FLUoxetine (Monograph)
Brand names: PROzac, PROzac Weekly, Sarafem
Drug class: Selective Serotonin-reuptake Inhibitors
- Serotonin-reuptake Inhibitors
- SSRIs
VA class: CN609
Chemical name: N-Methyl-γ-[4-(trifluoromethyl)phenoxy]benzenepropanamine hydrochloride
Molecular formula: C17H18F3NO•HCl
CAS number: 56296-78-7
Warning
- Suicidality
-
Antidepressants increased risk of suicidal thinking and behavior (suicidality) compared with placebo in children, adolescents, and young adults (18–24 years of age) with major depressive disorder and other psychiatric disorders; balance this risk with clinical need. Fluoxetine is not approved for use in pediatric patients except for patients with major depressive disorder or obsessive-compulsive disorder. (See Pediatric Use under Cautions.)
-
In pooled data analyses, risk of suicidality was not increased in adults >24 years of age and was reduced in adults ≥65 years of age with antidepressant therapy compared with placebo.
-
Depression and certain other psychiatric disorders are themselves associated with an increased risk of suicide.
-
Appropriately monitor and closely observe all patients who are started on fluoxetine therapy for clinical worsening, suicidality, or unusual changes in behavior; involve family members and/or caregivers in this process. (See Worsening of Depression and Suicidality Risk under Cautions.)
Introduction
Antidepressant; selective serotonin-reuptake inhibitor (SSRI).
Uses for FLUoxetine
Major Depressive Disorder
Acute and maintenance treatment of major depressive disorder.
APA states that effectiveness of antidepressants is generally comparable between and within classes of medications, including SSRIs, SNRIs, TCAs, MAO inhibitors, and other antidepressants (e.g., bupropion, mirtazapine, trazodone). Choose antidepressant based mainly on patient preference; nature of prior response to medication; safety, tolerability, and anticipated adverse effects; concurrent psychiatric and medical conditions; and specific properties of the medication (e.g., half-life, actions on CYP isoenzymes, other drug interactions). For most patients, an SSRI, SNRI, mirtazapine, or bupropion is considered optimal. Consult APA’s Practice Guidelines for the Treatment of Patients with Major Depressive Disorder for additional information.
Obsessive-Compulsive Disorder (OCD)
Acute and maintenance treatment of OCD.
Premenstrual Dysphoric Disorder (PMDD)
Management of PMDD (previously late luteal phase dysphoric disorder).
Eating Disorders
Acute and maintenance treatment of moderate to severe bulimia nervosa (at least 3 bulimic episodes per week for 6 months).
SSRIs usually are preferred drugs in management of bulimia because of more favorable adverse effect profile.
Also has been used for management of anorexia nervosa† [off-label].
Not recommended as the sole or primary treatment of anorexia nervosa† [off-label].
Panic Disorder
Acute treatment of panic disorder with or without agoraphobia.
Bipolar Disorder
Short-term treatment of acute depressive episodes (alone† [off-label] or in combination with olanzapine) in patients with bipolar I disorder (bipolar depression).
May cause manic reactions when used as monotherapy in some patients; should not be used without mood stabilizing agents (e.g., lithium, lamotrigine).
Obesity
Has been used for the short-term treatment of exogenous obesity† [off-label].
Cataplexy
Has been used for the symptomatic management of cataplexy† [off-label] in a limited number of patients with cataplexy and associated narcolepsy.
Alcohol Dependence
Has been used in the management of alcohol dependence†.
Studies of SSRIs have generally shown modest effects on alcohol consumption.
Myoclonus
Has been used for management of intention myoclonus†, including postanoxic action myoclonus† and progressive action myoclonus† in a limited number of patients.
Premature Ejaculation
Like some other SSRIs, has been used for the treatment of premature ejaculation†.
FLUoxetine Dosage and Administration
General
-
Allow at least 2 weeks to elapse between discontinuance of an MAO inhibitor and initiation of fluoxetine, and at least 5 weeks to elapse between discontinuance of fluoxetine and initiation of an MAO inhibitor or thioridazine. (See Contraindications and also see Serotonin Syndrome or Neuroleptic Malignant Syndrome-like Reactions under Cautions.)
-
Monitor for possible worsening of depression, suicidality, or unusual changes in behavior, especially at the beginning of therapy or during periods of dosage adjustments. (See Worsening of Depression and Suicidality Risk under Cautions.)
-
Sustained therapy may be required; periodically reassess need for continued therapy.
-
Avoid abrupt discontinuance. Taper dosage gradually and monitor for withdrawal symptoms. If intolerable symptoms occur following dosage reduction or discontinuance, consider reinstituting previously prescribed dosage, then resume more gradual dosage reductions. (See Withdrawal of Therapy under Cautions.)
-
Consider cautiously tapering dosage during third trimester of pregnancy prior to delivery. (See Pregnancy under Cautions.)
Administration
Oral Administration
Administer conventional capsules, tablets, and solution orally once (in the morning) or twice daily (preferably in the morning and at noon) without regard to meals. If sedation occurs, the second dose may be administered at bedtime.
Administer delayed-release preparation once weekly without regard to meals.
Administer fixed-combination fluoxetine/olanzapine capsules (Symbyax) once daily in the evening.
Dosage
Available as fluoxetine hydrochloride; dosage is expressed in terms of fluoxetine.
Consider prolonged elimination half-life of fluoxetine and norfluoxetine (active metabolite) when titrating dosage or discontinuing therapy. Several weeks may be required before full effect of dosage alterations is realized.
Pediatric Patients
Major Depressive Disorder
Oral
Children and adolescents ≥8 years of age: Initially, 10 or 20 mg daily. If therapy is initiated at 10 mg daily, should increase dosage after 1 week to 20 mg daily.
Manufacturer states that both the initial and target dosage in lower weight children may be 10 mg daily.
An increase in dosage to 20 mg daily may be considered after several weeks in lower weight children if insufficient clinical improvement is observed.
Obsessive-Compulsive Disorder
Oral
Children and adolescents ≥7 years of age: Initially, 10 mg daily.
In adolescents and higher weight children, should increase dosage to 20 mg daily after 2 weeks; additional dosage increases may be considered after several more weeks if insufficient clinical improvement is observed.
In lower weight children, dosage increases may be considered after several weeks if insufficient clinical improvement is observed.
Usual dosages: 20–60 mg daily for adolescents and higher weight children or 20–30 mg daily for lower weight children.
Optimal duration not established. If used for prolonged period, use minimum effective dosage and periodically reassess need for continued therapy.
Adults
Major Depressive Disorder
Oral
As conventional capsules, tablets, or solution: Initially, 20 mg daily (in the morning). May initiate with lower dosage (e.g., 5 mg daily, 20 mg every 2–3 days). If no improvement is apparent after several weeks of therapy with 20 mg daily, an increase in dosage may be considered.
Usual dosage: 10–80 mg daily.
Delayed-release capsules: 90 mg once weekly, beginning 7 days after the last 20 mg daily dose as conventional capsules, tablets, or solution.
If a satisfactory response is not maintained, consider reestablishing daily dosage regimen with conventional capsules, tablets, or solution.
Optimum duration not established; may require several months of therapy or longer.
Obsessive-Compulsive Disorder
Oral
Initially, 20 mg daily (in the morning). If no improvement is apparent after several weeks, dosage may be increased.
Usual dosage: 20–60 mg daily; dosages ≤80 mg daily were well tolerated in clinical studies.
Optimal duration not established. If used for prolonged period, use minimum effective dosage and periodically reassess need for continued therapy.
Premenstrual Dysphoric Disorder
Oral
20 mg once daily given continuously throughout the menstrual cycle or intermittently (i.e., only during the luteal phase, starting 14 days prior to the anticipated onset of menstruation and continuing through the first full day of menses).
If the intermittent dosing regimen is used, it should be repeated with each new menstrual cycle.
Eating Disorders
Bulimia Nervosa
Oral60 mg daily (in the morning); dosage may be decreased as necessary to minimize adverse effects. Alternatively, dosage may be titrated up to recommended initial dosage over several days.
Efficacy was maintained for periods of ≤12 months following 2 months of acute treatment in patients receiving 60 mg daily as conventional fluoxetine capsules. Most clinicians recommend continuing antidepressant therapy, including fluoxetine, for at least 6–12 months before attempting to discontinue therapy. If used for extended periods, periodically reassess need for continued therapy.
Anorexia Nervosa†
Oral40 mg daily in weight-restored patients has been used.
Panic Disorder
Oral
Initially, 10 mg daily. Increase dosage after 1 week to 20 mg daily. 10–60 mg is effective; 20 mg daily most frequently used. Dosages >60 mg daily not systematically evaluated.
Optimal duration not established. If used for prolonged period, periodically reassess need for continued therapy.
Bipolar Disorder
Monotherapy for Acute Depressive Episodes†
Oral20–60 mg daily in conjunction with a mood-stabilizing agent (e.g., lithium, lamotrigine).
Combination Therapy for Acute Depressive Episodes
OralFluoxetine/olanzapine (Symbyax): Initially, fluoxetine 25 mg and olanzapine 6 mg (Symbyax 6/25) once daily in the evening.
Fluoxetine 25 mg and olanzapine 3–6 mg (Symbyax 3/25 or Symbyax 6/25) once daily in the evening as initial and maintenance therapy in patients with a predisposition to hypotensive reactions, patients with hepatic impairment, those with a combination of factors that may slow metabolism of the drugs(s) (e.g., female gender, geriatric age, nonsmoking status), or those who may be pharmacodynamically sensitive to olanzapine; when indicated, escalate dosage with caution.
In other patients, increase dosages of fluoxetine/olanzapine according to patient response and tolerance as indicated. In clinical trials, antidepressive efficacy was demonstrated at olanzapine dosages ranging from 6–12 mg daily and fluoxetine dosages ranging from 25–50 mg daily. Dosages >18 mg of olanzapine and 75 mg of fluoxetine not evaluated in clinical studies.
When used with olanzapine as the single-ingredient components, administer the drugs once daily in the evening, usually initiating therapy with 5 mg of olanzapine and 20 mg of fluoxetine. May adjust dosage within the dosage ranges of 20–50 mg for fluoxetine and 5–12.5 mg for olanzapine. Use an initial dosage of 2.5–5 mg of olanzapine with fluoxetine 20 mg in patients with a predisposition to hypotensive reactions, patients with hepatic impairment, those with a combination of factors that may slow metabolism of the drugs(s) (e.g., female gender, geriatric age, nonsmoking status), or those patients who may be pharmacodynamically sensitive to olanzapine; when indicated, escalate dosage increases with caution.
Although the manufacturer states that long-term efficacy (>8 weeks) not established, patients have received the fixed combination ≤24 weeks in clinical trials. If used for >8 weeks, periodically reassess need for continued therapy.
Cataplexy†
Oral
20 mg once or twice daily has been used in conjunction with CNS stimulant therapy (e.g., dextroamphetamine, methylphenidate).
Alcohol Dependence†
Oral
60 mg daily has been used.
Higher than average antidepressant SSRI dosage apparently is required for reduced alcohol intake; fluoxetine 40 mg daily is comparable to placebo in efficacy.
Prescribing Limits
Adults
Oral
Conventional capsules, tablets, or solution: Maximum 80 mg daily.
Special Populations
Hepatic Impairment
Reduce dosage and/or frequency; some clinicians recommend a 50% reduction in initial dosage for patients with well-compensated cirrhosis.
Carefully individualize dosage in substantial hepatic impairment; adjust based on tolerance and therapeutic response.
Renal Impairment
Reduction in dosage and/or frequency not routinely necessary. Supplemental doses after hemodialysis not necessary.
Geriatric Patients
Consider reducing dosage and/or frequency.
Cautions for FLUoxetine
Contraindications
-
Concurrent or recent (i.e., within 2 weeks) therapy with an MAO inhibitor. MAO inhibitors are contraindicated within 5 weeks after discontinuance of fluoxetine. (See Serotonin Syndrome or Neuroleptic Malignant Syndrome-like Reactions under Cautions and also see Interactions.)
-
Concurrent pimozide therapy.
-
Concurrent thioridazine therapy. Thioridazine is contraindicated within 5 weeks after discontinuance of fluoxetine.
Warnings/Precautions
Warnings
Worsening of Depression and Suicidality Risk
Possible worsening of depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior in both adult and pediatric patients with major depressive disorder, whether or not they are taking antidepressants; may persist until clinically important remission occurs. However, suicide is a known risk of depression and certain other psychiatric disorders, and these disorders themselves are the strongest predictors of suicide.
Appropriately monitor and closely observe patients receiving fluoxetine for any reason, particularly during initiation of therapy (i.e., the first few months) and during periods of dosage adjustments. (See Boxed Warning and also see Pediatric Use under Cautions.)
Anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia, hypomania, and/or mania may be precursors to emerging suicidality. Consider changing or discontinuing therapy in patients whose depression is persistently worse or in those with emerging suicidality or symptoms that might be precursors to worsening depression or suicidality, particularly if severe, abrupt in onset, or not part of patient’s presenting symptoms. If decision is made to discontinue therapy, taper fluoxetine dosage as rapidly as is feasible but consider risks of abrupt discontinuance. (See General under Dosage and Administration.)
Prescribe in smallest quantity consistent with good patient management to reduce risk of overdosage.
Observe these precautions for patients with psychiatric (e.g., major depressive disorder, OCD) or nonpsychiatric disorders.
Sensitivity Reactions
Allergic Reactions and Rash
Possible anaphylactoid reactions (e.g., bronchospasm, angioedema, laryngospasm, and/or urticaria).
Rash and/or urticaria, sometimes associated with systemic manifestations (e.g., fever, leukocytosis, arthralgia, edema, carpal tunnel syndrome, respiratory distress, lymphadenopathy, proteinuria, mild elevation in serum aminotransferase concentrations, vasculitis, lupus-like syndrome) reported; systemic manifestations may be serious.
If rash or other possibly allergic manifestations for which an alternative etiology cannot be identified occur, discontinue therapy.
Other Warnings and Precautions
Serotonin Syndrome or Neuroleptic Malignant Syndrome-like Reactions
Potentially life-threatening serotonin syndrome or neuroleptic malignant syndrome (NMS)-like reactions reported with SSRIs and SNRIs alone, including fluoxetine, but particularly with concurrent administration of other serotonergic drugs (e.g., 5-HT1 receptor agonists [triptans]), drugs that impair serotonin metabolism (e.g., MAO inhibitors), or antipsychotics or other dopamine antagonists. (See Contraindications under Cautions and also see Interactions.)
Symptoms of serotonin syndrome may include mental status changes (e.g., agitation, hallucinations, coma), autonomic instability (e.g., tachycardia, labile BP, hyperthermia), neuromuscular aberrations (e.g., hyperreflexia, incoordination), and/or GI symptoms (e.g., nausea, vomiting, diarrhea).
Severe serotonin syndrome may resemble NMS, which is characterized by hyperthermia, muscle rigidity, autonomic instability with possible rapid fluctuations in vital signs, and mental status changes.
Monitor patients receiving fluoxetine for the development of serotonin syndrome or NMS-like signs and symptoms. If such signs and symptoms occur, immediately discontinue treatment with fluoxetine and any concurrently administered serotonergic or antidopaminergic agents, including antipsychotic agents, and initiate supportive and symptomatic treatment.
Activation of Mania or Hypomania
Possible hypomania, mania, and manic reaction. May be more likely in patients with bipolar disorder.
Bipolar Disorder
May unmask bipolar disorder. (See Activation of Mania or Hypomania under Cautions.)
Screen for risk of bipolar disorder by obtaining detailed psychiatric history (e.g., family history of suicide, bipolar disorder, depression) prior to initiating therapy.
Seizures
Possible seizures; use with caution in patients with a history of seizures.
Altered Appetite and Weight
Possible anorexia and substantial weight loss, which may be undesirable in underweight or bulimic patients. Monitor weight change during fluoxetine therapy. (See Pediatric Use under Cautions.)
Abnormal Bleeding
Possible increased risk of bleeding with SSRIs, including fluoxetine, and SNRIs; events ranged from ecchymoses, hematomas, epistaxis, and petechiae to life-threatening hemorrhages. Concomitant use of aspirin, NSAIAs, warfarin, or other anticoagulants may increase risk. (See Drugs Affecting Hemostasis and Specific Drugs under Interactions.)
Hyponatremia or SIADH
Treatment with SSRIs, including fluoxetine, and SNRIs may result in hyponatremia; in many cases, SIADH is apparent cause. Increased risk in patients who are volume depleted, elderly, or taking diuretics. Consider drug discontinuance and initiate appropriate medical intervention in patients with symptomatic hyponatremia.
Anxiety and Insomnia
Possible dose-related nervousness, anxiety, and insomnia.
Concomitant Illnesses
Limited experience; use with caution in patients with concomitant illnesses affecting metabolism or hemodynamic response.
Safety in patients with recent history of MI or those with unstable heart disease not established.
May alter glycemic control in patients with diabetes mellitus. Hypoglycemia has occurred during fluoxetine therapy and hyperglycemia has developed following discontinuance of drug. Adjust insulin and/or oral antidiabetic agent dosage as necessary when initiating or discontinuing fluoxetine therapy.
Mydriasis reported; use with caution in patients with elevated IOP or those at risk of acute narrow-angle glaucoma.
Cognitive/Motor Impairment
Potential impairment of judgment, thinking, and motor skills. (See Advice to Patients.)
Long Elimination Half-Life
Because of the long elimination half-lives of fluoxetine and its major active metabolite, norfluoxetine, changes in dosage will take several weeks to be fully reflected in plasma concentrations, which affects dosage titration and withdrawal from treatment. Consider these potential consequences when drug discontinuance is required or when prescribing concurrent drugs that may interact with fluoxetine and norfluoxetine following fluoxetine discontinuance.
Withdrawal of Therapy
Withdrawal effects (e.g., dysphoric mood, irritability, agitation, dizziness, sensory disturbances [e.g., paresthesias, such as electric shock sensations], anxiety, confusion, headache, lethargy, emotional lability, insomnia, hypomania) reported following discontinuance of serotonergic antidepressants, particularly when discontinuance was abrupt. Events generally self-limiting, but serious cases reported.
Taper dosage gradually; monitor patients for withdrawal symptoms when discontinuing therapy. If intolerable symptoms occur following dosage reduction or discontinuance, consider reinstituting previously prescribed dosage then resume more gradual dosage reductions.
Use of Fixed Combinations
When fluoxetine is used in fixed combination with olanzapine, consider cautions, precautions, contraindications, and interactions associated with each drug.
Electroconvulsive Therapy (ECT)
Effects of concomitant use with ECT not systematically evaluated. Prolonged seizures reported rarely.
Specific Populations
Pregnancy
Category C.
Possible complications, sometimes severe and requiring prolonged hospitalization, respiratory support, enteral nutrition, and other forms of supportive care, reported in neonates exposed to fluoxetine, other SSRIs, or SNRIs late in the third trimester; may arise immediately upon delivery.
Conflicting findings from available studies evaluating possible risk of persistent pulmonary hypertension of the newborn (PPHN) following in utero exposure to SSRIs; currently unclear whether SSRI use during pregnancy can cause PPHN.
Consult joint APA and ACOG guidelines (at [Web]) for additional information on management of depression in women prior to conception and during pregnancy, including treatment algorithms.
Carefully consider potential risks and benefits of treatment when used during third trimester of pregnancy. Consider cautiously tapering dosage during third trimester prior to delivery.
Lactation
Distributed into milk; use not recommended.
Pediatric Use
Safety and efficacy of fluoxetine not established in children <8 years of age for major depressive disorder and in children <7 years of age for OCD.
Safety and efficacy of fluoxetine in fixed combination with olanzapine not established in pediatric patients <18 years of age.
Decreased appetite and weight loss observed with the use of SSRIs, including fluoxetine; monitor weight and growth regularly in children and adolescents treated with fluoxetine. (See Altered Appetite and Weight under Cautions.)
FDA warns that a greater risk of suicidal thinking or behavior (suicidality) occurred during first few months of antidepressant treatment compared with placebo in children and adolescents with major depressive disorder, OCD, or other psychiatric disorders based on pooled analyses of 24 short-term, placebo-controlled trials of 9 antidepressant drugs (SSRIs and others). However, a more recent meta-analysis of 27 placebo-controlled trials of 9 antidepressants (SSRIs, including fluoxetine, and others) in patients <19 years of age with major depressive disorder, OCD, or non-OCD anxiety disorders suggests that the benefits of antidepressant therapy in treating these conditions may outweigh the risks of suicidal behavior or suicidal ideation. No suicides occurred in these pediatric trials.
Carefully consider these findings when assessing potential benefits and risks of fluoxetine in a child or adolescent for any clinical use. (See Boxed Warning and also see Worsening of Depression and Suicidality Risk under Cautions.)
Geriatric Use
No substantial differences in safety and efficacy relative to younger adults. However, increased sensitivity cannot be ruled out.
SNRIs and SSRIs, including fluoxetine, have been associated with clinically important hyponatremia in geriatric patients, who may be at greater risk for this adverse effect. (See Hyponatremia or SIADH under Cautions.)
In pooled data analyses, a reduced risk of suicidality was observed in adults ≥65 years of age with antidepressant therapy compared with placebo. (See Boxed Warning and also see Worsening of Depression and Suicidality Risk under Cautions.)
Hepatic Impairment
Decreased clearance with cirrhosis; use with caution and at reduced dosage and/or frequency. (See Hepatic Impairment under Dosage and Administration.)
Common Adverse Effects
Anxiety, nervousness, insomnia, somnolence, asthenia, tremor, anorexia, nausea, dyspepsia, diarrhea, vasodilation, dry mouth, decreased libido, abnormal ejaculation, impotence, rash, sweating, abnormal dreams, flu syndrome, pharyngitis, sinusitis, yawning.
Drug Interactions
Extensively metabolized; inhibits CYP2D6 and to much less extent CYP3A4.
When used in fixed combination with olanzapine, consider interactions associated with each drug in the fixed combination.
Drugs Associated with Serotonin Syndrome
Potential pharmacologic interaction (potentially serious, sometimes fatal serotonin syndrome or NMS-like reactions) with serotonergic agents. Avoid such use, or use with caution. (See Contraindications and see Serotonin Syndrome or Neuroleptic Malignant Syndrome-like Reactions under Cautions.)If serotonin syndrome or NMS occurs, immediately discontinue fluoxetine and any concurrently administered serotonergic agents or antidopaminergic agents and initiate supportive and symptomatic treatment.
Drugs Affecting Hepatic Microsomal Enzymes
Inhibitors of CYP2D6 or CYP3A4: clinically important pharmacokinetic interaction unlikely.
Drugs Metabolized by Hepatic Microsomal Enzymes
Substrates of CYP2D6: potential pharmacokinetic interaction. Fluoxetine inhibits CYP2D6 activity; may increase plasma concentrations of drugs metabolized by CYP2D6.
Substrates of CYP3A4: clinically important pharmacokinetic interaction unlikely.
Drugs Affecting Hemostasis
Potential pharmacologic interaction (increased risk of bleeding) with concomitant use of drugs that affect hemostasis; use with caution. (See Abnormal Bleeding under Cautions.)
Protein-bound Drugs
Fluoxetine displaces and is displaced by protein-bound drugs. Monitor for possible adverse effects if used concomitantly with other protein-bound drugs.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Alcohol |
Does not potentiate cognitive and motor effects of alcohol; possible serotonergically-mediated pharmacodynamic interaction in CNS |
Concomitant use not recommended |
|
Amphetamine |
Decreased amphetamine metabolism; potential serotonin syndrome |
|
|
Anticoagulants (e.g., warfarin) |
Altered anticoagulant effects, including increased bleeding |
Carefully monitor patients receiving warfarin when fluoxetine is initiated or discontinued |
|
Antidiabetic agents |
May alter blood glucose concentrations in patients with diabetes mellitus |
Adjust insulin and/or antidiabetic dosages as needed when fluoxetine therapy is initiated or discontinued |
|
β-Adrenergic blocking agents (e.g., metoprolol, propranolol) |
Increased plasma concentrations of β-adrenergic blocking agents metabolized by CYP2D6; possible cardiac toxicity |
Renally eliminated β-adrenergic blocking agents (e.g., atenolol) may be a safer choice |
|
Antidepressants, other SSRIs (e.g., citalopram, escitalopram, fluvoxamine, paroxetine, sertraline) or SNRIs (e.g., desvenlafaxine, duloxetine, milnacipran, venlafaxine) |
Potentially serious, sometimes fatal serotonin syndrome or NMS-like reactions |
Concomitant use not recommended |
|
Antidepressants, tricyclic (TCAs) |
Increased plasma TCA concentrations |
Observe patient closely for adverse effects. Plasma TCA concentrations may need to be monitored and TCA dosages reduced when fluoxetine is administered concurrently or has been recently discontinued |
|
Antipsychotic agents (e.g., clozapine, haloperidol, olanzapine, pimozide, risperidone, thioridazine) |
Potentially serious, sometimes fatal serotonin syndrome or NMS-like reactions Clozapine: Increased plasma clozapine concentrations Haloperidol: Increased plasma haloperidol concentrations; severe extrapyramidal symptoms have occurred Olanzapine: Increase in peak plasma olanzapine concentrations and decreased olanzapine clearance; unlikely to be clinically important Pimozide: Possible increased risk of QTc interval prolongation. Bradycardia, altered mental status (e.g., stupor, inability to think clearly), and/or hypersalivation reported rarely with concomitant use Risperidone: Possible increased risperidone plasma concentrations; tardive dyskinesia reported Thioridazine: Increased plasma thioridazine concentrations; serious ventricular arrhythmias and sudden death are possible |
If serotonin syndrome or NMS occurs, immediately discontinue fluoxetine and any concurrently administered antidopaminergic or serotonergic agents; initiate supportive and symptomatic treatment Clozapine: Use with caution, monitor closely, and consider decreasing clozapine dosage Olanzapine: No dosage adjustment necessary Pimozide: Concomitant use contraindicated Thioridazine: Concomitant use is contraindicated; an interval of >5 weeks should elapse between discontinuance of fluoxetine and initiation of thioridazine |
|
Benzodiazepines |
Increased plasma concentrations of diazepam and alprazolam |
Clinically important interaction possible in geriatric or other susceptible patients |
|
Buspirone |
Possible serotonin syndrome |
|
|
Carbamazepine |
Increased plasma concentrations of carbamazepine and its active metabolite; carbamazepine toxicity has been reported |
Monitor patient and plasma carbamazepine concentrations closely when fluoxetine therapy is initiated or discontinued and adjust carbamazepine dosage accordingly |
|
Diuretics |
Increased risk of hyponatremia |
|
|
Dopamine antagonists |
Potentially serious, sometimes fatal serotonin syndrome or NMS-like reactions |
If serotonin syndrome or NMS occurs, immediately discontinue fluoxetine and any concurrently administered antidopaminergic or serotonergic agents; initiate supportive and symptomatic treatment |
|
5-HT1 receptor agonists (triptans) |
Potentially serious, sometimes fatal serotonin syndrome or NMS-like reactions |
Observe carefully if used concomitantly, particularly during treatment initiation, dosage increases, or when another serotonergic agent is initiated If serotonin syndrome or NMS occurs, immediately discontinue fluoxetine and any concurrently administered antidopaminergic or serotonergic agents; initiate supportive and symptomatic treatment |
|
Isoniazid |
Potential for serotonin syndrome Isoniazid has some MAO-inhibiting activity |
|
|
Linezolid |
Potentially life-threatening serotonin syndrome or NMS-like reactions |
Do not use concurrently; consider availability of alternative anti-infectives and weigh benefit of linezolid against risk of serotonin syndrome If emergency use of linezolid is considered necessary, immediately discontinue fluoxetine; monitor closely for symptoms of CNS toxicity for 5 weeks or until 24 hours after the last linezolid dose, whichever comes first If nonemergency use of linezolid is planned, withhold fluoxetine for at least 5 weeks prior to initiating linezolid; fluoxetine may be resumed 24 hours after last linezolid dose Do not initiate fluoxetine in patients receiving linezolid; when necessary, initiate 24 hours after last linezolid dose |
|
Lithium |
Increased or decreased serum lithium concentrations Lithium toxicity and/or serotonin syndrome has been reported |
Use with caution and monitor serum lithium concentrations closely |
|
MAO inhibitors |
Potentially serious, sometimes fatal serotonin syndrome or NMS-like reactions |
Concomitant use is contraindicated Allow at least 5 weeks to elapse between discontinuance of fluoxetine therapy and initiation of MAO inhibitor therapy and at least 2 weeks between discontinuance of MAO inhibitor therapy and initiation of fluoxetine |
|
NSAIAs (e.g., aspirin) |
Increased risk of bleeding |
Use with caution |
|
Pentazocine |
Adverse effects resembling serotonin syndrome |
|
|
Phenytoin |
Increased plasma phenytoin concentrations and phenytoin toxicity |
|
|
Selegiline |
Possible serotonin syndrome |
Avoid concomitant use Allow at least 5 weeks to elapse between discontinuance of fluoxetine therapy and initiation of selegiline and at least 2 weeks between discontinuance of selegiline and initiation of fluoxetine |
|
Sibutramine (no longer commercially available in US) |
Possible serotonin syndrome |
Use with caution |
|
Stimulants (e.g., methylphenidate) |
Potential serotonin syndrome |
Do not exceed maximum fluoxetine dosage of 20 mg daily |
|
Tramadol |
Potentially serious, sometimes fatal serotonin syndrome or NMS-like reactions |
Use with caution If serotonin syndrome or NMS occurs, immediately discontinue fluoxetine and any concurrently administered antidopaminergic or serotonergic agents; initiate supportive and symptomatic treatment |
|
Trazodone |
Increased plasma trazodone concentrations and adverse effects |
Observe patient closely for adverse effects and decrease trazodone dosage as necessary |
|
Tryptophan and other serotonin precursors |
Potentially serious, sometimes fatal serotonin syndrome or NMS-like reactions |
Concomitant use not recommended |
|
Warfarin |
Possible increased risk of bleeding |
Carefully monitor patients receiving warfarin during initiation and discontinuance of fluoxetine therapy |
FLUoxetine Pharmacokinetics
Absorption
Bioavailability
Oral bioavailability in humans not fully elucidated, but at least 60–80% of an oral dose appears to be absorbed.
Commercially available conventional and delayed-release capsules, tablets, and oral solution are bioequivalent.
Onset
Antidepressant effect usually occurs within 1–4 weeks.
Maximal therapeutic effect in OCD may take 5 weeks or longer.
Therapeutic effect in PMDD usually occurs in 2–4 weeks.
Food
Food does not appear to affect systemic bioavailability, although it may delay absorption by 1–2 hours.
Special Populations
In patients receiving hemodialysis, chronic administration produced steady-state plasma fluoxetine and norfluoxetine (active metabolite) concentrations comparable with those observed in patients with normal renal function.
Distribution
Extent
Crosses the blood-brain barrier in humans.
Crosses the placenta in animals.
Distributed into milk in humans.
Plasma Protein Binding
Approximately 95%.
Elimination
Metabolism
Extensively metabolized in the liver to norfluoxetine and a number of other unidentified metabolites.
Elimination Route
Principally by hepatic metabolism to inactive metabolites excreted by the kidney.
Half-life
Elimination half-life of approximately 2–3 days after a single dose and 4–6 days after chronic administration of fluoxetine.
Elimination half-life of norfluoxetine is approximately 4–16 days after acute and chronic administration.
Special Populations
In patients with chronic liver disease (e.g., cirrhosis), plasma clearances of fluoxetine and norfluoxetine reportedly are decreased and elimination half-lives are increased compared with those of healthy individuals.
In patients with renal impairment, elimination half-lives of fluoxetine and norfluoxetine not substantially altered.
Stability
Storage
Oral
Capsules, Conventional and Delayed-release
15–30°C; protect from light.
Solution
20–25°C; protect from light.
Tablets
20–25°C; protect from light.
Actions
-
Mechanism of action as an antidepressant or as an anti-obsessive agent is unclear but presumed to be linked to potentiation of serotonergic activity in the CNS resulting from its inhibition of CNS neuronal reuptake of serotonin (5-HT).
-
Mechanism of action in PMDD not mediated by the drug’s antidepressant or anti-obsessive effects.
-
Potent and highly selective reuptake inhibitor of serotonin. Increases synaptic concentrations of serotonin in the CNS but has little or no effect on other neurotransmitters.
-
No important anticholinergic, α1-adrenergic blocking, or antihistaminic activity at usual therapeutic dosages.
-
Generally less sedating than most other antidepressants (e.g., TCAs, MAO inhibitors).
Advice to Patients
-
Importance of providing copy of written patient information (medication guide) each time fluoxetine is dispensed. Importance of advising patients to read the patient information before taking fluoxetine and each time the prescription is filled.
-
Risk of suicidality; importance of patients, family, and caregivers being alert to and immediately reporting emergence of suicidality, worsening depression, or unusual changes in behavior, especially during the first few months of therapy or during periods of dosage adjustment. (See Worsening of Depression and Suicidality Risk under Cautions.)
-
Importance of instructing patients not to take fluoxetine with an MAO inhibitor or within 14 days of stopping the MAO inhibitor, and not to take an MAO inhibitor within 5 weeks of stopping fluoxetine therapy.
-
Importance of informing patients of potential risk of serotonin syndrome and neuroleptic malignant syndrome (NMS)-like reactions, particularly with concurrent use of fluoxetine and 5-HT1 receptor agonists (also called triptans), tramadol, tryptophan, other serotonergic agents, or antipsychotic agents. Importance of immediately contacting clinician if signs and symptoms of these syndromes develop (e.g., restlessness, hallucinations, loss of coordination, fast heart beat, increased body temperature, muscle stiffness, increased BP, diarrhea, coma, nausea, vomiting, confusion).
-
Risk of allergic reactions and rash. Importance of advising patients to notify their clinician if they develop a rash or hives. Importance of also advising patients of the signs and symptoms associated with severe allergic reactions (e.g., swelling of the face, eyes, mouth; difficulty breathing) and to seek immediate medical attention if they experience these symptoms.
-
Importance of informing patients that if they receive diuretics, or are otherwise volume-depleted, or are elderly, that they may be at greater risk of developing hyponatremia during fluoxetine therapy.
-
Importance of understanding that full effects of the drug may not be apparent for more than 4–5 weeks following initiation of therapy.
-
Importance of patients being aware that withdrawal effects may occur when stopping fluoxetine, especially with abrupt discontinuance of the drug.
-
Risk of cognitive and motor impairment; importance of avoiding certain activities (e.g., operating machinery, driving a motor vehicle) until effects on the individual are known.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription (e.g., Symbyax, Sarafem) and OTC drugs or herbal supplements and alcohol-containing beverages or products, as well as any concomitant illnesses (e.g., bipolar disorder) or personal or family history of suicidality or bipolar disorder. Importance of also informing clinicians if patients plan to discontinue any medications while receiving fluoxetine therapy.
-
Importance of advising patients about the risk of bleeding or bruising associated with concomitant use of fluoxetine with aspirin or other NSAIAs, warfarin, or other drugs that affect coagulation. Importance of advising patients to inform their clinician if they experience any increased or unusual bruising or bleeding while receiving fluoxetine.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
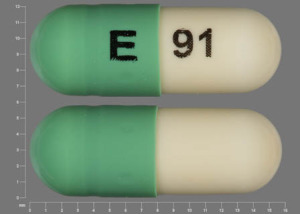
Capsules |
10 mg (of fluoxetine)* |
FLUoxetine Hydrochloride Capsules |
|
|
PROzac Pulvules |
Dista |
|||
|
Sarafem Pulvules |
Lilly |
|||
|
20 mg (of fluoxetine)* |
FLUoxetine Hydrochloride Capsules |
|||
|
PROzac Pulvules |
Dista |
|||
|
Sarafem Pulvules |
Lilly |
|||
|
40 mg (of fluoxetine)* |
FLUoxetine Hydrochloride Capsules |
|||
|
PROzac Pulvules |
Dista |
|||
|
Capsules, delayed-release (containing enteric-coated pellets) |
90 mg (of fluoxetine) |
PROzac Weekly |
Dista |
|
|
Solution |
20 mg (of fluoxetine) per 5 mL* |
Fluoxetine Hydrochloride Oral Solution |
||
|
Tablets |
10 mg (of fluoxetine)* |
FLUoxetine Hydrochloride Tablets |
||
|
Sarafem |
Warner Chilcott |
|||
|
15 mg (of fluoxetine)* |
Sarafem |
Warner Chilcott |
||
|
20 mg (of fluoxetine)* |
FLUoxetine Hydrochloride Tablets |
|||
|
Sarafem |
Warner Chilcott |
|||
|
60 mg (of fluoxetine)* |
FLUoxetine Hydrochloride Tablets |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules |
25 mg (of fluoxetine) with Olanzapine 3 mg |
Symbyax (combination) |
Lilly |
|
25 mg (of fluoxetine) with Olanzapine 6 mg |
Symbyax |
Lilly |
||
|
25 mg (of fluoxetine) with Olanzapine 12 mg |
Symbyax |
Lilly |
||
|
50 mg (of fluoxetine) with Olanzapine 6 mg |
Symbyax |
Lilly |
||
|
50 mg (of fluoxetine) with Olanzapine 12 mg |
Symbyax |
Lilly |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions February 15, 2013. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Frequently asked questions
- SSRIs vs SNRIs - What's the difference between them?
- What drugs can cause serotonin syndrome?
- Prozac vs Zoloft: Understanding the Differences Between Two Popular Antidepressants
- Is Prozac (fluoxetine) safe for dogs?
- What are some common side effects of antidepressants?
- Taking fluoxetine, what can I use for a bad cough from cold or strep throat?
More about fluoxetine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (2,254)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: selective serotonin reuptake inhibitors
- Breastfeeding
Patient resources
Professional resources
- Fluoxetine Capsules prescribing information
- Fluoxetine Delayed Release Capsules (FDA)
- Fluoxetine Solution (FDA)
Other brands
Prozac, Prozac Weekly, Sarafem