Fosaprepitant
Medically reviewed by Drugs.com. Last updated on May 21, 2024.
Pronunciation
(fos a PRE pi tant)
Index Terms
- Fosaprepitant Dimeglumine
- L-758,298
- MK 0517
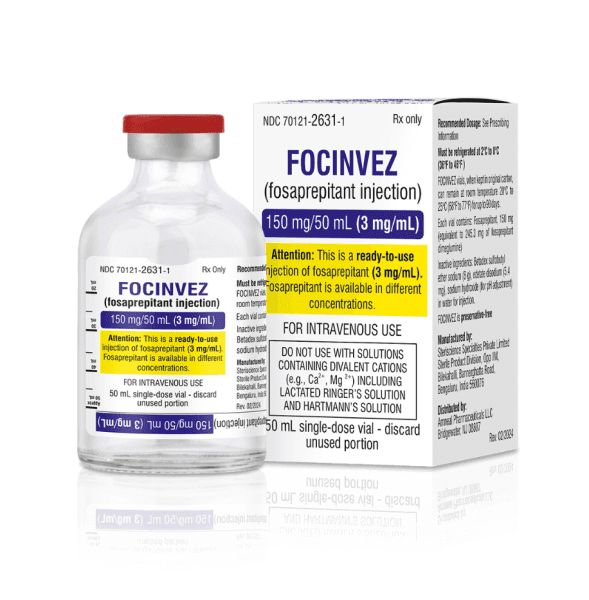
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Solution Reconstituted, Intravenous:
Generic: 150 mg (1 ea)
Solution Reconstituted, Intravenous [preservative free]:
Emend: 150 mg (1 ea [DSC]) [contains disodium edta, lactose, polysorbate 80]
Emend: 150 mg (1 ea) [contains edetate disodium, lactose, polysorbate 80]
Generic: 150 mg (1 ea)
Brand Names: U.S.
- Emend
Pharmacologic Category
- Antiemetic
- Substance P/Neurokinin 1 Receptor Antagonist
Pharmacology
Fosaprepitant is a prodrug of aprepitant, a substance P/neurokinin 1 (NK1) receptor antagonist. Fosaprepitant is rapidly converted to aprepitant, which prevents acute and delayed vomiting by inhibiting the substance P/neurokinin 1 (NK1) receptor; also augments the antiemetic activity of the 5-HT3 receptor antagonist and corticosteroid activity and inhibits chemotherapy-induced emesis.
Distribution
Aprepitant: Vd: ~70 L; crosses the blood-brain barrier
Metabolism
Fosaprepitant: Hepatic and extrahepatic; rapidly (within 30 minutes after the end of infusion) converted to aprepitant (nearly complete conversion)
Aprepitant: Hepatic via CYP3A4 (major); CYP1A2 and CYP2C19 (minor); forms 7 weakly-active metabolites
Excretion
Urine (57%); feces (45%)
Time to Peak
Fosaprepitant is converted to aprepitant within 30 minutes after the end of infusion
Half-Life Elimination
Aprepitant: ~9 to 13 hours
Protein Binding
Aprepitant: >95%
Special Populations: Renal Function Impairment
Following a single oral aprepitant 240 mg dose in patients with severe renal impairment (CrCl <30 mL/minute), the AUC of total aprepitant (unbound and protein bound) decreased by 21% and Cmax decreased by 32% compared with healthy subjects. In patients with ESRD undergoing hemodialysis, the AUC of total aprepitant decreased by 42% and Cmax decreased by 32%. Hemodialysis conducted 4 or 48 hours after aprepitant dosing had no significant impact on aprepitant pharmacokinetics.
Special Populations: Hepatic Function Impairment
Following oral administration of aprepitant 125 mg on day 1 and 80 mg once daily on days 2 and 3 to patients with mild hepatic impairment (Child-Pugh score 5 to 6), the AUC of aprepitant was 11% lower on day 1 and 36% lower on day 3 (compared to healthy subjects); in patients with moderate hepatic impairment (Child-Pugh score 7 to 9), the AUC of aprepitant was 10% higher on day 1 and 18% higher on day 3 (compared to healthy subjects). These differences are not considered clinically meaningful.
Special Populations: Elderly
Following oral administration of aprepitant 125 mg on day 1 and 80 mg once daily on days 2 through 5, the AUC of aprepitant was 21% higher on day 1 and 36% higher on day 5 in elderly patients; the Cmax was 10% higher on day 1 and 24% higher on day 5 in elderly patients (relative to younger adults). These differences are not considered clinically meaningful.
Special Populations: Gender
Following a single oral aprepitant dose (ranging from 40 to 375 mg), the AUC was 9% higher and the Cmax was 17% higher in females (compared with males); the half-life of aprepitant is approximately 25% lower in females (compared with males). These differences are not considered clinically meaningful.
Special Populations: Race
Following a single oral aprepitant dose (ranging from 40 to 375 mg), the AUC of aprepitant was ~27% higher and the Cmax was ~19% higher in Hispanic patients compared with Caucasian patients; the AUC of aprepitant was 74% higher and the Cmax was 47% higher in Asian patients compared with Caucasian patients. These differences are not considered clinically meaningful.
Special Populations Note
Obesity: In an analysis of subjects with BMIs ranging from 18 kg/m2 to 36 kg/m2, for every 5 kg/m2 increase in BMI, the AUC and Cmax of aprepitant decrease by 9% and 10%, respectively. These differences are not considered clinically meaningful.
Use: Labeled Indications
Prevention of chemotherapy-induced nausea and vomiting:
Prevention of acute and delayed nausea and vomiting associated with highly emetogenic chemotherapy, including high-dose cisplatin (initial and repeat courses; in combination with other antiemetics) in patients ≥6 months of age
Prevention of delayed nausea and vomiting associated with moderately emetogenic chemotherapy (initial and repeat courses; in combination with other antiemetics) in patients ≥6 months of age
Limitations of use: Fosaprepitant has not been studied for the management of existing nausea and vomiting.
Contraindications
Hypersensitivity to fosaprepitant or any component of the formulation; concurrent use with pimozide
Canadian labeling: Additional contraindications (not in the US labeling): Concurrent use with astemizole, terfenadine, or cisapride
Dosing: Adult
Note: Dosing is for fosaprepitant (Emend IV); refer to the aprepitant monograph for IV aprepitant (Cinvanti) dosing.
Prevention of chemotherapy-induced nausea/vomiting:
Highly emetogenic chemotherapy: IV: 150 mg on day 1 only (infusion should be completed ~30 minutes prior to chemotherapy); administer in combination with a 5-HT3 antagonist on day 1 only and with dexamethasone on days 1 to 4 (reduce dexamethasone dose by 50% on days 1 and 2).
Moderately emetogenic chemotherapy: IV: 150 mg on day 1 only (infusion should be completed ~30 minutes prior to chemotherapy); administer in combination with a 5-HT3 antagonist and dexamethasone on day 1 (reduce dexamethasone dose by 50%).
Dosage adjustment for concomitant therapy: Significant drug interactions exist, requiring dose/frequency adjustment or avoidance. Consult drug interactions database for more information.
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Chemotherapy-induced nausea/vomiting, prevention; highly and moderately emetogenic chemotherapy:
Infants ≥6 months weighing ≥6 kg and Children <2 years:
Single-dose NK1 receptor antagonist regimen: Note: Use only with single-day chemotherapy regimens. IV: 5 mg/kg once; maximum dose: 150 mg/dose; administer ~90 minutes prior to chemotherapy on day 1 only; use in combination with a 5-HT3 antagonist with or without corticosteroid.
Three-day NK1 receptor antagonist regimen: Note: May be used with single-day or multiday chemotherapy regimens. IV: 3 mg/kg once; maximum dose: 115 mg/dose; administer ~90 minutes prior to chemotherapy on day 1 only followed by oral aprepitant on days 2 and 3; use in combination with a 5-HT3 antagonist with or without corticosteroid.
Children 2 to <12 years:
Single-dose NK1 receptor antagonist regimen: Note: Use only with single-day chemotherapy regimens. IV: 4 mg/kg once; maximum dose: 150 mg/dose; administer ~90 minutes prior to chemotherapy on day 1 only; use in combination with a 5-HT3 antagonist with or without corticosteroid.
Three-day NK1 receptor antagonist regimen: Note: May be used with single-day or multiday chemotherapy regimens. IV: 3 mg/kg once; maximum dose: 115 mg/dose; administer ~90 minutes prior to chemotherapy on day 1 only followed by oral aprepitant on days 2 and 3; use in combination with a 5-HT3 antagonist with or without corticosteroid.
Children ≥12 years and Adolescents ≤17 years:
Single-dose NK1 receptor antagonist regimen: Note: Use only with single-day chemotherapy regimens. IV: 150 mg once, administered ~60 minutes prior to chemotherapy on day 1 only; use in combination with a 5-HT3 antagonist with or without corticosteroid.
Three-day NK1 receptor antagonist regimen: Note: May be used with single-day or multiday chemotherapy regimens. IV: 115 mg once, administered ~60 minutes prior to chemotherapy on day 1 only followed by oral aprepitant on days 2 and 3; use in combination with a 5-HT3 antagonist with or without corticosteroid.
Adolescents ≥18 years: Single-dose NK1 receptor antagonist regimen: IV: 150 mg once, administer ~50 to 60 minutes prior to chemotherapy on day 1 only; in combination with a 5-HT3 antagonist and corticosteroid.
Dosage adjustment for concomitant therapy: Significant drug interactions exist, requiring dose/frequency adjustment or avoidance. Consult drug interactions database for more information.
Reconstitution
Reconstitute vial with 5 mL of NS, slowly directing diluent down wall of vial to avoid foaming; swirl gently. Add reconstituted contents of the 150 mg vial to 145 mL NS (total volume of 150 mL), resulting in a final concentration of 1 mg/mL; gently invert bag 2 to 3 times to mix. For doses <150 mg (resulting in an infusion volume <150 mL), transfer calculated volume to an appropriate size bag or syringe prior to infusion. Solutions diluted to a final volume of 250 mL (0.6 mg/mL) have also been reported (Chau 2019).
Administration
IV: Infuse over 20 to 30 minutes; infusion should be completed ~30 minutes prior to chemotherapy.
Note: Administration information is for fosaprepitant (Emend IV); refer to the aprepitant monograph for IV aprepitant (Cinvanti) administration.
Storage
Store intact vials at 2°C to 8°C (36°F to 46°F). Solutions diluted to 1 mg/mL for infusion are stable for 24 hours at room temperature at ≤25°C (≤77°F). Solutions diluted in NS to a final volume of 250 mL (0.6 mg/mL) should be administered within 24 hours (data on file [Merck 2013]).
Drug Interactions
Abametapir: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Astemizole: Fosaprepitant may increase the serum concentration of Astemizole. The active metabolite aprepitant is likely responsible for this effect. Avoid combination
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Corticosteroids (Systemic): Fosaprepitant may increase the serum concentration of Corticosteroids (Systemic). The active metabolite aprepitant is likely responsible for this effect. Management: Reduce the dose of corticosteroids, such as dexamethasone or oral methylprednisolone, by 50% when coadministered with fosaprepitant. Reduce intravenous methylprednisolone doses by 25% during coadministration with fosaprepitant. Consider therapy modification
CYP3A4 Inducers (Moderate): May decrease the serum concentration of Fosaprepitant. Specifically, CYP3A4 Inducers (Moderate) may decrease serum concentrations of the active metabolite aprepitant. Monitor therapy
CYP3A4 Inducers (Strong): May decrease the serum concentration of Fosaprepitant. Specifically, CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite aprepitant. Avoid combination
CYP3A4 Inhibitors (Moderate): May increase the serum concentration of Fosaprepitant. Avoid combination
CYP3A4 Inhibitors (Strong): May increase the serum concentration of Fosaprepitant. Avoid combination
CYP3A4 Substrates (High risk with Inhibitors): Fosaprepitant may increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to concomitant therapy when possible. If concomitant therapy cannot be avoided, monitor for reduced clinical effects of the CYP3A4 substrate. Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Dofetilide: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Dofetilide. Monitor therapy
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Estrogen Derivatives (Contraceptive): Fosaprepitant may decrease the serum concentration of Estrogen Derivatives (Contraceptive). The active metabolite aprepitant is likely responsible for this effect. Management: Alternative or additional methods of contraception should be used both during treatment with fosaprepitant or aprepitant and for at least one month following the last fosaprepitant/aprepitant dose. Consider therapy modification
Flibanserin: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Flibanserin. Monitor therapy
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Ifosfamide: Fosaprepitant may increase the serum concentration of Ifosfamide. Specifically, concentrations of the toxic metabolites of ifosfamide may increase. Monitor therapy
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Lemborexant: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Lemborexant. Management: The maximum recommended dosage of lemborexant is 5 mg, no more than once per night, when coadministered with weak CYP3A4 inhibitors. Consider therapy modification
Lomitapide: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Lomitapide. Management: Patients on lomitapide 5 mg/day may continue that dose. Patients taking lomitapide 10 mg/day or more should decrease the lomitapide dose by half. The lomitapide dose may then be titrated up to a max adult dose of 30 mg/day. Consider therapy modification
NiMODipine: CYP3A4 Inhibitors (Weak) may increase the serum concentration of NiMODipine. Monitor therapy
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
PARoxetine: May decrease serum concentrations of the active metabolite(s) of Fosaprepitant. Fosaprepitant may decrease the serum concentration of PARoxetine. Monitor therapy
Pimozide: Fosaprepitant may increase the serum concentration of Pimozide. The active metabolite aprepitant is likely responsible for this effect. Avoid combination
Progestins (Contraceptive): Fosaprepitant may decrease the serum concentration of Progestins (Contraceptive). The active metabolite aprepitant is likely responsible for this effect. Management: Alternative or additional methods of contraception should be used both during treatment with aprepitant or fosaprepitant and for at least one month following the last aprepitant/fosaprepitant dose. Consider therapy modification
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Tacrolimus (Systemic): CYP3A4 Inhibitors (Weak) may increase the serum concentration of Tacrolimus (Systemic). Monitor therapy
Terfenadine: Fosaprepitant may increase the serum concentration of Terfenadine. The active metabolite aprepitant is likely responsible for this effect. Avoid combination
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Triazolam: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Triazolam. Management: Consider triazolam dose reduction in patients receiving concomitant weak CYP3A4 inhibitors. Consider therapy modification
Ubrogepant: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Ubrogepant. Management: In patients taking weak CYP3A4 inhibitors, the initial and second dose (given at least 2 hours later if needed) of ubrogepant should be limited to 50 mg. Consider therapy modification
Vitamin K Antagonists (eg, warfarin): Fosaprepitant may decrease the serum concentration of Vitamin K Antagonists. Monitor therapy
Adverse Reactions
The following adverse drug reactions and incidences are derived from product labeling unless otherwise specified.
Adverse reactions reported with fosaprepitant (as part of a combination chemotherapy regimen) occurring at a higher frequency than standard antiemetic therapy. Also see aprepitant monograph for additional adverse reactions.
>10%:
Central nervous system: Fatigue (15%)
Gastrointestinal: Diarrhea (13%)
1% to 10%:
Central nervous system: Peripheral neuropathy (3%)
Gastrointestinal: Dyspepsia (2%)
Genitourinary: Urinary tract infection (2%)
Hematologic & oncologic: Neutropenia (8%), anemia (3%), leukopenia (2%)
Local: Infusion-site reaction (2% to 3%; includes induration at injection site, infusion-site pain, local pruritus, localized erythema)
Neuromuscular & skeletal: Weakness (4%), limb pain (2%)
<1%, postmarketing, and/or case reports: Anaphylactic shock, anaphylaxis, dyspnea, erythema, flushing, hypersensitivity reaction, hypotension, pruritus, skin rash, Stevens-Johnson syndrome, syncope, toxic epidermal necrolysis, urticaria
Related/similar drugs
Reglan
Reglan (metoclopramide) is used to treat heartburn caused by gastric reflux. Includes Reglan side ...
Decadron
Decadron is used for addison's disease, adrenal insufficiency, adrenocortical insufficiency ...
Ozempic
Learn about Ozempic (semaglutide) for type 2 diabetes treatment, weight management, cardiovascular ...
Zofran ODT
Zofran ODT is used for nausea/vomiting, nausea/vomiting, chemotherapy induced, nausea/vomiting ...
Dronabinol
Dronabinol systemic is used for AIDS Related Wasting, anorexia, nausea/vomiting, nausea/vomiting ...
Metoclopramide
Metoclopramide is used short-term to treat heartburn caused by gastroesophageal reflux. Learn about ...
Ativan
Ativan is a benzodiazepine used to treat anxiety disorders or anxiety associated with depression ...
Diphenhydramine
Diphenhydramine is an antihistamine used to treat sneezing, runny nose, itching, hives and other ...
Meclizine
Meclizine is used to treat or prevent nausea, vomiting, and dizziness caused by motion sickness ...
Promethazine
Promethazine is a phenothiazine and antihistamine used to treat allergies, motion sickness, nausea ...
Warnings/Precautions
Concerns related to adverse effects:
• Hypersensitivity: Hypersensitivity reactions, including dyspnea, erythema, flushing, hypotension, syncope, and anaphylaxis/anaphylactic shock have been reported during infusions; if symptoms occur, stop infusion; do not reinitiate.
• Infusion-site reactions: Infusion-site reactions, including erythema, pain, edema, thrombophlebitis, pruritus, and injection-site induration have occurred; the majority of severe infusion-related reactions (including thrombophlebitis, vasculitis, and necrosis) have been reported with administration of concomitant vesicant (anthracycline-based) chemotherapy, particularly when associated with extravasation. Most reactions occurred with the first three exposures to single fosaprepitant injections; some reactions persisted ≥2 weeks. Avoid infusing fosaprepitant into small veins or through a butterfly catheter. If a severe infusion-site reaction occurs, stop infusion and administer appropriate therapy.
Dosage form specific issues:
• Polysorbate 80: Some dosage forms may contain polysorbate 80 (also known as Tweens). Hypersensitivity reactions, usually a delayed reaction, have been reported following exposure to pharmaceutical products containing polysorbate 80 in certain individuals (Isaksson 2002; Lucente 2000; Shelley 1995). Thrombocytopenia, ascites, pulmonary deterioration, and renal and hepatic failure have been reported in premature neonates after receiving parenteral products containing polysorbate 80 (Alade 1986; CDC 1984). See manufacturer's labeling.
Other warnings/precautions:
• Appropriate use: Chronic continuous administration is not recommended.
Monitoring Parameters
Monitor INR in patients on chronic warfarin therapy in the 2-week period (particularly at 7 to 10 days) following fosaprepitant administration; monitor for signs/symptoms of hypersensitivity and infusion site reactions.
Reproductive Considerations
Efficacy of hormonal contraceptive may be reduced; alternative or additional methods of contraception should be used during treatment with fosaprepitant and for at least 1 month following the last fosaprepitant dose.
Pregnancy Considerations
Adverse events were not observed in animal reproduction studies.
Patient Education
What is this drug used for?
• It is used to prevent upset stomach and throwing up from chemo.
• It may be given for other reasons. Talk with the doctor.
All drugs may cause side effects. However, many people have no side effects or only have minor side effects. Call your doctor or get medical help if any of these side effects or any other side effects bother you or do not go away:
• Diarrhea
• Painful extremities
• Abdominal pain
• Heartburn
WARNING/CAUTION: Even though it may be rare, some people may have very bad and sometimes deadly side effects when taking a drug. Tell your doctor or get medical help right away if you have any of the following signs or symptoms that may be related to a very bad side effect:
• Urinary tract infection like blood in the urine, burning or painful urination, passing a lot of urine, fever, lower abdominal pain, or pelvic pain
• Infection
• Flushing
• Dizziness
• Passing out
• Fast heartbeat
• Abnormal heartbeat
• Burning or numbness feeling
• Bruising
• Bleeding
• Severe loss of strength and energy
• Severe injection site redness, swelling, blisters, burning, pain or irritation
• Signs of an allergic reaction, like rash; hives; itching; red, swollen, blistered, or peeling skin with or without fever; wheezing; tightness in the chest or throat; trouble breathing, swallowing, or talking; unusual hoarseness; or swelling of the mouth, face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a limited summary of general information about the medicine’s uses from the patient education leaflet and is not intended to be comprehensive. This limited summary does NOT include all information available about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not intended to provide medical advice, diagnosis or treatment and does not replace information you receive from the healthcare provider. For a more detailed summary of information about the risks and benefits of using this medicine, please speak with your healthcare provider and review the entire patient education leaflet.
Frequently asked questions
More about fosaprepitant
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (1)
- Side effects
- Dosage information
- During pregnancy
- Drug class: NK1 receptor antagonists
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.