID-19 Vaccine (Original Monovalent) Administered as a First Booster Dose Following Vaccination with Another Authorized or Approved COVID-19 Vaccine
The safety of a Pfizer-BioNTech COVID-19 Vaccine booster dose in individuals who completed primary vaccination with another authorized or approved COVID-19 Vaccine (heterologous booster dose) is inferred from the safety of a Pfizer-BioNTech COVID-19 Vaccine (30 mcg modRNA) booster dose administered following completion of Pfizer-BioNTech COVID-19 Vaccine primary series (homologous booster dose) and from data from an independent National Institutes of Health (NIH) study Phase 1/2 open-label clinical trial (NCT04889209) conducted in the United States that evaluated a heterologous booster dose of the Pfizer-BioNTech COVID-19 Vaccine. In this study, participants who had completed primary vaccination with a Moderna COVID-19 Vaccine 2-dose series (N=151), a Janssen COVID-19 Vaccine single dose (N=156), or a Pfizer-BioNTech COVID-19 Vaccine 2-dose series (N=151) at least 12 weeks prior to enrollment and who reported no history of SARS-CoV-2 infection were randomized 1:1:1 to receive a booster dose of 1 of 3 vaccines: Moderna COVID-19 Vaccine, Janssen COVID-19 Vaccine, or Pfizer-BioNTech COVID-19 Vaccine. Adverse events were assessed through 28 days after the booster dose. An overall review of adverse reactions reported in the study following the Pfizer-BioNTech COVID-19 Vaccine heterologous booster dose did not identify any new safety concerns, as compared with adverse reactions reported following Pfizer-BioNTech COVID-19 Vaccine primary series doses or a homologous booster dose.
Pfizer-BioNTech COVID-19 Vaccine (Original Monovalent) Administered as a Second Booster Dose Following Primary and Booster Vaccination with Another Authorized or Approved COVID-19 Vaccine
Safety surveillance data from the Ministry of Health of Israel on the administration of approximately 700,000 fourth doses of the Pfizer-BioNTech COVID-19 Vaccine (30 mcg modRNA) given at least 4 months after the third dose in participants 18 years of age and older (approximately 600,000 of whom were 60 years of age and older) revealed no new safety concerns.
Pfizer-BioNTech COVID-19 Vaccine, Bivalent (Original and Omicron BA.4/BA.5)
Study 5 (NCT05472038) enrolled participants 12 years of age and older to receive a booster (fourth dose) of Pfizer-BioNTech COVID-19 Vaccine, Bivalent (30 mcg modRNA). In Study 5, all participants 12 years of age and older are being monitored for safety throughout the study [through 6 months after the booster (fourth dose)].
Study 6 (NCT05543616) enrolled participants 6 months through 11 years of age to receive a booster (fourth dose) of Pfizer-BioNTech COVID-19 Vaccine, Bivalent.
In Study 6, all participants 6 months through 4 years of age were monitored for solicited local and systemic reactions and use of antipyretic medication after the vaccination in an electronic diary. Participants are being monitored for safety throughout the study [through 6 months after the booster (fourth dose)]. Tables 10 through 13 present the frequency and severity of solicited local and systemic reactions, within 7 days following a booster (fourth dose) of Pfizer-BioNTech COVID-19 Vaccine, Bivalent in participants 6 through 23 months of age and 2 through 4 years of age who were previously vaccinated with a 3-dose primary series of Pfizer-BioNTech COVID-19 Vaccine (Original monovalent).
Participants 12 Years of Age and Older Who Received a Booster Dose with Pfizer-BioNTech COVID-19 Vaccine, Bivalent (Original and Omicron BA.4/BA.5)
A subset of Study 5 Phase 2/3 participants 12 through 17 years of age (n=107), 18 through 55 years of age (n=103) and 56 years of age and older (n=106) previously vaccinated with a 2-dose primary series and 1 booster dose of Pfizer-BioNTech COVID-19 Vaccine (Original monovalent, 30 mcg modRNA), received a second booster dose with Pfizer-BioNTech COVID-19 Vaccine, Bivalent (Original and Omicron BA.4/BA.5) (30 mcg modRNA).
The participants received the second booster dose a median of 9.9 months (range 5.5 to 14.3 months) after receiving the first booster dose and had a median follow-up time of 1.6 months up to a data cutoff date of October 12, 2022. The median age was 40.0 years, 53.2% were male, 46.8% were female, 81.3% were White, 9.2% were Hispanic/Latino, 5.1% were Asian, and 10.8% were Black or African American.
Unsolicited Adverse Events
In the following analysis of Study 5, 316 participants 12 years of age and older who received a second booster of Pfizer-BioNTech COVID-19 Vaccine, Bivalent had a median follow-up time of 1.6 months (range 1.3 to 1.8 months) to the cutoff date October 12, 2022.
Serious Adverse Events
Serious adverse events were reported in the 1 participant (considered unrelated to the vaccine) from the study vaccination through 1 month post vaccination.
Non-Serious Adverse Events
Lymphadenopathy 2 days post-vaccination, considered related to vaccination, was reported in 1 (0.3%) participant 12 years of age and older.
Participants 5 Through 11 Years of Age Who Received a Booster Dose with Pfizer-BioNTech COVID-19 Vaccine, Bivalent (Original and Omicron BA.4/BA.5)
In Study 6, 113 participants 5 through 11 years of age previously vaccinated with a 2-dose primary series and 1 booster dose of Pfizer-BioNTech COVID-19 Vaccine (Original monovalent, 10 mcg modRNA) received a booster (fourth dose) with Pfizer-BioNTech COVID-19 Vaccine, Bivalent (Original and Omicron BA.4/BA.5) (10 mcg modRNA).
Participants received a booster (fourth dose) with Pfizer-BioNTech COVID-19, Bivalent 2.6 to 8.5 months after receiving their third dose with Pfizer-BioNTech COVID-19 Vaccine (Original monovalent) and had a median follow-up time of 1.6 months (range 1.1 to 2.3 months) up to a data cutoff date of November 25, 2022. Their median age was 9 years (range 5 through 11 years of age), 50.4% were male and 49.6% were female, 58.4% were White, 20.4% were Hispanic/Latino, 19.5% were multi-racial, 11.5% were Asian, and 8.0% were Black or African American.
Unsolicited Adverse Events
In the following analysis of Study 6, 113 participants 5 through 11 years of age who received a booster (fourth dose) with the Pfizer-BioNTech COVID-19 Vaccine, Bivalent had a median follow-up time of 1.6 months (range 1.1 to 2.3 months) to the cutoff date (November 25, 2022).
Serious Adverse Events
No serious adverse events were reported in the 113 participants 5 through 11 years of age from the study vaccination through 1 month post vaccination.
Non-Serious Adverse Events
Lymphadenopathy 2 days post-vaccination, considered related to vaccination, was reported in 1 (0.9%) participant 5 through 11 years of age.
Participants 2 Through 4 Years of Age Who Received a Booster Dose with Pfizer-BioNTech COVID-19 Vaccine, Bivalent (Original and Omicron BA.4/BA.5)
In a subset of Study 6, 36 participants 2 through 4 years of age previously vaccinated with a 3-dose primary series of Pfizer-BioNTech COVID-19 Vaccine (Original monovalent, 3 mcg modRNA) received a booster (fourth dose) with Pfizer-BioNTech COVID-19 Vaccine, Bivalent (Original and Omicron BA.4/BA.5) (3 mcg modRNA).
Participants received a booster (fourth dose) with Pfizer-BioNTech COVID-19 Vaccine, Bivalent 2.2 to 8.5 months after receiving their third dose with Pfizer-BioNTech COVID-19 Vaccine (Original monovalent) and had a median follow-up time of 1.9 months (range 1.6 to 2.3 months) up to a data cutoff date of November 25, 2022. Their median age was 2 years (range 2 through 4 years of age), 55.6% were male and 44.4% were female, 61.1% were White, 30.6% were Hispanic/Latino, 22.2% were multi-racial, 11.1% were Asian, and 5.6% were Black or African American.
Solicited Local and Systemic Adverse Reactions
Table 10 and Table 11 present the frequency and severity of reported solicited local reactions and systemic reactions, respectively, within 7 days of a booster (fourth dose) of Pfizer-BioNTech COVID-19 Vaccine, Bivalent.
The mean duration of pain at the injection site was 1.1 days (range 1 to 2 days), for redness 1.3 days (range 1 to 2 days), and for swelling 3 days for participants 2 through 4 years of age.
Table 10: Local Adverse Reactions, by Maximum Severity, Within 7 Days After a Booster (Fourth Dose) – Participants 2 through 4 Years of Age – Safety Population
| Note: Reactions were collected in the electronic diary (e-diary) and at unscheduled clinical assessments from Day 1 through Day 7 after the study vaccination. Reactions reported as adverse events in the case report form within 7 days after the study vaccination were also included in the analysis; the severity of these events is based on the grading scale in the adverse event section of the case report form. | |
|
|
|
Pfizer-BioNTech COVID-19 Vaccine, Bivalent (Original and Omicron BA.4/BA.5) 3 mcg modRNA N*=36 n† (%) |
|
|
Redness‡ | |
|
Any (≥0.5 cm) |
3 (8.3) |
|
Mild |
2 (5.6) |
|
Moderate |
1 (2.8) |
|
Swelling‡ | |
|
Any (≥0.5 cm) |
1 (2.8) |
|
Mild |
0 |
|
Moderate |
1 (2.8) |
|
Pain at the injection site§ | |
|
Any |
10 (27.8) |
|
Mild |
8 (22.2) |
|
Moderate |
2 (5.6) |
Table 11: Frequency and Percentages of Participants with Solicited Systemic Reactions, by Maximum Severity, Within 7 Days After a Booster (Fourth Dose) – Participants 2 Through 4 Years of Age – Safety Population
| Note: Events and use of antipyretic or pain medication were collected in the electronic diary (e-diary) and at unscheduled clinical assessments from Day 1 through Day 7 after the study vaccination. Events reported as adverse events in the case report form within 7 days after the study vaccination were also included in the analysis; the severity of these events is based on the grading scale in the adverse event section of the case report form. | |
|
|
|
Pfizer-BioNTech COVID-19 Vaccine, Bivalent (Original and Omicron BA.4/BA.5) 3 mcg modRNA N*=36 n† (%) |
|
|
Fever |
|
|
≥38.0℃ |
0 |
|
Fatigue‡ |
|
|
Any |
11 (30.6) |
|
Mild |
6 (16.7) |
|
Moderate |
5 (13.9) |
|
Headache‡ |
|
|
Any |
1 (2.8) |
|
Mild |
1 (2.8) |
|
Chills‡ |
|
|
Any |
1 (2.8) |
|
Mild |
1 (2.8) |
|
Vomiting§ |
|
|
Any |
1 (2.8) |
|
Mild |
1 (2.8) |
|
Diarrhea¶ |
|
|
Any |
2 (5.6) |
|
Mild |
1 (2.8) |
|
Moderate |
1 (2.8) |
|
New or worsened muscle pain‡ |
|
|
Any |
0 |
|
New or worsened joint pain‡ |
|
|
Any |
1 (2.8) |
|
Mild |
1 (2.8) |
|
Use of antipyretic or pain medication# |
1 (2.8) |
Unsolicited Adverse Events
Participants 2 through 4 years of age who received a booster (fourth dose) with the Pfizer-BioNTech COVID-19 Vaccine, Bivalent had a median follow-up time of 1.9 months (range 1.6 to 2.3 months) to the cutoff date (November 25, 2022).
Serious Adverse Events
No serious adverse events were reported in the 36 participants 2 through 4 years of age from the study vaccination through 1 month post vaccination.
Participants 6 Through 23 Months of Age Who Received a Booster Dose with Pfizer-BioNTech COVID-19 Vaccine, Bivalent (Original and Omicron BA.4/BA.5)
In a subset of Study 6, 24 participants 6 through 23 months previously vaccinated with a 3-dose primary series of Pfizer-BioNTech COVID-19 Vaccine (Original monovalent, 3 mcg modRNA) received a booster (fourth dose) of Pfizer-BioNTech COVID-19 Vaccine, Bivalent (Original and Omicron BA.4/BA.5) (3 mcg modRNA).
Participants received a booster dose with Pfizer-BioNTech COVID-19 Vaccine, Bivalent 2.1 to 8.6 months after receiving their third dose with Pfizer-BioNTech COVID-19 and had a median follow-up time of 1.6 months (range 1.5 to 2.3 months) up to a data cutoff date of November 25, 2022. Their median age was 19 months (range 12 through 23 months), 58.3% were female and 41.7% were male, 54.2% were White, 20.8% were Asian, 20.8% were multi-racial, 16.7% were Hispanic/Latino, and 4.2% were Black or African American.
Solicited Local and Systemic Adverse Reactions
Table 12 and Table 13 present the frequency and severity of reported solicited local reactions and systemic reactions, respectively, within 7 days of a booster (fourth dose) of Pfizer-BioNTech COVID-19 Vaccine, Bivalent.
The duration of injection site tenderness, swelling and redness for all events observed was 1 day.
Table 12: Local Adverse Reactions, by Maximum Severity, Within 7 Days After a Booster (Fourth Dose) – Participants 6 Through 23 Months of Age – Safety Population
| Note: Reactions were collected in the electronic diary (e-diary) and at unscheduled clinical assessments from Day 1 through Day 7 after the study vaccination. Reactions reported as adverse events in the case report form within 7 days after the study vaccination were also included in the analysis; the severity of these events is based on the grading scale in the adverse event section of the case report form. | |
|
|
|
Pfizer-BioNTech COVID-19 Vaccine, Bivalent (Original and Omicron BA.4/BA.5) 3 mcg modRNA n‡ (%) |
|
|
Redness§ | |
|
Any (≥0.5 cm) |
2 (8.3) |
|
Mild |
2 (8.3) |
|
Swelling§ | |
|
Any (≥0.5 cm) |
1 (4.2) |
|
Mild |
1 (4.2) |
|
Tenderness at the injection site¶ | |
|
Any |
1 (4.3) |
|
Mild |
1 (4.3) |
Table 13: Frequency and Percentages of Participants with Solicited Systemic Reactions, by Maximum Severity, Within 7 Days After a Booster (Fourth Dose) – Participants 6 Through 23 Months of Age – Safety Population
| Note: Events and use of antipyretic or pain medication were collected in the electronic diary (e-diary) and at unscheduled clinical assessments from Day 1 through Day 7 after the study vaccination. Events reported as adverse events in the case report form within 7 days after the study vaccination were also included in the analysis; the severity of these events is based on the grading scale in the adverse event section of the case report form. | |
|
|
|
Pfizer-BioNTech COVID-19 Vaccine, Bivalent (Original and Omicron BA.4/BA.5) 3 mcg modRNA n‡ (%) |
|
|
Fever§ |
|
|
≥38.0℃ |
1 (4.2) |
|
≥38.0℃ to 38.4℃ |
1 (4.2) |
|
Decreased appetite¶ |
|
|
Any |
1 (4.5) |
|
Mild |
1 (4.5) |
|
Drowsiness# |
|
|
Any |
2 (9.1) |
|
Mild |
2 (9.1) |
|
IrritabilityÞ |
|
|
Any |
4 (18.2) |
|
Mild |
3 (13.6) |
|
Moderate |
1 (4.5) |
|
Use of antipyretic or pain medicationß |
2 (8.3) |
Unsolicited Adverse Events
Participants 6 through 23 months of age who received a booster (fourth dose) with the Pfizer-BioNTech COVID-19 Vaccine, Bivalent had a median follow-up time of 1.6 months (range 1.5 to 2.3 months) to the cutoff date (November 25, 2022). In an analysis of all unsolicited adverse events reported following the booster dose through 1 month after the booster dose, the adverse reaction not already captured by solicited local and systemic reactions was injection site pain (n=1; 4.2%).
Serious Adverse Events
No serious adverse events were reported in the 24 participants 6 through 23 months of age from the study vaccination through 1 month post vaccination.
Non-Serious Adverse Events
Non-serious adverse events in participants 6 through 23 months of age from the study vaccination through 1 month post vaccination were reported in 3 (12.5%) Pfizer-BioNTech COVID-19 Vaccine, Bivalent recipients. Non-serious adverse events considered related to vaccination by the study investigator were fatigue (n=1; 4.2%) and injection site pain (n=1; 4.2%).
Bivalent Vaccine (Original and Omicron BA.1)
Bivalent Vaccine (Original and Omicron BA.1) Administered as a Second Booster Dose
In Study 4, a total of 610 participants greater than 55 years of age previously vaccinated with a 2-dose primary series and 1 booster dose of Pfizer-BioNTech COVID-19 Vaccine (Original monovalent) went on to receive a second booster dose with either Pfizer-BioNTech COVID-19 Vaccine (Original monovalent) or the bivalent vaccine (Original and Omicron BA.1).
The 305 participants greater than 55 years who received a second booster dose with Pfizer-BioNTech COVID-19 Vaccine (Original monovalent) received it 5.3 to 13.1 months after receiving the first booster dose and had a median follow-up time of 1.8 months up to a data cutoff date of May 16, 2022. Their median age was 66 years (range 56 through 87 years of age), 47.5% were male and 52.5% were female, 87.9% were White, 18.7% were Hispanic/Latino, 4.3% were Asian, and 6.2% were Black or African American.
The 305 participants greater than 55 years who received a second booster dose with the bivalent vaccine (Original and Omicron BA.1) received it 4.7 to 11.5 months after receiving the first booster dose and had a median follow-up time of 1.7 months up to a data cutoff date of May 16, 2022. Their median age was 67 years (range 56 through 85 years of age), 53.1% were male and 46.9% were female, 89.8% were White, 14.8% were Hispanic/Latino, 5.2% were Asian, and 4.3% were Black or African American.
Unsolicited Adverse Events
Overall, the participants who received a second booster dose with the bivalent vaccine (Original and Omicron BA.1) had a median follow-up time of 1.7 months (range 1.0 to 2.0 months) to the cutoff date (May 16, 2022).
In an analysis of all unsolicited adverse events reported following the second booster dose, through 1 month after the booster dose, those assessed as adverse reactions not already captured by solicited local and systemic reactions were lymphadenopathy (n=1, 0.3%) for the Pfizer-BioNTech COVID-19 Vaccine (Original monovalent) and (n=1, 0.3%) for the bivalent vaccine (Original and Omicron BA.1), nausea (n=1, 0.3%) for the Pfizer-BioNTech COVID-19 Vaccine (Original monovalent) and (n=1, 0.3%) for the bivalent vaccine (Original and Omicron BA.1), and malaise (n=0) for the Pfizer-BioNTech COVID-19 Vaccine (Original monovalent) and (n=1, 0.3%) for the bivalent vaccine (Original and Omicron BA.1).
Serious Adverse Events
Serious adverse events up to 1 month after the second booster dose in ongoing follow-up were reported by no Pfizer-BioNTech COVID-19 Vaccine (Original monovalent) recipients and by 1 bivalent vaccine (Original and Omicron BA.1) recipient (1 serious adverse event considered unrelated to the vaccine).
6.2 Postmarketing Experience
The following adverse reactions have been identified during postmarketing use of COMIRNATY, Pfizer-BioNTech COVID-19 Vaccine and Pfizer-BioNTech COVID-19 Vaccine, Bivalent. Because these reactions are reported voluntarily, it is not always possible to reliably estimate their frequency or establish a causal relationship to vaccine exposure.
Cardiac Disorders: myocarditis, pericarditis
Gastrointestinal Disorders: diarrhea, vomiting
Immune System Disorders: severe allergic reactions, including anaphylaxis, and other hypersensitivity reactions (e.g., rash, pruritus, urticaria, angioedema)
Musculoskeletal and Connective Tissue Disorders: pain in extremity (arm)
Nervous System Disorders: syncope, dizziness, febrile seizures
6.3 Required Reporting for Adverse Events and Vaccine Administration Errors
Vaccination providers must report the listed events following administration of the Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula)9 to the Vaccine Adverse Event Reporting System (VAERS)
- •
- Vaccine administration errors whether or not associated with an adverse event
- •
- Serious adverse events* (irrespective of attribution to vaccination)
- •
- Cases of myocarditis
- •
- Cases of pericarditis
- •
- Cases of Multisystem Inflammatory Syndrome (MIS)
- •
- Cases of COVID-19 that results in hospitalization or death
*Serious Adverse Events are defined as:
- •
- Death;
- •
- A life-threatening adverse event;
- •
- Inpatient hospitalization or prolongation of existing hospitalization;
- •
- A persistent or significant incapacity or substantial disruption of the ability to conduct normal life functions;
- •
- A congenital anomaly/birth defect;
- •
- An important medical event that based on appropriate medical judgement may jeopardize the individual and may require medical or surgical intervention to prevent one of the outcomes listed above.
Instructions for Reporting to VAERS
Vaccination providers should complete and submit a VAERS form to FDA using one of the following methods:
- •
- Complete and submit the report online: https://vaers.hhs.gov/reportevent.html or
- •
- If you are unable to submit this form electronically, you may fax it to VAERS at 1-877-721-0366. If you need additional help submitting a report, you may call the VAERS toll-free information line at 1-800-822-7967 or send an email to info@vaers.org.
IMPORTANT: When reporting adverse events or vaccine administration errors to VAERS, please complete the entire form with detailed information. It is important that the information reported to FDA be as detailed and complete as possible. Information to include:
- •
- Patient demographics (e.g., patient name, date of birth)
- •
- Pertinent medical history
- •
- Pertinent details regarding admission and course of illness
- •
- Concomitant medications
- •
- Timing of adverse event(s) in relationship to administration of Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula)
- •
- Pertinent laboratory and virology information
- •
- Outcome of the event and any additional follow-up information if it is available at the time of the VAERS report. Subsequent reporting of follow-up information should be completed if additional details become available.
The following steps are highlighted to provide the necessary information for safety tracking:
- 1.
- In Box 17, provide information on Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula) and any other vaccines administered on the same day; and in Box 22, provide information on any other vaccines received within one month prior.
- 2.
- In Box 18, description of the event:
- a.
- Write “Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula) EUA” as the first line
- b.
- Provide a detailed report of vaccine administration error and/or adverse event. It is important to provide detailed information regarding the patient and adverse event/medication error for ongoing safety evaluation of this unapproved vaccine. Please see information to include listed above.
- 3.
- Contact information:
- a.
- In Box 13, provide the name and contact information of the prescribing healthcare provider or institutional designee who is responsible for the report.
- b.
- In Box 14, provide the name and contact information of the best doctor/healthcare professional to contact about the adverse event.
- c.
- In Box 15, provide the address of the facility where vaccine was given (NOT the healthcare provider’s office address).
Other Reporting Instructions
Vaccination providers may report to VAERS other adverse events that are not required to be reported using the contact information above.
To the extent feasible, report adverse events to Pfizer Inc. using the contact information below or by providing a copy of the VAERS form to Pfizer Inc.
|
Website |
Fax number |
Telephone number |
|
https://www.pfizersafetyreporting.com |
1-866-635-8337 |
1-800-438-1985 |
- 9
- Vaccination providers administering COMIRNATY (COVID-19 Vaccine, mRNA) (2024-2025 Formula) under EUA must adhere to the same reporting requirements
7. Drug Interactions
There are no data to assess the concomitant administration of Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula) with other vaccines.
8. Use In Specific Populations
8.1 Pregnancy
Risk Summary
All pregnancies have a risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively. Available data on COMIRNATY, Pfizer-BioNTech COVID-19 Vaccine, Bivalent or Pfizer-BioNTech COVID-19 Vaccine administered to pregnant women are insufficient to inform vaccine-associated risks in pregnancy.
A developmental toxicity study has been performed in female rats administered the equivalent of a single human dose of Pfizer-BioNTech COVID-19 Vaccine (Original monovalent) on 4 occasions, twice prior to mating and twice during gestation. These studies revealed no evidence of harm to the fetus due to the vaccine (see Animal Data).
Clinical Considerations
Disease-Associated Maternal and/or Embryo/Fetal Risk
Pregnant individuals infected with SARS-CoV-2 are at increased risk of severe COVID-19 compared with non-pregnant individuals.
Data
In a developmental toxicity study, 0.06 mL of a vaccine formulation containing the same quantity of nucleoside-modified messenger ribonucleic acid (modRNA) (30 mcg) and other ingredients included in a single human dose of Pfizer-BioNTech COVID-19 Vaccine (Original monovalent) was administered to female rats by the intramuscular route on 4 occasions: 21 and 14 days prior to mating, and on gestation days 9 and 20. No vaccine-related adverse effects on female fertility, fetal development, or postnatal development were reported in the study.
8.2 Lactation
Risk Summary
It is not known whether Pfizer-BioNTech COVID-19 Vaccine is excreted in human milk. Data are not available to assess the effects of Pfizer-BioNTech COVID-19 Vaccine on the breastfed infant or on milk production/excretion. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for Pfizer-BioNTech COVID-19 Vaccine and any potential adverse effects on the breastfed child from Pfizer-BioNTech COVID-19 Vaccine or from the underlying maternal condition. For preventive vaccines, the underlying maternal condition is susceptibility to disease prevented by the vaccine.
8.4 Pediatric Use
Pfizer-BioNTech COVID-19 Vaccine is authorized for use in individuals 6 months through 11 years of age.
Pfizer-BioNTech COVID-19 Vaccine is not authorized for use in individuals younger than 6 months of age or individuals 12 years of age and older.
8.6 Use in Immunocompromised Individuals
As reported in an independent publication (Kamar N, Abravanel F, Marion O, et al. Three doses of an mRNA Covid-19 vaccine in solid-organ transplant recipients. N Engl J Med), a single arm study has been conducted in 101 individuals who had undergone various solid organ transplant procedures (heart, kidney, liver, lung, pancreas) 97±8 months previously. A third dose of the Original monovalent Pfizer-BioNTech COVID-19 Vaccine was administered to 99 of these individuals approximately 2 months after they had received a second dose. Following the third dose, the adverse event profile was similar to that after the second dose and no grade 3 or grade 4 events were reported in recipients who were followed for 1 month following post Dose 3. Among the 59 patients who had been seronegative before the third dose, 26 (44%) were seropositive at 4 weeks after the third dose. All 40 patients who had been seropositive before the third dose were still seropositive 4 weeks later. The prevalence of anti-SARS-CoV-2 antibodies was 68% (67 of 99 patients) 4 weeks after the third dose.
Patients should still be counseled to maintain physical precautions to help prevent COVID-19. In addition, close contacts of immunocompromised persons should be vaccinated as appropriate for their health status.
11. Covid-19 Vaccine Pfizer, Bivalent Description
The Pfizer-BioNTech COVID-19 Vaccine does not contain preservative. The vial stoppers are not made with natural rubber latex.
Multiple Dose Vials with Yellow Caps and Labels with Yellow Borders
The Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula) in multiple dose vials with yellow caps and labels with yellow borders is supplied as a frozen suspension; each vial must be diluted with 1.1 mL of sterile 0.9% Sodium Chloride Injection, USP prior to use to form the vaccine.
After dilution, each 0.3 mL dose is formulated to contain 3 mcg of nucleoside-modified messenger RNA (modRNA) encoding the viral spike (S) glycoprotein of SARS-CoV-2 Omicron variant lineage KP.2.
Each 0.3 mL dose also includes the following ingredients: lipids (0.04 mg ((4-hydroxybutyl)azanediyl)bis(hexane-6,1-diyl)bis(2-hexyldecanoate), 0.005 mg 2[(polyethylene glycol)-2000]-N,N-ditetradecylacetamide, 0.01 mg 1,2-distearoyl-sn-glycero-3-phosphocholine, and 0.02 mg cholesterol), 9.4 mg sucrose, 0.02 mg tromethamine, and 0.12 mg tromethamine hydrochloride. The diluent (sterile 0.9% Sodium Chloride Injection, USP) contributes 1.88 mg sodium chloride per dose.
Single Dose Vials with Blue Caps and Labels with Blue Borders
The Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula) in single dose vials with blue caps and labels with blue borders is supplied as a frozen suspension. This presentation does not need to be diluted.
Each 0.3 mL dose is formulated to contain 10 mcg of a modRNA encoding the viral spike (S) glycoprotein of SARS-CoV-2 Omicron variant lineage KP.2.
Each 0.3 mL dose also includes the following ingredients: lipids (0.14 mg ((4-hydroxybutyl)azanediyl)bis(hexane-6,1-diyl)bis(2-hexyldecanoate), 0.02 mg 2[(polyethylene glycol)-2000]-N,N-ditetradecylacetamide, 0.03 mg 1,2-distearoyl-sn-glycero-3-phosphocholine, and 0.06 mg cholesterol), 31 mg sucrose, 0.06 mg tromethamine, and 0.4 mg tromethamine hydrochloride.
12. Covid-19 Vaccine Pfizer, Bivalent - Clinical Pharmacology
The modRNA in the Pfizer-BioNTech COVID-19 Vaccine is formulated in lipid particles, which enable delivery of the RNA into host cells to allow expression of the SARS-CoV-2 S antigen. The vaccine elicits an immune response to the S antigen, which protects against COVID-19.
14 CLINICAL STUDIES
The effectiveness of Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula) for individuals 6 months through 11 years of age is based on:
- •
- effectiveness of the Pfizer-BioNTech COVID-19 Vaccine (Original monovalent) in individuals 6 months of age and older, and
- •
- immunogenicity of Pfizer-BioNTech COVID-19 Vaccine, Bivalent in individuals 6 months through 4 years of age.
14.1 Efficacy of 2-Dose Primary Series of Pfizer-BioNTech COVID-19 Vaccine (Original Monovalent) in Participants 16 Years of Age and Older
Study 2 is a multicenter, multinational, Phase 1/2/3, randomized, placebo-controlled, observer-blind, dose-finding, vaccine candidate-selection, and efficacy study in participants 12 years of age and older. Randomization was stratified by age: 12 through 15 years of age, 16 through 55 years of age, or 56 years of age and older, with a minimum of 40% of participants in the ≥56-year stratum. The study excluded participants who were immunocompromised and those who had previous clinical or microbiological diagnosis of COVID-19. Participants with preexisting stable disease, defined as disease not requiring significant change in therapy or hospitalization for worsening disease during the 6 weeks before enrollment, were included as were participants with known stable infection with human immunodeficiency virus (HIV), hepatitis C virus (HCV), or hepatitis B virus (HBV).
In the Phase 2/3 portion of Study 2, based on data accrued through November 14, 2020, approximately 44,000 participants 12 years of age and older were randomized equally and received 2 doses of Pfizer-BioNTech COVID-19 Vaccine (30 mcg modRNA) or placebo separated by 21 days. Participants are planned to be followed for up to 24 months, for assessments of safety and efficacy against COVID-19.
The population for the analysis of the primary efficacy endpoint included 36,621 participants 12 years of age and older (18,242 in the Pfizer-BioNTech COVID-19 Vaccine group and 18,379 in the placebo group) who did not have evidence of prior infection with SARS-CoV-2 through 7 days after the second dose. Table 14 presents the specific demographic characteristics in the studied population.
|
||
|
Pfizer-BioNTech
|
Placebo
|
|
|
Sex | ||
|
Male |
9318 (51.1) |
9225 (50.2) |
|
Female |
8924 (48.9) |
9154 (49.8) |
|
Age (years) | ||
|
Mean (SD) |
50.6 (15.70) |
50.4 (15.81) |
|
Median |
52.0 |
52.0 |
|
Min, max |
(12, 89) |
(12, 91) |
|
Age group | ||
|
≥12 through 15 years‡ |
46 (0.3) |
42 (0.2) |
|
≥16 through 17 years |
66 (0.4) |
68 (0.4) |
|
≥16 through 64 years |
14,216 (77.9) |
14,299 (77.8) |
|
≥65 through 74 years |
3176 (17.4) |
3226 (17.6) |
|
≥75 years |
804 (4.4) |
812 (4.4) |
|
Race | ||
|
White |
15,110 (82.8) |
15,301 (83.3) |
|
Black or African American |
1617 (8.9) |
1617 (8.8) |
|
American Indian or Alaska Native |
118 (0.6) |
106 (0.6) |
|
Asian |
815 (4.5) |
810 (4.4) |
|
Native Hawaiian or other Pacific Islander |
48 (0.3) |
29 (0.2) |
|
Other§ |
534 (2.9) |
516 (2.8) |
|
Ethnicity | ||
|
Hispanic or Latino |
4886 (26.8) |
4857 (26.4) |
|
Not Hispanic or Latino |
13,253 (72.7) |
13,412 (73.0) |
|
Not reported |
103 (0.6) |
110 (0.6) |
|
Comorbidities¶ | ||
|
Yes |
8432 (46.2) |
8450 (46.0) |
|
No |
9810 (53.8) |
9929 (54.0) |
The population in the primary efficacy analysis included all participants 12 years of age and older who had been enrolled from July 27, 2020, and followed for the development of COVID-19 through November 14, 2020. Participants 18 through 55 years of age and 56 years of age and older began enrollment from July 27, 2020, 16 through 17 years of age began enrollment from September 16, 2020, and 12 through 15 years of age began enrollment from October 15, 2020.
The vaccine efficacy information is presented in Table 15.
| Note: Confirmed cases were determined by Reverse Transcription-Polymerase Chain Reaction (RT-PCR) and at least 1 symptom consistent with COVID-19 (symptoms included: fever; new or increased cough; new or increased shortness of breath; chills; new or increased muscle pain; new loss of taste or smell; sore throat; diarrhea; vomiting). | |||
|
|||
|
First COVID-19 occurrence from 7 days after Dose 2 in participants without evidence of prior SARS-CoV-2 infection* |
|||
|
Subgroup |
Pfizer-BioNTech COVID-19 Vaccine†
|
Vaccine Efficacy %
|
|
|
All subjectsÞ |
8 |
162 |
95.0 |
|
16 through 64 years |
7 |
143 |
95.1 |
|
65 years and older |
1 |
19 |
94.7 |
|
First COVID-19 occurrence from 7 days after Dose 2 in participants with or without evidence of prior SARS-CoV-2 infection |
|||
|
Subgroup |
Pfizer-BioNTech COVID-19 Vaccine†
|
Vaccine Efficacy %
|
|
|
All subjectsÞ |
9 |
169 |
94.6 |
|
16 through 64 years |
8 |
150 |
94.6 |
|
65 years and older |
1 |
19 |
94.7 |
14.2 Efficacy of 2-Dose Primary Series of Pfizer-BioNTech COVID-19 Vaccine (Original Monovalent) in Participants 12 Through 15 Years of Age
A descriptive efficacy analysis of Study 2 has been performed in approximately 2,200 participants 12 through 15 years of age evaluating confirmed COVID-19 cases accrued up to a data cutoff date of March 13, 2021.
The efficacy information in participants 12 through 15 years of age is presented in Table 16.
| Note: Confirmed cases were determined by Reverse Transcription-Polymerase Chain Reaction (RT-PCR) and at least 1 symptom consistent with COVID-19 (symptoms included: fever; new or increased cough; new or increased shortness of breath; chills; new or increased muscle pain; new loss of taste or smell; sore throat; diarrhea; vomiting). | |||
|
|||
|
First COVID-19 occurrence from 7 days after Dose 2 in participants 12 through 15 years of age without evidence of prior SARS-CoV-2 infection* |
|||
|
Pfizer-BioNTech COVID-19 Vaccine†
|
Vaccine Efficacy %
|
||
|
Participants 12 through 15 years of age |
0 |
16 |
100.0 |
|
First COVID-19 occurrence from 7 days after Dose 2 in participants 12 through 15 years of age with or without evidence of prior SARS-CoV-2 infection |
|||
|
Pfizer-BioNTech COVID-19 Vaccine†
|
Vaccine Efficacy %
|
||
|
Participants 12 through 15 years of age |
0 |
18 |
100.0 |
14.3 Efficacy of 2-Dose Primary Series of Pfizer-BioNTech COVID-19 Vaccine (Original Monovalent) in Participants 5 Through 11 Years of Age
A descriptive efficacy analysis of Study 3 has been performed in 1,968 participants 5 through 11 years of age without evidence of infection prior to 7 days after Dose 2. This analysis evaluated confirmed symptomatic COVID-19 cases accrued up to a data cutoff date of October 8, 2021.
Table 17 presents the specific demographic characteristics in participants who did not have evidence of prior infection with SARS-CoV-2 through 7 days after the second dose.
| Pfizer-BioNTech COVID-19 Vaccine*
10 mcg/Dose (N†=1305) n‡ (%) | Placebo
(N†=663) n‡ (%) |
|
|---|---|---|
|
||
|
Sex |
||
|
Male |
679 (52.0) |
343 (51.7) |
|
Female |
626 (48.0) |
320 (48.3) |
|
Age at Vaccination |
||
|
Mean (SD) |
8.2 (1.93) |
8.1 (1.98) |
|
Median |
8.0 |
8.0 |
|
Min, max |
(5, 11) |
(5, 11) |
|
Race |
||
|
White |
1018 (78.0) |
514 (77.5) |
|
Black or African American |
76 (5.8) |
48 (7.2) |
|
American Indian or Alaska Native |
<1.0% |
<1.0% |
|
Asian |
86 (6.6) |
46 (6.9) |
|
Native Hawaiian or other Pacific Islander |
<1.0% |
<1.0% |
|
Other§ |
110 (8.4) |
52 (7.8) |
|
Ethnicity |
||
|
Hispanic or Latino |
243 (18.6) |
130 (19.6) |
|
Not Hispanic or Latino |
1059 (81.1) |
533 (80.4) |
|
Not reported |
<1.0% |
<1.0% |
|
Comorbidities¶ |
||
|
Yes |
262 (20.1) |
133 (20.1) |
|
No |
1043 (79.9) |
530 (79.9) |
The descriptive vaccine efficacy results in participants 5 through 11 years of age without evidence of prior SARS-CoV-2 infection are presented in Table 18. None of the cases accrued met criteria for severe COVID-19 or multisystem inflammatory syndrome in children (MIS-C). No cases of COVID-19 were observed in either the vaccine group or the placebo group in participants with evidence of prior SARS-CoV-2 infection.
| First COVID-19 occurrence from 7 days after Dose 2 in participants 5 through 11 years of age without evidence of prior SARS-CoV-2 infection* | |||
|---|---|---|---|
| Pfizer-BioNTech COVID-19 Vaccine†
10 mcg/dose N‡=1305 Cases n1§ Surveillance Time¶ (n2#) | Placebo
N‡=663 Cases n1§ Surveillance Time¶ (n2#) | Vaccine Efficacy %
(95% CI) |
|
| Note: Confirmed cases were determined by Reverse Transcription-Polymerase Chain Reaction (RT-PCR) and at least 1 symptom consistent with COVID-19 (symptoms included: fever; new or increased cough; new or increased shortness of breath; chills; new or increased muscle pain; new loss of taste or smell; sore throat; diarrhea; vomiting). | |||
|
|||
|
Participants 5 through 11 years of age |
3 |
16 |
90.7 |
14.4 Immunogenicity of 2-Dose Primary Series of Pfizer-BioNTech COVID-19 Vaccine (Original Monovalent) in Participants 5 Through 11 Years of Age
SARS-CoV-2 50% neutralizing antibody titers (NT50) 1 month after the primary series were compared between randomly selected subsets of Phase 2/3 participants 5 through 11 years of age from study C4591007 and the efficacy study C4591001 Phase 2/3 participants 16 through 25 years of age, using a microneutralization assay against the reference strain (USA_WA1/2020). The primary immunobridging analyses compared the geometric mean titers (using a geometric mean ratio [GMR]) and the seroresponse (defined as achieving at least 4-fold rise in SARS-CoV-2 NT50 from before Dose 1) rates in the evaluable immunogenicity population of participants without evidence of prior SARS-CoV-2 infection up to 1 month after Dose 2 in each group. The prespecified immunobridging criteria were met for both the GMR and the seroresponse difference (Table 19 and Table 20).
| Abbreviations: CI = confidence interval; GMR = geometric mean ratio; GMT = geometric mean titer; LLOQ = lower limit of quantitation; NAAT = nucleic acid amplification test; NT50 = 50% neutralizing titer; SARS-CoV-2 = severe acute respiratory syndrome coronavirus 2. Note: Participants who had no serological or virological evidence (up to 1 month post-Dose 2 blood sample collection) of past SARS-CoV-2 infection (i.e., N-binding antibody [serum] negative at pre-Dose 1 and 1 month after Dose 2, SARS-CoV-2 not detected by NAAT [nasal swab] at pre-Dose 1 and pre-Dose 2, and negative NAAT (nasal swab) at any unscheduled visit up to 1 month after Dose 2 blood collection) and had no medical history of COVID-19 were included in the analysis. |
||||
|
||||
|
Pfizer-BioNTech COVID-19 Vaccine |
GMT Ratio (95%CI)
|
|||
|
Assay |
Time Point# | |||
|
SARS-CoV-2 neutralization assay – NT50 (titer)ß |
1 month after Dose 2 |
1197.6 |
1146.5 |
1.04 |
| Abbreviations: LLOQ = lower limit of quantitation; NAAT = nucleic acid amplification test; N-binding = SARS-CoV-2 nucleoprotein–binding; NT50 = 50% neutralizing titer 50; SARS-CoV-2 = severe acute respiratory syndrome coronavirus 2. Note: Seroresponse is defined as achieving a ≥4-fold rise from baseline (before Dose 1). If the baseline measurement is below the LLOQ, a post-vaccination assay result ≥4 × LLOQ is considered a seroresponse Note: Participants who had no serological or virological evidence (up to 1 month post-Dose 2 blood sample collection) of past SARS-CoV-2 infection (i.e., N-binding antibody [serum] negative at pre-Dose 1 and 1 month after Dose 2, SARS-CoV-2 not detected by NAAT [nasal swab] at pre-Dose 1 and pre-Dose 2, and negative NAAT (nasal swab) at any unscheduled visit up to 1 month after Dose 2 blood collection) and had no medical history of COVID-19 were included in the analysis. |
||||
|
||||
|
Pfizer-BioNTech COVID-19 Vaccine |
Difference in Seroresponse Rates %* (95% CI†)
|
|||
|
Assay |
Time PointÞ | |||
|
SARS-CoV-2 neutralization assay – NT50 (titer)è |
1 month after Dose 2 |
262 (99.2) |
251 (99.2) |
0.0 |
14.5 Effectiveness of 3-Dose Primary Series of Pfizer-BioNTech COVID-19 Vaccine (Original Monovalent) in Participants 6 Months Through 4 Years of Age
Study 3 is an ongoing Phase 1/2/3 multicenter, randomized, dose finding, open-label (Phase 1) and multinational, saline placebo-controlled, observer-blind, immunogenicity and efficacy (Phase 2/3) study to evaluate the safety and effectiveness of Pfizer-BioNTech COVID-19 Vaccine in individuals 6 months through 11 years of age. Randomization was stratified by age: 6 through 23 months of age, 2 through 4 years of age, or 5 through 11 years of age. The study excluded participants who were immunocompromised and those who had previous clinical or microbiological diagnosis of COVID-19. Results from participants 6 months through 4 years of age are presented in this subsection. In Phase 2/3, a total of 1,776 participants 6 through 23 months of age and 2,750 participants 2 through 4 years of age were randomized 2:1 and received 3 doses of the Pfizer-BioNTech COVID-19 Vaccine or saline placebo.
Effectiveness in individuals 6 months through 4 years of age is based on a comparison of immune responses in this age group to individuals 16 through 25 years of age.
Immunogenicity in Participants 2 Through 4 Years of Age After a 3-Dose Primary Series
Immunogenicity analyses have been performed in the immunobridging subset of 143 Study 3 participants 2 through 4 years of age without evidence of infection up to 1 month after Dose 3 based on a data cutoff date of April 29, 2022.
The evaluable immunogenicity population without prior evidence of SARS-CoV-2 infection up to 1 month after Dose 3 of Pfizer-BioNTech COVID-19 Vaccine was comprised of 143 participants 2 through 4 years of age. Most participants in this analysis population were White 69.2%, with 5.6% Black or African American participants, 11.2% Asian participants, and 11.9% multi-racial participants. There were 11.2% Hispanic/Latino participants. The median age was 3.0 years and 44.1% of participants were male. There were 6.3% of participants reported as obese. In the evaluable immunogenicity population (regardless of evidence of prior infection), 11/204 participants (5.4%) were baseline positive for prior SARS-CoV-2 infection.
SARS-CoV-2 NT50 were compared between an immunogenicity subset of Phase 2/3 participants 2 through 4 years of age from Study 3 at 1 month after the 3-dose primary series and a randomly selected subset from Study 2 Phase 2/3 participants 16 through 25 years of age at 1 month after the 2-dose primary series, using a microneutralization assay against the reference strain (USA_WA1/2020). The primary immunobridging analyses compared the geometric mean titers (using a GMR) and the seroresponse (defined as achieving at least 4-fold rise in SARS-CoV-2 NT50 from before Dose 1) rates in the evaluable immunogenicity population of participants without evidence of prior SARS-CoV-2 infection up to 1 month after Dose 3 in participants 2 through 4 years of age and up to 1 month after Dose 2 in participants 16 through 25 years of age. The prespecified immunobridging criteria were met for both the GMR and the seroresponse difference (Table 21 and Table 22, respectively).
| Abbreviations: CI = confidence interval; GMR = geometric mean ratio; GMT = geometric mean titer; LLOQ = lower limit of quantitation; NAAT = nucleic acid amplification test; NT50 = 50% neutralizing titer; SARS-CoV-2 = severe acute respiratory syndrome coronavirus 2. Note: Participants who had no serological or virological evidence [(up to 1 month after Dose 2 (Study 2) or 1 month after Dose 3 (Study 3) blood sample collection)] of past SARS-CoV-2 infection [(i.e., N-binding antibody [serum] negative at Dose 1, Dose 3 (Study 3) and 1 month after Dose 2 (Study 2) or 1 month after Dose 3 (Study 3), SARS-CoV-2 not detected by NAAT [nasal swab] at Dose 1, Dose 2, and Dose 3 (Study 3) study visits, and negative NAAT (nasal swab) at any unscheduled visit up to 1 month after Dose 2 (Study 2) or 1 month after Dose 3 (Study 3) blood collection)] and had no medical history of COVID-19 were included in the analysis. |
|||
|
|||
|
Assay |
Pfizer-BioNTech COVID-19 Vaccine |
GMR (95%CI) |
|
|
3 mcg modRNA/Dose
|
30 mcg modRNA/Dose
|
||
|
SARS-CoV-2 neutralization assay – NT50 (titer)¶ |
1535.2 |
1180.0 |
1.30 |
| Abbreviations: LLOQ = lower limit of quantitation; NAAT = nucleic acid amplification test; N-binding = SARS-CoV-2 nucleoprotein–binding; NT50 = 50% neutralizing titer 50; SARS-CoV-2 = severe acute respiratory syndrome coronavirus 2. Note: Seroresponse is defined as achieving a ≥4-fold rise from baseline (before Dose 1). If the baseline measurement is below the LLOQ, a post-vaccination assay result ≥4 × LLOQ is considered a seroresponse. Note: Participants who had no serological or virological evidence (up to 1 month after Dose 2 [(Study 2) or 1 month after Dose 3 (Study 3) blood sample collection)[ of past SARS-CoV-2 infection [(i.e., N-binding antibody [serum] negative at pre-Dose 1, pre-Dose 3 (Study 3) and 1 month after Dose 2 (Study 2) or 1 month after Dose 3 (Study 3), SARS-CoV-2 not detected by NAAT [nasal swab] at pre-Dose 1, pre-Dose 2, and pre-Dose 3 (Study 3) study visits, and negative NAAT (nasal swab) at any unscheduled visit up to 1 month after Dose 2 (Study 2) or 1 month after Dose 3 (Study 3) blood collection)] and had no medical history of COVID-19 were included in the analysis. |
|||
|
|||
|
Pfizer-BioNTech COVID-19 Vaccine |
Difference in Seroresponse Rates %*
|
||
|
3 mcg modRNA/Dose
|
30 mcg modRNA/Dose
|
||
|
Assay | |||
|
SARS-CoV-2 neutralization assay – NT50 (titer)Þ |
141 (100.0) |
168 (98.8) |
1.2 |
Using a non-validated fluorescence focus reduction neutralization test assay against the Omicron variant of SARS-CoV-2 (BA.1), the NT50 GMT at 1 month after Dose 3 among a subset of 34 study participants without evidence of prior SARS-CoV-2 infection (82.5 [95% CI: 55.4, 122.9]) was increased compared to the NT50 GMT before Dose 3 (14.0 [95% CI: 10.6, 18.5]).
Immunogenicity in Participants 6 Through 23 Months of Age After a 3-Dose Primary Series
Immunogenicity analyses have been performed in the immunobridging subset of 82 Study 3 participants 6 through 23 months of age without evidence of infection up to 1 month after Dose 3 based on a data cutoff date of April 29, 2022.
The evaluable immunogenicity population without prior evidence of SARS-CoV-2 infection up to 1 month after Dose 3 of Pfizer-BioNTech COVID-19 Vaccine was comprised of 82 participants 6 through 23 months of age. Most participants in this analysis population were White (72.0%), with 1.2% Black or African American participants, 13.4% Asian participants, and 12.2% multi-racial participants. There were 15.9% Hispanic/Latino participants. The median age was 16.0 months and 62.2% of participants were male. In the evaluable immunogenicity population (regardless of evidence of prior infection), 6/132 participants (4.5%) were baseline positive for prior SARS-CoV-2 infection.
SARS-CoV-2 NT50 1 month after the vaccination series were compared between an immunogenicity subset of Phase 2/3 participants 6 through 23 months of age from Study 3 and a randomly selected subset from Study 2 Phase 2/3 participants 16 through 25 years of age, using a microneutralization assay against the reference strain (USA_WA1/2020). The primary immunobridging analyses compared the geometric mean titers (using a GMR) and the seroresponse (defined as achieving at least 4-fold rise in SARS-CoV-2 NT50 from before Dose 1) rates in the evaluable immunogenicity population of participants without evidence of prior SARS-CoV-2 infection up to 1 month after Dose 3 in participants 6 through 23 months of age and up to 1 month after Dose 2 in participants 16 through 25 years of age. The prespecified immunobridging criteria were met for both the GMR and the seroresponse difference (Table 23 and Table 24, respectively).
| Abbreviations: CI = confidence interval; GMR = geometric mean ratio; GMT = geometric mean titer; LLOQ = lower limit of quantitation; NAAT = nucleic acid amplification test; NT50 = 50% neutralizing titer; SARS-CoV-2 = severe acute respiratory syndrome coronavirus 2. Note: Participants who had no serological or virological evidence [(up to 1 month after Dose 2 (Study 2) or 1 month after Dose 3 (Study 3) blood sample collection)] of past SARS-CoV-2 infection (i.e., N-binding antibody [serum] negative at Dose 1, Dose 3 (Study 3) and 1 month after Dose 2 (Study 2) or 1 month after Dose 3 (Study 3), SARS-CoV-2 not detected by NAAT [nasal swab] at Dose 1, Dose 2, and Dose 3 (Study 3) study visits, and negative NAAT (nasal swab) at any unscheduled visit up to 1 month after Dose 2 (Study 2) or 1 month after Dose 3 (Study 3) blood collection)] and had no medical history of COVID-19 were included in the analysis. |
|||
|
|||
|
Pfizer-BioNTech COVID-19 Vaccine |
GMR (95%CI)
|
||
|
3 mcg modRNA/Dose
|
30 mcg modRNA/Dose
|
||
|
Assay | |||
|
SARS-CoV-2 neutralization assay – NT50 (titer)¶ |
1406.5 |
1180.0 |
1.19 |
| Abbreviations: LLOQ = lower limit of quantitation; NAAT = nucleic acid amplification test; N-binding = SARS-CoV-2 nucleoprotein–binding; NT50 = 50% neutralizing titer 50; SARS-CoV-2 = severe acute respiratory syndrome coronavirus 2. Note: Seroresponse is defined as achieving a ≥4-fold rise from baseline (before Dose 1). If the baseline measurement is below the LLOQ, a post-vaccination assay result ≥4 × LLOQ is considered a seroresponse. Note: Participants who had no serological or virological evidence [(up to 1 month after Dose 2 (Study 2) or 1 month after Dose 3 (Study 3) blood sample collection) of past SARS-CoV-2 infection (i.e., N-binding antibody [serum] negative at pre-Dose 1, Dose 3 (Study 3) and 1 month after Dose 2 (Study 2) or 1 month after Dose 3 (Study 3), SARS-CoV-2 not detected by NAAT [nasal swab] at pre-Dose 1, pre-Dose 2, and pre-Dose 3 (Study 3) study visits, and negative NAAT (nasal swab) at any unscheduled visit up to 1 month after Dose 2 (Study 2) or 1 month after Dose 3 (Study 3) blood collection)] and had no medical history of COVID-19 were included in the analysis. |
|||
|
|||
|
Pfizer-BioNTech COVID-19 Vaccine |
Difference in Seroresponse Rates %*
|
||
|
3 mcg modRNA/Dose 6 Through 23 months of Age
|
30 mcg modRNA/Dose
|
||
|
Assay | |||
|
SARS-CoV-2 neutralization assay – NT50 (titer)Þ |
80 (100.0) |
168 (98.8) |
1.2 |
Using a non-validated fluorescence focus reduction neutralization test assay against the Omicron variant of SARS-CoV-2 (BA.1), the NT50 GMT at 1 month after Dose 3 among a subset of 32 study participants without evidence of prior SARS-CoV-2 infection (127.5 [95% CI: 90.2, 180.1]) was increased compared to the NT50 GMT before Dose 3 (16.3 [95% CI: 12.8, 20.8]).
Efficacy in Participants 6 Months Through 4 Years of Age After a 3-Dose Primary Series
A descriptive efficacy analysis of Study 3 was performed across the combined population of participants 6 months through 4 years of age based on PCR-confirmed COVID-19 cases among 873 participants in the Pfizer-BioNTech COVID-19 Vaccine group and 381 participants in the placebo group (2:1 randomization) who received 3 doses of study intervention during the blinded follow-up period when the Omicron variant of SARS-CoV-2 (BA.2) was the predominant variant in circulation (data cutoff date of June 17, 2022).
The evaluable efficacy population without prior evidence of SARS-CoV-2 infection up to 7 days after Dose 3 of Pfizer-BioNTech COVID-19 Vaccine was comprised of 873 vaccine recipients and 381 placebo recipients 6 months through 4 years of age. Most vaccine recipients in this analysis population were White (76.3%), with 3.4% Black or African American participants, 10.0% Asian participants, and 10.1% who identified as multi-racial, other or not reported. There were 11.2% Hispanic/Latino vaccine recipients. Among the vaccine recipients, 51.1% were female. The median age was 16.0 months in vaccine recipients 6 through 23 months of age and the median age was 3.0 years in vaccine recipients 2 through 4 years of age. In the evaluable efficacy population, 8.7% of vaccine recipients had one or more comorbidities that increase the risk of severe COVID-19 as described in the Morbidity and Mortality Weekly Report (MMWR) 69(32);1081-8 and/or obesity (BMI ≥95th percentile) for participants 2 through 4 years of age. Between participants who received Pfizer-BioNTech COVID-19 Vaccine and those who received placebo, there were no notable differences in demographics.
The median dose interval between Dose 2 and Dose 3 was 13.4 weeks (range 8 to 33 weeks) among participants 6 through 23 months of age and 10 weeks (range 8 to 34 weeks) among participants 2 through 4 years of age who received Pfizer-BioNTech COVID-19 Vaccine. The median length of blinded follow-up for efficacy after Dose 3 was 1.7 months for participants 6 through 23 months of age and 2.1 months for participants 2 through 4 years of age in the Dose 3 Evaluable Efficacy Population who received Pfizer-BioNTech COVID-19 Vaccine or placebo.
The vaccine efficacy results after Dose 3 in participants 6 months through 4 years of age are presented in Table 25.
| Abbreviations: NAAT = nucleic acid amplification test; N-binding = SARS-CoV-2 nucleoprotein–binding; SARS-CoV-2 = severe acute respiratory syndrome coronavirus 2; VE = vaccine efficacy. Note: Confirmed cases were determined by Reverse Transcription-Polymerase Chain Reaction (RT-PCR) and at least 1 symptom consistent with COVID-19 (symptoms included: fever; new or increased cough; new or increased shortness of breath; chills; new or increased muscle pain; new loss of taste or smell; sore throat; diarrhea; vomiting; inability to eat/poor feeding). |
|||
|
|||
|
First COVID-19 occurrence from 7 days after Dose 3 in participants without evidence of prior SARS-CoV-2 infection* |
|||
|
Subgroup |
Pfizer-BioNTech COVID-19 Vaccine
|
Vaccine Efficacy %
|
|
|
6 months through 4 years# |
13 |
21 |
73.2 |
|
2 through 4 years |
9 |
13 |
71.8 |
|
6 through 23 months |
4 |
8 |
75.8 |
|
First COVID-19 occurrence from 7 days after Dose 3 in participants with or without evidence of prior SARS-CoV-2 infection |
|||
|
Subgroup |
Pfizer-BioNTech COVID-19 Vaccine
|
Vaccine Efficacy %
|
|
|
6 months through 4 years# |
14 |
23 |
72.5 |
|
2 through 4 years |
10 |
15 |
70.7 |
|
6 through 23 months |
4 |
8 |
76.2 |
Among participants 6 months through 4 years of age, severe COVID-19 case criteria were fulfilled after Dose 3 in 1 placebo recipient in the 6 through 23-month age group. This case occurred 44 days after Dose 3, based on a single criterion (increased heart rate) and did not require hospitalization. There were no cases of multisystem inflammatory syndrome in children reported through the June 17, 2022 data cutoff date.
14.6 Immunogenicity of Pfizer-BioNTech COVID-19 Vaccine (Original Monovalent) Booster Dose Following Pfizer-BioNTech COVID-19 Vaccine (Original Monovalent) Primary Series in Participants 5 Through 11 Years of Age
In Study 3, immunogenicity of a booster dose administered at 7 to 9 months after the second primary series dose was evaluated in 67 study participants 5 through 11 years of age who had no serological or virological evidence of past SARS-CoV-2 infection up to 1 month after the booster dose. Using a microneutralization assay against the reference strain of SARS-CoV-2 (USA_WA1/2020), the NT50 GMT at 1 month after the booster dose (2720.9 [95% CI: 2280.1, 3247.0]) was increased compared to before the booster dose (271.0 [95% CI: 229.1, 320.6]). Using a non-validated fluorescence focus reduction neutralization test assay against the Omicron variant of SARS-CoV-2 (B.1.1.529), the NT50 GMT at 1 month after the booster dose among a subset of 17 study participants (614.4 [95% CI: 410.7, 919.2]) was increased compared to the NT50 GMT at 1 month after dose 2 among a subset of 29 study participants (27.6 [95% CI: 22.1, 34.5]).
14.7 Immunogenicity of a Pfizer-BioNTech COVID-19 Vaccine (Original Monovalent) Booster Dose Following Primary Vaccination with Another Authorized or Approved COVID-19 Vaccine (Original Monovalent)
Effectiveness of a Pfizer-BioNTech COVID-19 Vaccine booster dose (30 mcg modRNA) in individuals who completed primary vaccination with another authorized or approved COVID-19 Vaccine (heterologous booster dose) is inferred from immunogenicity data supporting effectiveness of a Pfizer-BioNTech COVID-19 Vaccine booster dose administered following completion of Pfizer-BioNTech COVID-19 Vaccine primary series and from immunogenicity data from an independent NIH study Phase 1/2 open-label clinical trial (NCT04889209) conducted in the United States that evaluated a heterologous booster dose of the Pfizer-BioNTech COVID-19 Vaccine. In this study, participants who had completed primary vaccination with a Moderna COVID-19 Vaccine 2-dose series (N=151), a Janssen COVID-19 Vaccine single dose (N=156), or a Pfizer-BioNTech COVID-19 Vaccine 2-dose series (N=151) at least 12 weeks prior to enrollment and who reported no history of SARS-CoV-2 infection were randomized 1:1:1 to receive a booster dose of 1 of 3 vaccines: Moderna COVID-19 Vaccine, Janssen COVID-19 Vaccine, or Pfizer-BioNTech COVID-19 Vaccine (30 mcg modRNA). Neutralizing antibody titers, as measured by a pseudovirus neutralization assay using a lentivirus expressing the SARS-CoV-2 Spike protein with D614G mutation, were assessed on Day 1 prior to administration of the booster dose and on Day 15 after the booster dose. A booster response to the Pfizer-BioNTech COVID-19 Vaccine was demonstrated regardless of the vaccine used for primary vaccination.
14.8 Immunogenicity of Pfizer-BioNTech COVID-19 Vaccine, Bivalent (Original and Omicron BA.4/BA.5) Administered as a Booster (Fourth Dose) in Individuals 6 Months Through 4 Years of Age
In Study 6, a subset of 60 participants 6 months through 4 years of age received a booster dose (fourth dose) of Pfizer-BioNTech COVID-19 Vaccine, Bivalent (3 mcg modRNA) after receiving 3 prior doses of Pfizer-BioNTech COVID-19 Vaccine (Original monovalent, 3 mcg modRNA). Neutralizing antibody levels following the fourth dose are presented in Table 26. Data from a subset of participants 6 months through 4 years of age in Study 3 who received 3 doses of Pfizer-BioNTech COVID-19 Vaccine (Original monovalent, 3 mcg modRNA) are included as a reference. There were no formal statistical comparisons of the immune response between subsets from the two studies.
| Abbreviations: GMT = geometric mean titer; LLOQ = lower limit of quantitation; N-binding = SARS-CoV-2 nucleoprotein-binding; NAAT = nucleic acid amplification test. NT50 = 50% neutralizing titer; SARS-CoV-2 = severe acute respiratory syndrome coronavirus 2. |
||||||
|
||||||
|
SARS-CoV-2 Neutralization Assay |
Age Group |
Sampling Time Point† |
Study 6 Pfizer-BioNTech COVID-19 Vaccine, Bivalent (Original/Omicron BA.4/BA.5) 3 mcg modRNA Dose 4 and 1 Month After Dose 4 |
Study 3 Pfizer-BioNTech COVID‑19 Vaccine (Original Monovalent) 3 mcg modRNA Dose 3 and 1 Month After Dose 3 |
||
|
n‡ |
n‡ | |||||
|
Omicron BA.4/BA.5 – NT50 (titer)¶ |
6 through 23 months |
Pre- vaccination |
21 |
243.9 (115.3, 516.1) |
23 |
96.0 (55.3, 166.8) |
|
1 month |
23 |
2011.4 (1141.3, 3544.9) |
23 |
625.6 (365.7, 1070.5) |
||
|
2 through 4 years |
Pre- vaccination |
33 |
165.6 (88.3, 310.5) |
31 |
56.1 (38.0, 82.7) |
|
|
1 month |
35 |
1514.9 (882.2, 2601.5) |
31 |
595.0 (370.5, 955.6) |
||
|
Reference strain – NT50 (titer)¶ |
6 through 23 months |
Pre-vaccination |
22 |
2491.2 (1432.0, 4333.8) |
22 |
981.6 (503.5, 1913.7) |
|
1 month |
23 |
8737.2 (5959.6, 12809.5) |
23 |
9221.7 (6734.0, 12628.3) |
||
|
2 through |
Pre-vaccination |
35 |
2802.7 (1795.7, 4374.3) |
31 |
657.9 (421.5, 1026.9) |
|
|
1 month |
35 |
10448.3 (7685.1, 14205.1) |
30 |
8933.3 (6388.0, 12492.9) |
||
14.9 Effectiveness of a Single Dose of Pfizer-BioNTech COVID-19 Vaccine (Original Monovalent) in Individuals with Evidence of Prior SARS-CoV-2 Infection
Seroprevalence surveys estimate that almost all of the U.S. population 5 years of age and older now have antibodies (from vaccination and/or infection) against SARS-CoV-2 (Centers for Disease Control and Prevention. COVID Data Tracker. Atlanta, GA: US Department of Health and Human Services, CDC; 2023, March 31. https://covid.cdc.gov/covid-data-tracker#datatracker-home).
Powell et al. conducted an observational test-negative study including symptomatic individuals aged 12 to 17 years of age with SARS-CoV-2 polymerase chain reaction (PCR) testing results in England from August 9, 2021 to March 31, 2022 (Powell et al. Protection against symptomatic infection with delta (B.1.617.2) and omicron (B.1.1.529) BA.1 and BA.2 SARS-CoV-2 variants after previous infection and vaccination in adolescents in England, August, 2021–March, 2022: a national, observational, test-negative, case-control study. Lancet Infectious Diseases. April 2023). Among 1,161,704 SARS-CoV-2 PCR tests linked to COVID-19 vaccination status, there were 390,467 SARS-CoV-2 PCR-confirmed positive tests during Delta variant predominance and 212,433 SARS-CoV-2 positive tests during Omicron variants BA.1 and BA.2 predominance. Among adolescents who had received only 1 dose of the Pfizer-BioNTech COVID-19 Vaccine, those who had evidence of previous infection with Alpha, Delta, or Omicron variants had increased protection against symptomatic Omicron infection compared with those with no evidence of previous infection. At 2 to 14 weeks following 1 dose of the Pfizer-BioNTech COVID-19 Vaccine, the estimated effectiveness was 18.8% (95% CI: 17.2%, 20.3%), 81.5% (95% CI: 80.0%, 82.9%), 78.8% (95% CI: 77.9, 79.5%), and 79.6% (95% CI: 44.9%, 92.4%) for individuals with no evidence of prior infection, and evidence of prior Alpha, Delta, and Omicron infection, respectively.
16. How is Covid-19 Vaccine Pfizer, Bivalent supplied
How Supplied
Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula): multiple dose vials with yellow caps and labels with yellow borders
|
NDC 59267-4426-2 |
Carton of 10 multiple dose vials |
|
NDC 59267-4426-1 |
Multiple dose vial containing 3 doses of 0.3 mL (after dilution) |
Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula): single dose vials with blue caps and labels with blue borders
|
NDC 59267-4438-2 |
Carton of 10 single dose vials |
|
NDC 59267-4438-1 |
One vial contains 1 dose of 0.3 mL (Do Not Dilute) |
During storage, minimize exposure to room light, and avoid exposure to direct sunlight and ultraviolet light. Do not refreeze thawed vials.
Vial Storage Prior to Use
Cartons of Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula) may arrive frozen at ultra-cold conditions in thermal containers with dry ice.
Once received, frozen vials may be immediately transferred to the refrigerator [2ºC to 8ºC (35ºF to 46ºF)], thawed and stored for up to 10 weeks, not to exceed the expiration date printed on the vial and cartons. The 10-week refrigerated expiry date should be recorded on the carton at the time of transfer. Cartons of multiple dose vials with yellow caps and labels with yellow borders and cartons of single dose vials with blue caps and labels with blue borders may take up to 2 hours to thaw at this temperature.
Alternatively, frozen vials may be stored in an ultra-low temperature freezer at -90ºC to -60ºC (-130ºF to -76ºF) until the expiration date printed on the vials and cartons. Do not store vials at -25°C to -15°C (-13°F to 5°F). Once vials are thawed, they should not be refrozen.
If cartons of Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula) are received at 2°C to 8°C (35ºF to 46ºF), they should be stored at 2°C to 8°C (35ºF to 46ºF). Check that the carton has been updated to reflect the 10-week refrigerated expiry date, not to exceed the expiration date printed on the vial and cartons.
Vial Storage During Use
If not previously thawed at 2ºC to 8ºC (35ºF to 46ºF), allow Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula) multiple dose vials or single dose vials to thaw at room temperature [up to 25ºC (77ºF)] for 30 minutes.
Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula) may be stored at room temperature [8°C to 25°C (46°F to 77°F)] for a total of 12 hours prior to the first puncture. After dilution, multiple dose vials should be held between 2ºC to 25°C (35°F to 77°F). Multiple dose vials should be discarded 12 hours after dilution.
Transportation of Vials
If local redistribution is needed, multiple dose vials and single dose vials may be transported at -90°C to -60°C (-130°F to -76°F) or 2°C to 8°C (35°F to 46°F).
17 PATIENT COUNSELING INFORMATION
Advise the recipient or caregiver to read the Fact Sheet for Recipients and Caregivers.
The vaccination provider must include vaccination information in the state/local jurisdiction's Immunization Information System (IIS) or other designated system. Advise recipient or caregiver that more information about IISs can be found at: https://www.cdc.gov/vaccines/programs/iis/about.html
18 MANUFACTURER INFORMATION
For general questions, visit the website or call the telephone number provided below.
This Full EUA Fact Sheet may have been updated. For the most recent Full EUA Fact Sheet, please see https://www.cvdvaccine.com.

Manufactured for
BioNTech Manufacturing GmbH
An der Goldgrube 12
55131 Mainz, Germany

Manufactured by
Pfizer Inc., New York, NY 10001
LAB-1571-6.0
Revised: 22 August 2024
Patient Counseling Information
Your child is being offered the Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula)10 to prevent coronavirus disease 2019 (COVID-19), which is caused by the virus SARS-CoV-2.11 This Fact Sheet contains information to help you understand the risks and benefits of the Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula), hereafter referred to as Pfizer-BioNTech COVID-19 Vaccine, which your child may receive because there is currently a pandemic of COVID-19. Talk to your child’s vaccination provider if you have questions.
This Fact Sheet may have been updated. For the most recent Fact Sheet, please see https://www.covidvaxoption.com
The U.S. Food and Drug Administration (FDA) has issued an Emergency Use Authorization (EUA) to make the Pfizer-BioNTech COVID-19 Vaccine available during the COVID-19 pandemic (for more details about an EUA please see “WHAT IS AN EMERGENCY USE AUTHORIZATION?” at the end of this document). The Pfizer-BioNTech COVID-19 Vaccine is not an FDA-approved vaccine in the United States. Read this Fact Sheet for information about the Pfizer-BioNTech COVID-19 Vaccine.
WHAT IS COVID-19?
COVID-19 is caused by a coronavirus called SARS-CoV-2. You can get COVID-19 through close contact with another person who has the virus.
It is predominantly a respiratory illness that can affect other organs. People with COVID-19 have had a wide range of symptoms reported, ranging from mild symptoms to severe illness leading to death. Symptoms may appear 2 to 14 days after exposure to the virus. Symptoms may include: fever or chills; cough; shortness of breath; fatigue; muscle or body aches; headache; new loss of taste or smell; sore throat; congestion or runny nose; nausea or vomiting; diarrhea.
WHAT IS THE PFIZER-BIONTECH COVID-19 VACCINE?
The Pfizer-BioNTech COVID-19 Vaccine is a vaccine for use in individuals 6 months through 11 years of age to prevent COVID-19. The FDA has authorized the emergency use of the Pfizer-BioNTech COVID-19 Vaccine under an EUA.
The Pfizer-BioNTech COVID-19 Vaccine may not protect everyone.
WHAT SHOULD YOU MENTION TO THE VACCINATION PROVIDER BEFORE YOUR CHILD GETS THE PFIZER-BIONTECH COVID-19 VACCINE?
Tell the vaccination provider about all of your child’s medical conditions, including if your child:
- •
- has any allergies
- •
- has had myocarditis (inflammation of the heart muscle) or pericarditis (inflammation of the lining outside the heart)
- •
- has a fever
- •
- has a bleeding disorder or is on a blood thinner
- •
- is immunocompromised or is on a medicine that affects the immune system
- •
- is pregnant
- •
- is breastfeeding
- •
- has received another COVID-19 vaccine
- •
- has ever fainted in association with an injection
HOW IS THE VACCINE GIVEN?
The Pfizer-BioNTech COVID-19 Vaccine is given as an injection into the muscle.
Individuals 6 months through 4 years of age
- •
- Unvaccinated individuals: Three doses of Pfizer-BioNTech COVID-19 Vaccine are administered over at least 11 weeks. The first 2 doses are administered 3 weeks apart. The third dose is administered at least 8 weeks after the second dose.
- •
- Individuals who have received 1 previous dose of the Pfizer-BioNTech COVID-19 Vaccine12: Two doses of Pfizer-BioNTech COVID-19 Vaccine are administered. The first dose of Pfizer-BioNTech COVID-19 Vaccine is administered 3 weeks after the previous dose of a Pfizer-BioNTech COVID-19 Vaccine and the second dose at least 8 weeks later.
- •
- Individuals who have received 2 or more previous doses of the Pfizer-BioNTech COVID-19 Vaccine12: A single dose of Pfizer-BioNTech COVID-19 Vaccine is administered at least 8 weeks after the last previous dose of a Pfizer-BioNTech COVID-19 Vaccine.
Individuals 5 through 11 years of age
A single dose of Pfizer-BioNTech COVID-19 Vaccine is administered to individuals who have not received a COVID-19 vaccine (2024-2025 Formula). You must wait at least 2 months since your last dose of any COVID-19 vaccine.
Immunocompromised individuals 6 months through 11 years of age
Additional doses of Pfizer-BioNTech COVID-19 Vaccine may be administered. For more information, talk to your child’s healthcare provider.
WHO SHOULD NOT GET PFIZER-BIONTECH COVID-19 VACCINE?
Your child should not get Pfizer-BioNTech COVID-19 Vaccine if they had:
- •
- a severe allergic reaction after a previous dose of any Pfizer-BioNTech COVID-19 vaccine
- •
- a severe allergic reaction to any ingredient in these vaccines.
WHAT ARE THE INGREDIENTS IN THIS VACCINE?
Pfizer-BioNTech COVID-19 Vaccine contains the following ingredients: messenger ribonucleic acid (mRNA), lipids (((4-hydroxybutyl)azanediyl)bis(hexane-6,1-diyl)bis(2-hexyldecanoate), 2 [(polyethylene glycol)-2000]-N,N-ditetradecylacetamide, 1,2-distearoyl-sn-glycero-3-phosphocholine, and cholesterol), tromethamine, tromethamine hydrochloride, and sucrose. Pfizer-BioNTech COVID-19 for use in individuals 6 months through 4 years of age also contains sodium chloride.
HAS THIS VACCINE BEEN USED BEFORE?
Millions of individuals 6 months of age and older have received a Pfizer-BioNTech COVID-19 vaccine under EUA.
In a clinical trial, approximately 1,200 individuals 6 months through 23 months of age, approximately 1,800 individuals 2 through 4 years of age, and approximately 3,100 individuals 5 through 11 years of age have received at least 1 dose of the Pfizer-BioNTech COVID-19 Vaccine (Original monovalent)13. In another clinical trial, approximately 23,000 individuals 12 years of age and older have received at least 1 dose of the Pfizer-BioNTech COVID-19 Vaccine (Original monovalent).
In clinical trials, 60 individuals 6 months through 4 years of age, 113 individuals 5 through 11 years of age, 107 individuals 12 through 17 years of age, 103 individuals 18 through 55 years of age, and 106 individuals greater than 55 years of age received a dose of Pfizer-BioNTech COVID-19 Vaccine, Bivalent.14
WHAT ARE THE BENEFITS OF PFIZER-BIONTECH COVID-19 VACCINE?
FDA has authorized the Pfizer-BioNTech COVID-19 Vaccine to provide protection against COVID-19.
The duration of protection against COVID-19 is currently unknown.
WHAT ARE THE RISKS OF PFIZER-BIONTECH COVID-19 VACCINE?
There is a remote chance that the vaccine could cause a severe allergic reaction. A severe allergic reaction would usually occur within a few minutes to one hour after getting a dose. For this reason, the vaccination provider may ask your child to stay at the place where your child received the vaccine for monitoring after vaccination. Signs of a severe allergic reaction can include:
- •
- Difficulty breathing
- •
- Swelling of the face and throat
- •
- A fast heartbeat
- •
- A bad rash all over the body
- •
- Dizziness and weakness
Myocarditis (inflammation of the heart muscle) and pericarditis (inflammation of the lining outside the heart) have occurred in some people who have received mRNA COVID-19 vaccines. Myocarditis and pericarditis following Pfizer-BioNTech COVID-19 Vaccines have occurred most commonly in adolescent males 12 through 17 years of age. In most of these individuals, symptoms began within a few days following vaccination. The chance of having this occur is very low. You should seek medical attention right away if your child has any of the following symptoms after receiving the vaccine, particularly during the 2 weeks after your child receives a dose of the vaccine:
- •
- Chest pain
- •
- Shortness of breath or difficulty breathing
- •
- Feelings of having a fast-beating, fluttering, or pounding heart
Additional symptoms, particularly in children, may include:
- •
- Fainting
- •
- Unusual and persistent irritability
- •
- Unusual and persistent poor feeding
- •
- Unusual and persistent fatigue or lack of energy
- •
- Persistent vomiting
- •
- Persistent pain in the abdomen
- •
- Unusual and persistent cool, pale skin
Side effects that have been reported with Pfizer-BioNTech COVID-19 Vaccines include:
- •
- Severe allergic reactions
- •
- Non-severe allergic reactions such as rash, itching, hives, or swelling of the face
- •
- Myocarditis (inflammation of the heart muscle)
- •
- Pericarditis (inflammation of the lining outside the heart)
- •
- Injection site pain/tenderness
- •
- Tiredness
- •
- Headache
- •
- Muscle pain
- •
- Chills
- •
- Joint pain
- •
- Fever
- •
- Injection site swelling
- •
- Injection site redness
- •
- Nausea
- •
- Feeling unwell
- •
- Swollen lymph nodes (lymphadenopathy)
- •
- Decreased appetite
- •
- Diarrhea
- •
- Vomiting
- •
- Arm pain
- •
- Fainting in association with injection of the vaccine
- •
- Dizziness
- •
- Irritability
- •
- Febrile seizures (convulsions during a fever)
These may not be all the possible side effects. Serious and unexpected side effects may occur. The possible side effects are still being studied.
WHAT SHOULD I DO ABOUT SIDE EFFECTS?
If your child experiences a severe allergic reaction, call 9-1-1, or go to the nearest hospital.
Call the vaccination provider or your child’s healthcare provider if your child has any side effects that bother your child or do not go away.
Report vaccine side effects to FDA/CDC Vaccine Adverse Event Reporting System (VAERS). The VAERS toll-free number is 1-800-822-7967 or report online to https://vaers.hhs.gov/reportevent.html. Please include “Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula) EUA” in the first line of box #18 of the report form.
In addition, you can report side effects to Pfizer Inc. at the contact information provided below.
| Website | Fax number | Telephone number |
|---|---|---|
|
www.pfizersafetyreporting.com |
1-866-635-8337 |
1-800-438-1985 |
WHAT IF I DECIDE NOT TO HAVE MY CHILD GET THE PFIZER-BIONTECH COVID-19 VACCINE?
Under the EUA, there is an option to accept or refuse receiving this vaccine. Should you decide for your child not to receive this vaccine, it will not change the standard medical care.
ARE THERE OTHER VACCINES FOR PREVENTING COVID-19 BESIDES THE PFIZER-BIONTECH COVID-19 VACCINE?
Other vaccines to prevent COVID-19 may be available under EUA, including vaccines that encode the spike protein of the SARS-CoV-2 Omicron variant lineage KP.2.
CAN MY CHILD RECEIVE PFIZER-BIONTECH COVID-19 VACCINE AT THE SAME TIME AS OTHER VACCINES?
If you are considering having your child receive Pfizer-BioNTech COVID-19 Vaccine with other vaccines, discuss the options with your child’s healthcare provider.
WHAT IF MY CHILD IS IMMUNOCOMPROMISED?
Immunocompromised individuals 6 months through 11 years of age may receive additional doses of Pfizer-BioNTech COVID-19 Vaccine (see HOW IS THE VACCINE GIVEN? above).
Vaccinations may not provide full immunity to COVID-19 in people who are immunocompromised; therefore, your child should continue to maintain physical precautions to help prevent COVID-19. Your child’s close contacts should be vaccinated as appropriate.
WHAT ABOUT PREGNANCY OR BREASTFEEDING?
If your child is pregnant or breastfeeding, discuss the options with your child’s healthcare provider.
WILL THIS VACCINE GIVE MY CHILD COVID-19?
No. This vaccine does not contain SARS-CoV-2 and cannot give your child COVID-19.
ADDITIONAL INFORMATION
If you have questions, visit the website or call the telephone number provided below.
To access the most recent Fact Sheets, please scan the QR code provided below.
HOW CAN I LEARN MORE?
- •
- Ask the vaccination provider.
- •
- Visit CDC at https://www.cdc.gov/coronavirus/2019-ncov/index.html.
- •
- Visit FDA at https://www.fda.gov/emergency-preparedness-and-response/mcm-legal-regulatory-and-policy-framework/emergency-use-authorization.
- •
- Contact your local or state public health department.
WHERE WILL VACCINATION INFORMATION BE RECORDED?
The vaccination provider may include your child’s vaccination information in your state/local jurisdiction’s Immunization Information System (IIS) or other designated system. For more information about IISs, visit: https://www.cdc.gov/vaccines/programs/iis/about.html
WHAT IS THE COUNTERMEASURES INJURY COMPENSATION PROGRAM?
The Countermeasures Injury Compensation Program (CICP) is a federal program that may help pay for costs of medical care and other specific expenses of certain people who have been seriously injured by certain medicines or vaccines, including this vaccine. Generally, a claim must be submitted to the CICP within one (1) year from the date of receiving the vaccine. To learn more about this program, visit www.hrsa.gov/cicp/ or call 1-855-266-2427.
WHAT IS AN EMERGENCY USE AUTHORIZATION (EUA)?
The FDA has made Pfizer-BioNTech COVID-19 Vaccine available under an emergency access mechanism called an EUA. An EUA is supported by a Secretary of Health and Human Services (HHS) declaration that circumstances exist to justify the emergency use of drugs and biological products during the COVID-19 pandemic. A product authorized for emergency use has not undergone the same type of review by FDA as an FDA-approved product.
FDA may issue an EUA when certain criteria are met, which includes that there are no adequate, approved, and available alternatives. In addition, the FDA decision is based on the totality of the scientific evidence available showing that the product may be effective to prevent COVID-19 during the COVID-19 pandemic and that the known and potential benefits of the product outweigh the known and potential risks of the product. All of these criteria must be met to allow for the product to be used under EUA during the COVID-19 pandemic.
The EUA is in effect for the duration of the COVID-19 EUA declaration justifying emergency use of this product, unless terminated or revoked (after which the product may no longer be used under the EUA).

Manufactured for
BioNTech Manufacturing GmbH
An der Goldgrube 12
55131 Mainz, Germany

Manufactured by
Pfizer Inc., New York, NY 10001
LAB-1572-4.0
Revised: 22 August 2024
 |
Scan to capture that this Fact Sheet was provided to vaccine recipient for the electronic medical records/immunization information systems. |
|
GDTI: 0886983000585 |
|
- 10
- The Pfizer-BioNTech COVID-19 Vaccine (2024-2025 Formula) encodes the spike protein of SARS CoV 2 Omicron variant lineage KP.2.
- 11
- If your child is immunocompromised and turning from 11 to 12 years of age during the vaccination series for immunocompromised individuals, you may receive this Fact Sheet because your child is being offered COMIRNATY (COVID-19 Vaccine, mRNA) (2024-2025 Formula) (hereafter referred to as COMIRNATY). COMIRNATY is an FDA-approved vaccine for prevention of COVID-19 in individuals 12 years of age and older that is authorized under EUA to complete the dosing schedule for immunocompromised individuals who turn from 11 years to 12 years of age during the vaccination series. Under the authorized dosing schedule, these individuals receive the Pfizer-BioNTech COVID-19 Vaccine before they turn 12 years old, and complete the vaccination series with COMIRNATY on or after the date the individual turns 12 years old. The dosing schedule is: Dose 1: Week 0; Dose 2: Week 3; Dose 3: ≥4 weeks after Dose 2. The information in this Fact Sheet about the Pfizer-BioNTech COVID-19 Vaccine, including information about the benefits, risks, and ingredients of that vaccine, also applies to your child’s use of COMIRNATY, except with respect to the dosing schedule and the ages authorized for use.
- 12
- Previous dose refers to a dose of any prior Pfizer-BioNTech COVID-19 Vaccine that is no longer authorized for use in the United States.
- 13
- Pfizer-BioNTech COVID-19 Vaccine (Original monovalent) refers to Pfizer-BioNTech COVID-19 Vaccine that encodes the spike protein of only the Original SARS CoV-2. This vaccine is no longer authorized for use in the United States.
- 14
- Pfizer-BioNTech COVID-19 Vaccine, Bivalent refers to Pfizer-BioNTech COVID-19 vVaccine that encodes the spike protein of the Original SARS CoV 2 and the Omicron BA.4/BA.5 SARS-CoV-2. This vaccine is no longer authorized for use in the United States.
PRINCIPAL DISPLAY PANEL – 3 Doses of 0.3 mL Multiple Dose Vial Label 2024-2025 Formula
Pfizer-BioNTech COVID-19 Vaccine
2024 – 2025 Formula
DILUTE PRIOR TO USE
Age 6m to < 5y
After dilution – 3 doses of 0.3 mL
For intramuscular use. Contains no preservative.
For use under Emergency Use Authorization.
After dilution store at 2 to 25°C (35 to 77°F) and
discard after 12 hours.
Dilution date and time:
NDC 59267-4426-1
PRINCIPAL DISPLAY PANEL – 10 Multiple Dose Vial Carton 2024-2025 Formula
Pfizer-BioNTech
COVID-19 Vaccine
NDC 59267-4426-2
2024 – 2025 Formula
Suspension for Intramuscular Injection
DILUTE PRIOR TO USE
10 Multiple Dose Vials
After dilution each vial contains 3 doses of 0.3 mL
For age 6 months to < 5 years
For use under Emergency Use Authorization.
BIONTECH
Pfizer
Rx only
PRINCIPAL DISPLAY PANEL - 0.3 mL Single Dose Vial Label 2024-2025 Formula
Pfizer-BioNTech COVID-19 Vaccine
2024 – 2025 Formula
DO NOT DILUTE
Age 5y to < 12y
Vial contains 1 dose of 0.3 mL
For intramuscular use.
For use under Emergency Use Authorization.
NDC 59267-4438-1
PRINCIPAL DISPLAY PANEL – 10 Single Dose Vial Carton 2024-2025 Formula
Pfizer-BioNTech
COVID-19 Vaccine
NDC 59267-4438-2
2024 – 2025 Formula
Suspension for Intramuscular Injection
DO NOT DILUTE
10 Single Dose Vials
Each vial contains 1 dose of 0.3 mL
For age 5 years to < 12 years
For use under Emergency Use Authorization.
BIONTECH
Pfizer
Rx only
| PFIZER-BIONTECH COVID-19 VACCINE
covid-19 vaccine, mrna injection, suspension |
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
| PFIZER-BIONTECH COVID-19 VACCINE
covid-19 vaccine, mrna injection, suspension |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Pfizer Manufacturing Belgium NV (370156507) |
| Registrant - Pfizer Inc (113480771) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Pfizer Manufacturing Belgium NV | 370156507 | ANALYSIS(59267-4426, 59267-4438) , MANUFACTURE(59267-4426, 59267-4438) , PACK(59267-4426, 59267-4438) , LABEL(59267-4426, 59267-4438) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Wyeth BioPharma Division of Wyeth Pharmaceuticals LLC | 174350868 | ANALYSIS(59267-4426, 59267-4438) , API MANUFACTURE(59267-4426, 59267-4438) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Pfizer Ireland Pharmaceuticals Unlimited Company | 985586408 | ANALYSIS(59267-4426, 59267-4438) , API MANUFACTURE(59267-4426, 59267-4438) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| BioNTech Innovative Manufacturing Services GmbH | 537365801 | ANALYSIS(59267-4426, 59267-4438) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| BioNTech Manufacturing GmbH | 314382536 | ANALYSIS(59267-4426, 59267-4438) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| BioNTech Manufacturing Marburg GmbH | 313270335 | ANALYSIS(59267-4426, 59267-4438) , API MANUFACTURE(59267-4426, 59267-4438) | |
More about COVID-19 mRNA (Pfizer) vaccine
- Check interactions
- Compare alternatives
- Reviews (17)
- Side effects
- Dosage information
- During pregnancy
- Drug class: viral vaccines
Patient resources
Professional resources
- COVID-19 Vaccine, mRNA (Pfizer-BioNTech) (2024-2025 Formula) monograph
- Covid-19 Vaccine Pfizer (FDA)
- Covid-19 Vaccine Pfizer, Monovalent, 6 mo-4 yr (FDA)
- Covid-19 Vaccine Pfizer, Monovalent,5 yr to 11 yr (FDA)
- Pfizer-BioNTech Vaccine (FDA)