Cannabidiol
Scientific Name(s): Cannabis sativa
Common Name(s): Cannabidiol, Cannabidiol oil, CBD, CBD oil, CBD oil tincture, CBD-dominant hemp oil, Hemp oil
Medically reviewed by Drugs.com. Last updated on Jul 14, 2025.
Clinical Overview
Use
Note: This monograph specifically discusses the nonpharmaceutical, natural preparations of the cannabinoid called cannabidiol (CBD), a chemical constituent of the cannabis plant (Cannabis sativa L.). According to US federal law, natural CBD products must meet the definition of hemp and contain little to no tetrahydrocannabinol (THC) (less than 0.3% by dry weight). For more information regarding clinical uses, interactions, adverse reactions, and toxicology associated with the C. sativa plant that includes CBD combined with THC, see the Cannabis monograph.
Robust data are lacking to support the effective use of natural CBD for any medical condition.
Dosing
Systematic reviews of randomized controlled trials report a variety of CBD dosages and treatment durations.
Contraindications
Contraindications have not been identified.
Pregnancy/Lactation
Avoid use. Information regarding safety and efficacy in pregnancy and lactation is lacking.
Interactions
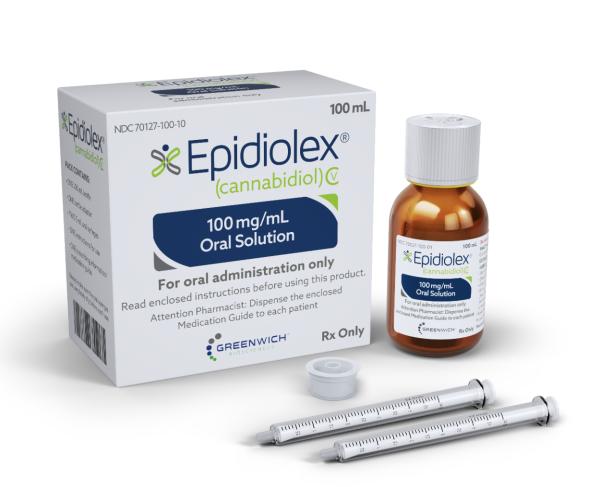
Tacrolimus toxicity was reported with concomitant use of the prescription CBD product (Epidiolex). CBD and its active metabolite demonstrate activity at varying degrees on numerous P450 isoforms, including CYP3A4 and 2C19, as well as at P-glycoprotein and glucuronidation pathways.
Adverse Reactions
Changes in alertness, GI distress, and mood changes are most commonly reported. Information regarding adverse effects specifically attributed to CBD is limited and is derived predominantly from the prescribing information for Epidiolex, a pure CBD oral solution approved by the US Food and Drug Administration (FDA). Somnolence, sedation, fatigue, decreased appetite, weight loss, insomnia, sleep disturbance, pneumonia, gait disturbance, and transaminase elevation occurred with prescription CBD at more than twice the incidence of placebo. Seizure aggravation, leading to treatment withdrawal, has also been reported.
Toxicology
No data.
Scientific Family
- Cannabaceae
Source
Cannabidiol, or CBD, is a non-psychoactive cannabinoid of the cannabis plant C. sativa L. Species, subspecies, and/or variants ascribed to the Cannabis genus include C. sativa, Cannabis indica, and Cannabis ruderalis; however, disagreement exists regarding distinct classification of these.Gloss 2015 Variants of C. sativa, such as Charlotte's Web cannabis, cultivated specifically to be low in THC and high in CBD content have been described.Jikomes 2018
History
The chemical structure of CBD and other major phytocannabinoids was elucidated in the 1960s, with the first clinical use of CBD in epilepsy reported in the literature in 1974.Friedman 2017, Russo 2017 In 2018, a pure CBD product (Epidiolex) for prescription use only was approved by the US FDA for treatment of rare seizure disorders in young children.
In the United States, the Agricultural Improvement Act of 2018 (also known as the Farm Bill) differentiated between non-psychoactive and psychoactive cannabis products. The Farm Bill created the definition for "hemp" as cannabis (C. sativa L.) and cannabis derivatives containing little to none of the psychoactive cannabinoid tetrahydrocannabinol, or THC (less than 0.3% by dry weight). Marketing of hemp and its derivatives, which includes CBD-dominant hemp oil, is therefore no longer illegal under US federal law, but these products are still under FDA regulatory authority and subject to requirements under the Food Drug and Cosmetic Act. Products containing CBD cannot currently be sold as a food or dietary supplement in the United States and fall under the category of a cosmetic.FDA 2018, FDA 2020
Cannabis and derivatives with higher concentrations of the psychoactive constituent THC remain Schedule I controlled substances.FDA 2018, FDA 2020 Federal and state laws in the United States, however, are not yet synchronized with respect to the legal medical and/or recreational use of Cannabis or Cannabis-derived products, including CBD, and many products are being marketed illegally with unproven medical claims.FDA 2020, Mead 2017 Adulterated, contaminated, and mislabeled CBD products are also being found in the market due to a lack of standardized production processes, with some analyses reporting only 30% of products with accurately labeled contents.FDA 2020, Herbst 2020
Chemistry
CBD is a chemical constituent of C. sativa L. Cannabidiol (2-[(1R,6R)-3-methyl-6-prop-1-en-2-ylcyclohex-2-en-1-yl]-5-pentylbenzene-1,3-diol) is distinct from the more than 100 other cannabinoid compounds, such as cannabinol, cannabigerol, and cannabivarin, found in lower concentrations in the plant.Morales 2017, NCBI 2018
Uses and Pharmacology
The uses described in the following sections focus on CBD specifically with THC content less than 0.3%. See also the Cannabis monograph for further information regarding potential uses of CBD in combination with THC at higher concentrations.
CBD has low affinity for CB receptors. It acts as an antagonist or partial antagonist at endogenous cannabinoid receptors (both CB1 and CB2 receptor types as well as other G-protein-coupled receptors [GPCRs]) by inhibiting full binding of direct ligands, and may act primarily at allosteric receptor sites. CBD acts as a modulator of receptor activation, influencing the endogenous cannabinoid system by inhibiting intrinsic anandamide-mediated neurotransmission and regulating other cerebral neurotransmitters and receptors. Serotonergic, vanilloid, alpha-1-adrenergic, mu opioid, noradrenaline, dopamine, GABA, anandamide, several ion channels, glycine, and PPAR-gamma are other recognized molecular targets of CBD.Brown 2019, Gaston 2017, Grant 2018, Martinez-Pinilla 2017, Pertwee 2008, Tzadok 2016
The majority of the biotransformation of CBD to its primary active metabolite, 7-hydroxy-CBD (7-OH-CBD), is accomplished through the P450 CYP3A4 and 2C19 enzymes. Both CBD and 7-OH-CBD have similar effects on multiple P450 enzymes, and CBD also has inhibitory effects on certain glucuronidation (ie, UGT1A9, UGT2B7) pathways. The most abundant metabolite of CBD is the hydroxylated form (7-COOH-CBD) and although it is inactive, it is a substrate for P-glycoprotein and other transport proteins. Bioavailability of CBD is predictable with liquid formulations and produces measurable drug levels in 1 to 3 hours with a Cmax at 3 to 5 hours postingestion. Vaping leads to rapid bioavailability with the first inhalation and a Cmax within 15 to 30 minutes; however, the high temperatures (356° to 392°F; 180° to 200°C) oxidize CBD and any excipients, which increases risk of adverse effects. Edible CBD products have less predictable and erratic absorption profiles.Brown 2019 After a 100 mg dose, mean (SD) peak whole blood CBD concentrations for vaporized CBD-dominant cannabis (CBD:THC approximately 25:1), vaporized CBD and oral CBD were 181.4 (160.8), 104.6 (76.5) and 11.1 (14.7) ng/mL, respectively, over an 8-hour period in a double-blind, double-dummy, randomized, placebo-controlled, crossover study (N=18) by Johns Hopkins University. In men compared to women, mean peak levels were approximately 30%, 50%, and 100% higher for each treatment, respectively. For the vaped CBD-dominant dosing, peak THC levels were 6.2 (7.8) ng/mL. Subjective effects that were significantly more noticeable with vaporized CBD than oral CBD or placebo were pleasantness, like drug, dry mouth, and irritated throat.Spindle 2020
Chemotherapy-induced peripheral neuropathy
Clinical data
The American Society of Clinical Oncology (ASCO) guideline update for prevention and management of chemotherapy-induced peripheral neuropathy (2020) recommends that clinicians not offer cannabinoids for the prevention of chemotherapy-induced peripheral neuropathy (CIPN) in adults with cancer undergoing treatment with neurotoxic agents (Intermediate; Moderate). For patients who have completed neurotoxic chemotherapy, no recommendations could be made for use of oral cannabinoids in treatment of CIPN, outside the context of a clinical trial (Low; NA).Loprinzi 2020
CNS effects
Antinociceptive effects
Animal data
Results from experiments conducted in animals and reviews of animal data suggest anti-inflammatory and antinociceptive effects of CBD in conditions such as arthritis,Hammell 2016 chronic neuropathic pain,Lötsch 2018, Mücke 2018 and osteoarthritis pain.O'Brien 2018
Clinical data
Few studies have investigated, or are currently investigating, the effect of CBD alone on pain; most rely on CBD/THC combination preparations.Mücke 2018, NIH 2018 High-quality clinical evidence for the use of CBD in neuropathic pain is lacking,Mücke 2018 with one clinical study suggesting improvement in quality-of-life scores, including a physical discomfort measure as part of the Parkinson Disease Questionnaire (PDQ-39), in patients with Parkinson disease.Chagas 2014 Application of topical CBD (250 mg CBD per 3 fluid ounces emu oil) to focal areas of neuropathy on the lower extremities up to 4 times a day for 4 weeks was noted to significantly improve intense (P=0.009), sharp (P<0.001), and itchy (P=0.001) pain compared to placebo in randomized, double-blind, controlled study. The 29 adults enrolled had an average age of 68 years (range, 35 to 79) with symptomatic neuropathic pain secondary to diabetes (62.1%), idiopathic etiology (20.7%), and medications (10.3%). The previous use of CBD products did not appear to significantly influence outcomes. No adverse events were reported.Xu 2019
A bias towards reporting positive findings exists both within individual clinical studies, as well as within systematic reviews of CBD use for pain management.Häuser 2018, Lötsch 2018
Parkinson disease
Clinical data
Clinical trials evaluating CBD alone in the management of motor symptoms in Parkinson disease are being conducted.NIH 2018 In a small study, patients with Parkinson disease (N=21) received CBD 75 mg/day, CBD 300 mg/day, or placebo for 6 weeks. There were no significant differences concerning motor and general symptoms; however, in Parkinson disease patients without psychiatric comorbidities, significant improvement in measures related to quality of life were observed with the higher CBD dosage compared to placebo.Chagas 2014
In a case series of Parkinson disease patients with rapid eye movement (REM) sleep behavior disorder, CBD 75 mg/day and 300 mg/day for 6 weeks resulted in a reduction in the frequency of REM sleep behavior disorder–related events. Further research is needed.Chagas 2014
Schizophrenia
Clinical data
Dates are equivocal. Several phase 1 and phase 2 clinical trials have evaluated CBD as an antipsychotic intervention, with no net effects reported in some, and publication of results pending for others.Boggs 2018, NIH 2018
In one phase 2 trial, men and women 18 to 50 years of age with schizophrenia (N=42) were randomized to receive CBD or amisulpride, each starting at 200 mg/day and increased to 200 mg 4 times per day (800 mg/day) within the first week. After 4 weeks of treatment, both CBD and amisulpride treatment resulted in significant clinical improvement in psychotic symptoms, as evidenced by a reduction in Positive and Negative Syndrome Scale (PANSS) total score (P<0.001), among other measures. Compared to amisulpride, CBD was well tolerated and was associated with fewer extrapyramidal symptoms, less weight gain, and a lower incidence of sexual dysfunction.Leweke 2012 In another multicenter, randomized, controlled trial, patients with schizophrenia (N=43) received CBD 1,000 mg/day or placebo in addition to their existing antipsychotic medication. After 6 weeks, the CBD group had lower levels of positive psychotic symptoms (treatment difference in PANSS positive score, −1.4). Patients receiving CBD also showed greater improvements in cognitive performance and overall functioning, but differences between groups were not statistically significant.McGuire 2018
A study of 36 stable antipsychotic-treated patients with schizophrenia showed no improvement in PANSS or MATRICS Consensus Cognitive Battery scores with CBD 600 mg/day for 2 weeks compared to placebo.Boggs 2018
Seizures
The exact mechanism by which CBD exerts its anticonvulsant activity is unknown. In contrast to THC, CBD has very weak affinity for the CB1 and CB2 receptors, indicating its antiseizure activity is mediated by other mechanisms; various targets have been investigated to explain CBD's anticonvulsant properties, including transient receptor potential channels, voltage-gated potassium and sodium channels, and certain GPCRs (such as GPR55), among others.Gaston 2017, Perucca 2017
Clinical data
Few moderate- or high-quality clinical trials (randomized controlled trials with a low risk of bias) have been conducted.Perucca 2017, Stockings 2018, Wong 2017 A number of open-label studies conducted by the manufacturers of the prescription CBD preparation Epidiolex have contributed to knowledge surrounding the safety profile of CBD for treatment-resistant epilepsy.Neale 2017, O'Connell 2017, Wong 2017 Retrospective analyses of case reports or clinical data, generally supportive of efficacy of CBD alone or in combination with THC in treatment-resistant seizures, have also been reviewed in the literature.Neale 2017, O'Connell 2017, Perucca 2017, Stockings 2018, Wong 2017
Other CNS conditions
Clinical data
Limited studies have evaluated the efficacy of CBD alone in generalized social anxiety disorder (1 study) and psychosis (2 studies). A review deemed the studies to be of lower quality or with potential for bias.Whiting 2015 Studies are lacking regarding use of CBD alone in Tourette syndrome or tics.NIH 2018
Diabetes
The role of the endocannabinoid system in energy metabolism has been investigated, with emerging evidence showing CBD may slow beta-cell damage in type 1 diabetes mellitus.Di Marzo 2011, Mastinu 2018
Animal data
Limited experiments in nonobese diabetic mice treated with CBD demonstrated reductions in incidence and manifestations of type 1 diabetes.Di Marzo 2011, Zuardi 2008
Clinical data
In one small randomized, double-blind, placebo-controlled study (N=62), patents with noninsulin–treated type 2 diabetes received CBD; tetrahydrocannabivarin (THCV), a combination of CBD and THCV; or placebo for 13 weeks. CBD decreased resistin and increased glucose-dependent insulinotropic peptide. However, the primary end point (change in HDL cholesterol) was not affected by treatment with CBD, THCV, or combination treatment.Jadoon 2016 More research is needed.
Graft-vs-host disease
Animal and in vitro data
Effects of CBD on T cells, cytokines, and other modulators of inflammation have been demonstrated in vitro and in animal models. Insufficient data exist.NIH 2018, Yeshurun 2015
Clinical data
Limited clinical studies evaluating use of CBD alone have been conducted. A small phase 2 study of 48 transplant patients examined effects of CBD on development of GVHD. In addition to GVHD standard prophylaxis (cyclosporine and methotrexate), CBD 300 mg/day was given orally, starting 7 days before transplantation until day 30. No patients developed GVHD during treatment with CBD. Following discontinuation of treatment, 8 patients developed GVHD. It was determined that addition of CBD to GVHD prophylaxis resulted in low cumulative incidence rates of GVHD by day 100.NIH 2018, Yeshurun 2015 Further studies are needed.
Inflammatory bowel disease
Animal and in vitro data
Cannabinoids have been shown to decrease macroscopic inflammation, myeloperoxidase activity, and peristalsis, and to ameliorate inflammation in rodent studies.Naftali 2013, Wallace 2013 CBD demonstrated anti-inflammatory activity in inflamed colonic tissue of inflammatory bowel disease explants.Couch 2017
Clinical data
A small clinical study (N= 20) evaluating CBD 10 mg orally or placebo twice daily in patients with moderately active Crohn disease reported no effect, possibly due to a lack of effect by CBD, the low CBD dose used, and/or the small number of participants.Naftali 2017 Further clinical studies in Crohn disease and inflammatory bowel disease are being conducted, with publication of results pending.NIH 2018
Multiple sclerosis:
Clinical data
Clinical studies evaluating CBD alone in the management of multiple sclerosis are limited, with most studies using commercially available CBD/THC combination preparations.NIH 2018, Nielsen 2018
Other
Clinical trials evaluating CBD alone in the management of Prader-Willi Syndrome are being conducted.NIH 2018
Dosing
Use caution and consider lower doses of CBD in patients with hepatic impairment or those on medications that carry a hepatic risk; liver function should be monitored.FDA 2020
Patients at increased risk of pneumonia or influenza or those on medications that increase such risk should consider vaccinations to increase immunity if taking CBD.
Pregnancy / Lactation
Avoid use. Information regarding safety and efficacy of CBD in pregnancy and lactation is limited. The endocannabinoid system plays an role in regulation of fertility; cannabis use and/or disruptions to the endocannabinoid system have demonstrated negative effects on reproduction.Dekker 2012, FDA 2020, Karasu 2011, Lewis 2012
Interactions
The cannabinoids THC and CBD are both metabolized by the cytochrome P450 enzyme system.(Gaston 2017, Tran 2017) CBD has been shown to exhibit activity at varying degrees on a number of P450 CYP isoforms, including 3A4, 2C9, 2C19, 2C8, 2B6, 2E1 and 1A2. The most relevant interactions for CBD have been noted at 3A4 and 2C19, which are responsible for metabolizing CBD to its primary active metabolite, 7-hydroxy-CBD (7-OH-CBD). Clinically relevant inhibition by CBD on substrates has been noted at 2C19, 2D6, 2C8, and 2C9 with a dual inhibition/induction effect at 1A2 and 2B6.(Brown 2019, Gaston 2017)
The clinical relevance of the in vitro effects demonstrated by CBD on other P450 isoforms (ie, 3A5/7, 2D6, 2C9, 2A6, 2B6, 1A1, 1A2, 1B1, 2J2) and glucuronidation pathways (ie, UGT1A9, UGT2B7) is unknown. However, with commonly used OTC medications like acetaminophen, ibuprofen and naproxen being substrates of UGT enzymes, patients and consumers are at increased risk of substrate side effects when these are used with CBD. The abundant, but inactive hydroxylated-CBD metabolite (7-COOH-CBD) is a P-glycoprotein substrate that has been documented to inhibit both the breast cancer resistance protein (BCRP) and bile salt export pump (BSEP) enzymes; both of which are involved in the transport and excretion pathways of several additional drugs used for common conditions (ie, diabetes, cancer, cardiovascular).(Brown 2019, Perucca 2017) Case reports are minimal.
Anticholinergic agents: Anticholinergic agents may enhance the tachycardic effect of cannabinoid-containing products. Monitor therapy.(Benowitz 1977, Cesamet 2009, Freemon 1975, Williamson 2000)
BCRP/BSEP substrates: Cannabidiol may increase the risk of side effects related to the substrate. Avoid coadministration, reduce substrate dose, and monitor for adverse effects and toxicity.(Brown 2019)
Brivaracetam: Cannabidiol may increase the serum concentration of brivaracetam. Monitor therapy.(Briviact May 2018, Klotz 2019)
Caffeine and caffeine-containing products: CYP1A2 inhibitors (weak) may increase the serum concentration of caffeine and caffeine-containing products. No action needed.(Abernethy 1985, Bachmann 2020, Balogh 1995, Beach 1986, Carbo 1989, Edwards 2017, Epidiolex October 2020, Harder 1988, Kinzig-Schippers 1999, Mavyret April 2020, Michaud 2006, Olysio November 2017, Pegintron January 2019)
Carisoprodol: CYP2C19 inhibitors (moderate) may decrease serum concentrations of the active metabolite(s) of carisoprodol. CYP2C19 inhibitors (moderate) may increase the serum concentration of carisoprodol. Monitor therapy.(Soma August 2019, Tse 2014)
Cilostazol: CYP2C19 inhibitors may increase the serum concentration of cilostazol. Consider therapy modification.(Pletal January 2015, Suri 1999)
Citalopram: CYP2C19 inhibitors (moderate) may increase the serum concentration of citalopram. Consider therapy modification.(Bondolfi 1996, Celexa August 2011, Mailling 2005, Priskorn 1997, Rocha 2010, Rochat 1997)
Clobazam: CYP2C19 inhibitors (moderate) may increase serum concentrations of the active metabolite(s) of clobazam. CYP2C19 inhibitors (moderate) may increase the serum concentration of clobazam. Monitor therapy.(Diacomit August 2018, Epidiolex December 2018, Gaston 2017, Geffrey 2015, Morrison 2019, Onfi June 2018, VanLandingham 2020, Yamamoto 2013)
Clopidogrel: CYP2C19 inhibitors (moderate) may decrease serum concentrations of the active metabolite(s) of clopidogrel. Consider therapy modification.(Brandt 2007, Collet 2009, Fontana 2008, Frere 2008, Gilard 2008, Gilard 2006, Giusti 2009, Hulot 2006, Juurlink 2009, Kim 2008, Mega 2009, Pezalla 2008, Plavix May 2009, Sibbing 2009, Simon 2009, Small 2008, Trenk 2008)
Clozapine: CYP1A2 inhibitors (weak) may increase the serum concentration of CloZAPine. Monitor therapy.(Al Hadithy 2012, Carrillo 1998, Clozaril February 2017, Gabbay 2002, Hagg 2000, Raaska 2004, Rajkumar 2013, Sandson 2007, Schoretsanitis 2020, Szymanski 1991, Vainer 1994)
CNS depressants: CNS depressants may enhance the CNS depressant effect of cannabinoid-containing products. Monitor therapy.(Belgrave 1979, Cesamet May 2006, Chait 1994, Consroe 1979, Dalton 1975, Epidiolex June 2018, Hollister 1986, Johnstone 1975, Macavoy 1975, Marinol July 2006, Perez-Reyes 1988, Reisfield 2010, Ronen 2010, Sativex March 2012, Sativex March 2015, Siemens 1980)
CYP2C19 inducers (moderate): CYP2C19 inducers (moderate) may decrease serum concentrations of the active metabolite(s) of cannabidiol. CYP2C19 inducers (moderate) may decrease the serum concentration of cannabidiol. No action needed.(Epidiolex October 2020, Jiang 2011, Stott 2013)
CYP2C19 inducers (strong): CYP2C19 inducers (strong) may decrease serum concentrations of the active metabolite(s) of cannabidiol. CYP2C19 inducers (strong) may decrease the serum concentration of cannabidiol. Monitor therapy.(Epidiolex October 2020, Jiang 2011, Stott 2013)
CYP2C19 inhibitors (moderate): CYP2C19 inhibitors (moderate) may increase the serum concentration of cannabidiol. Monitor therapy.(Epidiolex December 2018, Morrison 2019)
CYP2C19 inhibitors (strong): CYP2C19 inhibitors (strong) may decrease serum concentrations of the active metabolite(s) of cannabidiol. CYP2C19 inhibitors (strong) may increase the serum concentration of cannabidiol. No action needed.(Epidiolex October 2020)
CYP2C19 substrates: Cannabidiol may increase the risk of side effects related to the substrate. Avoid coadministration, reduce substrate dose, and monitor for adverse effects and toxicity.(Brown 2019)
CYP2C8/9 substrates: Cannabidiol may increase the risk of side effects related to the substrate. Avoid coadministration, reduce substrate dose, and monitor for adverse effects and toxicity.(Brown 2019)
CYP3A4 inducers (moderate): CYP3A4 inducers (moderate) may decrease serum concentrations of the active metabolite(s) of cannabidiol. CYP3A4 inducers (moderate) may decrease the serum concentration of cannabidiol. No action needed.(Epidiolex October 2020, Jiang 2011, Stott 2013)
CYP3A4 inducers (strong): CYP3A4 inducers (strong) may decrease serum concentrations of the active metabolite(s) of cannabidiol. CYP3A4 inducers (strong) may decrease the serum concentration of cannabidiol. Monitor therapy.(Epidiolex October 2020, Jiang 2011, Stott 2013)
CYP3A4 inhibitors (moderate): CYP3A4 inhibitors (moderate) may increase the serum concentration of cannabidiol. Monitor therapy.(Brown 2019, Epidiolex December 2018, Stott 2013, Watanabe 2007)
CYP3A4 inhibitors (strong): CYP3A4 inhibitors (strong) may increase the serum concentration of cannabidiol. Monitor therapy.(Epidiolex October 2020, Jiang 2011, Stott 2013, Watanabe 2007)
CYP3A4 substrates: Cannabidiol may increase the risk of side effects related to the substrate. Avoid coadministration, reduce substrate dose, and monitor for adverse effects and toxicity.(Brown 2019)
Dexlansoprazole: CYP2C19 inhibitors (moderate) may increase the serum concentration of dexlansoprazole. Monitor therapy.(Dexilant June 2018, Miura 2005, Vlase 2011, Yasui-Furukori 2004)
Diazepam: CYP2C19 inhibitors (moderate) may increase the serum concentration of diazepam. Monitor therapy.(Dent 1997, Lemberger 1988, Perucca 1994, Saari 2007, Valium 2016)
Disulfiram: Disulfiram may enhance the adverse/toxic effect of cannabinoid-containing products. Specifically, the risk of a hypomanic episode may be increased. Disulfiram may also produce intolerance to the alcohol contained in the dronabinol oral solution. No action needed. Use of the dronabinol oral solution with disulfiram is contraindicated, but this interaction does not apply to the dronabinol capsules or other cannabinoid-containing products.(Cesamet May 2006, Lacoursiere 1983, Mackie 1994, Marinol July 2006, Syndros July 2016)
Escitalopram: CYP2C19 inhibitors (moderate) may increase the serum concentration of escitalopram. Monitor therapy. Recommendations for management of this interaction found in product labeling may differ by country.(Escitalopram September 2017, Gjestad 2015, Jukic 2018, Lozano 2014, Malling 2005, Rocha 2010, Thase 2013, Tsuchimine 2018)
Etravirine: CYP2C19 inhibitors (moderate) may increase the serum concentration of etravirine. Monitor therapy.(Aouri 2012, Intelence 2019, Kakuda 2013, Toy 2011)
Everolimus: Cannabidiol may increase the serum concentration of everolimus. Monitor therapy.(Ebrahimi-Fakhari 2020, Epidiolex September 2021, Wiemer-Kruel 2019)
Fenfluramine: Cannabidiol may increase the serum concentration of Fenfluramine. No action needed.(Fintepla June 2020)
Flibanserin: CYP2C19 Inhibitors (moderate) may increase the serum concentration of flibanserin. Monitor therapy.(Addyi August 2015)
Fluoxetine: Cannabinoid-containing products may enhance the adverse/toxic effect of fluoxetine. Specifically, the risk of a hypomanic episode may be increased. No action needed.(Anderson 2022, Cesamet May 2006, Cornelius 2010, Marinol July 2006, Stoll 1991)
Fosphenytoin/Phenytoin: Cannabidiol may increase the serum concentration of fosphenytoin/phenytoin. Fosphenytoin/Phenytoin may decrease the serum concentration of cannabidiol. Monitor therapy.(Dilantin November 2018, Epidiolex December 2018, Purkins 2003, Stott 2013, Xcopri November 2019)
Grapefruit juice: Grapefruit juice may increase the serum concentration of tetrahydrocannabinol and cannabidiol. Avoid combination.(Sativex December 2019, Stott 2013)
Hormonal contraceptives: Tetrahydrocannabinol and cannabidiol may decrease the serum concentration of hormonal contraceptives. Consider therapy modification.(Sativex December 2019)
Lansoprazole: CYP2C19 inhibitors (moderate) may increase the serum concentration of lansoprazole. Monitor therapy.(Miura 2005, Prevacid June 2018, Vlase 2011, Yasui-Furukori 2004)
Levothyroxine: Levothyroxine may increase the serum concentration of cannabidiol. No action needed.(Guido 2021)
Lumacaftor and ivacaftor: Lumacaftor and ivacaftor may decrease the serum concentration of CYP2C9 substrates (high risk with inhibitors or inducers). Lumacaftor and ivacaftor may increase the serum concentration of CYP2C9 substrates (high risk with inhibitors or inducers). Monitor therapy.(Orkambi August 2018)
Methadone: Cannabidiol may enhance the CNS depressant effect of methadone. Cannabidiol may increase the serum concentration of methadone. Monitor therapy.(Epidiolex December 2018, Madden 2020, Sativex March 2012, Sativex March 2015)
Moclobemide: CYP2C19 inhibitors (moderate) may increase the serum concentration of moclobemide. Monitor therapy.(Dingemanse 1998, Manerix November 2015, Yu 2001)
Naloxone: Naloxone may enhance the therapeutic effect of cannabinoid-containing products. Naloxone may also decrease effectiveness of cannabinoids. These effects may depend on naloxone dose and frequency, cannabinoid dose and route of administration, and prior cannabinoid exposure. No action needed.(Cooper 2010, Greenwald 2000, Haney 2007, Haney 2003, Haney 2015, Ranganathan 2012, Wachtel 2000)
Naltrexone: Naltrexone may enhance the therapeutic effect of cannabinoid-containing products. Naltrexone may also decrease effectiveness of cannabinoids. These effects may depend on naltrexone dose and frequency, cannabinoid dose and route of administration, and prior cannabinoid exposure. No action needed.(Cooper 2010, Greenwald 2000, Haney 2007, Haney 2003, Haney 2015, Ranganathan 2012, Wachtel 2000)
Omeprazole: CYP2C19 inhibitors (moderate) may increase the serum concentration of omeprazole. Monitor therapy.(Cho 2002, Christensen 2002, Inrebic August 2019, Kamiya 2019, Prilosec August 2018, Sager 2014, Vfend April 2019, Vlase 2010, Vlase 2010, Xcopri November 2019, Yasui-Furukori 2004)
Pirfenidone:CYP2C19 inhibitors (moderate) may increase the serum concentration of pirfenidone. No action needed. The concomitant use of a moderate CYP2C19 inhibitor and pirfenidone should not be used in patients also receiving strong or moderate CYP1A2 inhibitors. No significant interaction is expected when pirfenidone and moderate CYP2C19 inhibitors are combined alone.(Esbiet September 2015, Esbriet December 2014)
Proguanil: CYP2C19 inhibitors (moderate) may decrease serum concentrations of the active metabolite(s) of proguanil. CYP2C19 inhibitors (moderate) may increase the serum concentration of proguanil. Monitor therapy.(Jeppesen 1997, Malarone February 2019)
Sirolimus (conventional): Cannabidiol may increase the serum concentration of sirolimus (conventional). Consider therapy modification.(Ebrahimi-Fakhari 2020, Rapamune August 2022)
Stiripentol: Stiripentol may increase the serum concentration of cannabidiol. Cannabidiol may increase the serum concentration of stiripentol. Monitor therapy.(Ben-Menachem 2020, Devinsky 2018, Diacomit August 2018, Epidiolex October 2020, Morrison 2019)
St. John's wort: St John's wort may decrease the serum concentration of tetrahydrocannabinol and cannabidiol. Consider therapy modification.(Sativex December 2019, Stott 2013)
Sympathomimetics: Cannabinoid-containing products may enhance the tachycardic effect of sympathomimetics. Monitor therapy.(Benowitz 1977, Foltin 1987, Foltin 1990, Foltin 1995, Gash 1978, Lukas 1994, Williamson 2000)
Tacrolimus (systemic): Cannabidiol may increase the serum concentration of tacrolimus (systemic). Monitor therapy.(Cunetti 2018, Epidiolex July 2020, Leino 2019, Moadel 2019)
Tamoxifen: Cannabidiol may decrease serum concentrations of the active metabolite(s) of tamoxifen. No action needed.(Parihar 2020)
Theophylline derivatives: CYP1A2 inhibitors (weak) may increase the serum concentration of theophylline derivatives. Monitor therapy.(Bauman 1982, Campbell 1981, Cohen 1985, Colli 1987, Conrad 1980, Gardner 1983, Granneman 1995, Koren 1985, Lee 1992, Lofgren 1982, Loi 1989, Lombardi 1987, Maeda 1996, Miners 1985, Mojtahedzadeh 2003, Mulkey 1983, Niki 1987, Powell 1984, Sato 1993, Spinler 1993, Staib 1989, Theo-24 August 2017, Tornatore 1982, Vestal 1983, Wijnands 1987, Wijnands 1986, Williams 1987)
Tizanidine: CYP1A2 inhibitors (weak) may increase the serum concentration of tizanidine. Consider therapy modification.(Granfors 2005, Zanaflex November 2013)
UGT1A9/2B7 substrates: Cannabidiol may increase the risk of side effects related to the substrate. Avoid coadministration, reduce substrate dose, and monitor for adverse effects and toxicity.(Brown 2019)
Valproate products: Valproate products may enhance the hepatotoxic effect of cannabidiol. Monitor therapy. This interaction has only been documented with the oral administration of cannabidiol.(Ben-Menachem 2020, Epidiolex October 2020, Gaston 2017)
Voriconazole: CYP2C19 inhibitors (moderate) may increase the serum concentration of voriconazole. Monitor therapy.(Damle 2011, Diflucan March 2018, Vfend April 2019, Wood 2003)
Warfarin: Cannabinoid-containing products may increase the serum concentration of warfarin. Monitor therapy.(Brown 2020, Cortopassi 2020, Damkier 2019, Grayson 2017, Hsu 2020, Yamaori 2012, Yamreudeewong 2009)
Adverse Reactions
Limited data are available; there is insufficient information regarding cumulative exposure or use in special populations, such as in the elderly, children, adolescents, or pregnant and lactating women.FDA 2020
Changes in alertness (drowsiness, sleepiness), GI distress (diarrhea, decreased appetite), and mood changes (irritability, agitation) are most commonly reported with use and should improve with a decrease in dose or discontinuation. However, insomnia, abdominal pain, or upset stomach may also occur. Liver function monitoring is recommended.FDA 2020 Adverse effects appear to be dose-dependent in most cases, and trial data suggest that some effects (ie, somnolence, sedation, asthenia) may diminish with prolonged use. In clinical trials using a prescription CBD (Epidiolex) maintenance dose of 10 mg/kg/day, adverse events that occurred with CBD at more than twice the incidence of placebo were somnolence/sedation/lethargy/fatigue (41% vs 15%); anemia (30% vs 13%); decreased appetite (16% vs 5%); insomnia/sleep disturbance (11% vs 4%); transaminase elevation (8% vs 3%); pneumonia (8% vs 1%); weight loss (3% vs 1%) and gait disturbance (3% vs <1%), respectively.Brown 2019 Seizure aggravation, leading to treatment withdrawal, has been reported in studies of patients with treatment-resistant seizure syndromes.Perucca 2017
A fatal case of Stevens-Johnson syndrome (SJS) was reported in a 56-year old woman 7 days after sublinqually administering a new liposomal CBD extract spray (Natural Native). A mild rash appeared on her extremities 2 days after initial use that was unresponsive to diphenhydramine and oral prednisone and progressed over the next 2 days to a full-body diffuse erythematous and vesicular rash. She indicated previous use of other CBD products that were not problematic. SJS was confirmed; she died approximately 3 weeks later from septic shock.Yin 2020
A 9-year-old boy with a complex medical history was unresponsive, lethargic, and hypothermic with periodic apnea subsequent to an accidental overdose of a CBD oil. He was subsequently intubated due to deteriorating mental status and decreased respiratory drive. The CBD oil was purchased by his mother online and used to treat his cluster seizures. An estimated single-dose of CBD 113 mg (3.7 mg/kg) had been given accidentally by a new home health nurse. The boy was treated, stabilized, and discharged within 72 hours. Per FDA analysis, the product also contained THC 0.53 mg/g.Herbst 2020
A systematic review found no effect on blood pressure or heart rate under control conditions, either with acute or chronic CBD administration. However, in models of stress, acute CBD significantly reduced blood pressure and heart rate that had been increased by the stress.Sultan 2017 In animal studies, CBD significantly increased cerebral blood flow.Sultan 2017
Related/similar drugs
Toxicology
Information specific to CBD is limited. Male reproductive toxicity has been reported in animal studies, including in the male offspring of CBD-treated pregnant females.FDA 2020
Index Terms
- Cannabis sativa
- Cannabis sativa supspecies indica
- Cannabis sativa supspecies ruderalis
References
Disclaimer
This information relates to an herbal, vitamin, mineral or other dietary supplement. This product has not been reviewed by the FDA to determine whether it is safe or effective and is not subject to the quality standards and safety information collection standards that are applicable to most prescription drugs. This information should not be used to decide whether or not to take this product. This information does not endorse this product as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this product. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this product. This information is not specific medical advice and does not replace information you receive from your health care provider. You should talk with your health care provider for complete information about the risks and benefits of using this product.
This product may adversely interact with certain health and medical conditions, other prescription and over-the-counter drugs, foods, or other dietary supplements. This product may be unsafe when used before surgery or other medical procedures. It is important to fully inform your doctor about the herbal, vitamins, mineral or any other supplements you are taking before any kind of surgery or medical procedure. With the exception of certain products that are generally recognized as safe in normal quantities, including use of folic acid and prenatal vitamins during pregnancy, this product has not been sufficiently studied to determine whether it is safe to use during pregnancy or nursing or by persons younger than 2 years of age.
Frequently asked questions
- How to Sleep Better: Tips for Insomnia Relief
- Does Epidiolex contain marijuana?
- What type of drug is Epidiolex?
More about cannabidiol
- Check interactions
- Compare alternatives
- Reviews (7)
- Latest FDA alerts (2)
- Side effects
- Dosage information
- During pregnancy
- Support group
- Drug class: miscellaneous anticonvulsants
- Breastfeeding
- En español
Patient resources
Professional resources
Other brands
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Copyright © 2025 Wolters Kluwer Health