Naltrexone
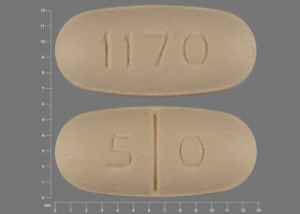
Generic name: Naltrexone
Brand names: Vivitrol, Naltrexone Tablets
Dosage form: intramuscular injection (380 mg), oral tablet (50mg)
Drug classes: Antidotes, Drugs used in alcohol dependence
What is naltrexone?
Naltrexone is a prescription medication used to treat alcohol use disorder (AUD) and opioid use disorder (OUD) to reduce cravings and help control physiological dependence. Naltrexone works by blocking the effects of alcohol and opioid medications, preventing the euphoria and intoxication (the “buzz”) these substances cause, and it also helps reduce the urge or cravings to use alcohol or opioids.
For alcohol use disorder, naltrexone helps people lessen their drinking behaviors and avoid relapses, and over time, cravings for alcohol will decrease. For opioid use disorder, naltrexone prevents euphoria and reduces physiological dependence on opioids such as heroin, morphine, and codeine to help people avoid relapses and remain opioid-free.
Low dose naltrexone (LDN) is used for conditions such as fibromyalgia, Crohn’s disease, multiple sclerosis, and complex regional pain syndrome, as it may work as an anti-inflammatory agent in the central nervous system. Use of low dose naltrexone is an off-label use and is not FDA-approved for these conditions.
Naltrexone is available as an intramuscular injection (Vivitrol) and as oral tablets. The branded tablets (Revia, Depade) have been discontinued, but generic versions are available.
Naltrexone is an opioid antagonist. Its mechanism of action (MOA) is blocking the mu opioid receptor. This medicine also modifies how the hypothalamus, pituitary gland, and adrenal gland (hypothalamic-pituitary-adrenal axis, HPA axis) interact to suppress the amount of alcohol consumed.
What is naltrexone used for?
Naltrexone to is a prescription medication that is FDA-approved:
- to treat alcohol dependence
- for the blockade of the effects of exogenously administered opioids. To prevent relapse to opioid dependence after opioid detoxification.
You should stop drinking alcohol or using opioids before starting this medicine. To avoid precipitated opioid withdrawal, it is recommended you should have an opioid-free interval of a minimum of 7 to 10 days if previously dependent on short-acting opioids. Patients transitioning from buprenorphine or methadone may be vulnerable to precipitation of withdrawal symptoms for as long as two weeks.
Low dose naltrexone (LDN) use is not FDA approved.
This medicine should not be used in children and adolescents under 18 years.
Naltrexone side effects
Common naltrexone side effects
Common side effects of naltrexone may include nausea, vomiting, loss of appetite, joint pain, muscle cramps, headache, dizziness, drowsiness, sleep problems (insomnia), tooth pain or cold symptoms such as stuffy nose, sneezing, sore throat, feeling, anxious or nervous.
Serious naltrexone side effects
Get emergency medical help if you have signs of an allergic reaction: hives, difficulty breathing, swelling of your face, lips, tongue, or throat.
Using opioid medicine while you are receiving this medicine could stimulate opioid withdrawal symptoms. Common withdrawal symptoms are craving for opioids, sweating, yawning, fever, stomach pain, vomiting, diarrhea, watery eyes, runny or stuffy nose, tingling, goose bumps, body aches, shaking, muscle twitching, trouble sleeping, feeling anxious, depressed, fearful, restless or uneasy.
Naltrexone may cause other serious side effects. Call your doctor at once if you have:
- weak or shallow breathing;
- cough that does not go away;
- new or worsening cough, wheezing, trouble breathing;
- severe nausea, vomiting, or diarrhea;
- severe pain, swelling, blistering, skin changes, a dark scab, or a hard lump where the medicine was injected;
- liver problems - stomach pain (upper right side), dark urine, tiredness, vomiting, loss of appetite, clay-colored stools, jaundice (yellowing of the skin or eyes); or
- symptoms of depression - unusual mood or behavior changes, loss of interest in things you once enjoyed, crying, new sleep problems, thoughts about hurting yourself.
You may feel nauseated the first time you receive an injection of this medicine. You may also have a headache, tiredness, joint and muscle pain, loss of appetite, and vomiting.
Tell your healthcare provider if you have any side effect that bothers you, or that does not go away.
This is not a complete list of side effects, and others may occur. Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
Related/similar drugs
Suboxone
Suboxone (buprenorphine and naloxone) is used to treat opiate addiction. Includes Suboxone side ...
Subutex
Subutex (buprenorphine) is used to treat opioid addiction. Includes Subutex side effects ...
Ozempic
Learn about Ozempic (semaglutide) for type 2 diabetes treatment, weight management, cardiovascular ...
Belbuca
Belbuca (buprenorphine) is used for chronic pain management. Includes Belbuca side effects ...
Vivitrol
Vivitrol is a long-acting injectable form of naltrexone used to treat alcohol use disorder and ...
Sublocade
Sublocade information from Drugs.com, includes Sublocade side effects, interactions and indications.
Butrans
Butrans (buprenorphine) transdermal patches are used to treat moderate to severe chronic pain ...
Brixadi
Brixadi (buprenorphine) is a weekly or monthly injection used to treat moderate to severe opioid ...
Campral
Campral is used to help people with alcohol dependence quit drinking alcohol. Learn about side ...
Before taking this medicine
You should not be treated with this medicine if you are allergic to it, or if:
- you are currently addicted to opioids;
- you are having withdrawal symptoms from opioid addiction;
- you are using any opioid pain medicine (including fentanyl, Vicodin, OxyContin, and many others);
- you have failed the naloxone challenge test or have a positive urine screen for opioids or
- you have used any opioid medicine such as methadone, buprenorphine, tramadol, and other opioids within 7 to 14 days.
Also, tell your doctor if you have or have ever had:
- bleeding problems such as hemophilia; or
- liver or kidney disease.
- have alcohol dependence and use opioids.
Pregnancy
Tell your doctor if you are pregnant or plan to become pregnant. It is not known if this medicine will harm your unborn baby. This medication should only be used during pregnancy if the potential benefits justify the potential risk to the fetus.
Breastfeeding
Tell your doctor if you are breastfeeding. It is not known if this medicine passes into your milk when it is administered by IM injection, and it is not known if it can harm your baby. Naltrexone from tablets passes into breast milk. Talk to your healthcare provider about whether you will breastfeed or take this medication. You should not do both.
Important information
This medicine can cause serious side effects, including:
Risk of opioid overdose.
You can accidentally overdose in two ways.
- Naltrexone blocks the effects of opioid drugs. Do not take large amounts of opioids, including opioid-containing medicines, such as heroin or prescription pain pills, to try to overcome the opioid-blocking effects of this medication. This can lead to serious injury, coma, or death.
- After you receive a dose of the extended-release injection form of this medication, its blocking effect slowly decreases and completely goes away over time. If you have used opioid street drugs or opioid-containing medicines in the past, using opioids in amounts that you used before treatment can lead to overdose and death. You may also be more sensitive to the effects of lower amounts of opioids:
- after you have gone through detoxification
- when your next injection is due
- if you miss a dose of this medication
- after you stop treatment with this medicine
It is important that you tell your family and the people closest to you of this increased sensitivity to opioids and the risk of overdose.
You or someone close to you should call 911 or get emergency medical help right away if you:
- have trouble breathing
- become very drowsy with slowed breathing
- have slow, shallow breathing (little chest movement with breathing)
- feel faint, very dizzy, confused, or have unusual symptoms
Talk to your healthcare provider about naloxone, a medicine that is available to patients for the emergency treatment of an opioid overdose.
Call 911 or get emergency medical help right away in all cases of known or suspected opioid overdose, even if naloxone is administered.
Severe reactions at the site of the naltrexone injection (injection site reactions).
Some people have had severe injection site reactions, including tissue death (necrosis), while receiving injections. Some of these injection site reactions have required surgery. This medication must be injected by a healthcare provider. Call your healthcare provider right away if you notice any of the following at any of your injection sites:
- intense pain
- the area feels hard
- large area of swelling
- lumps
- blisters
- an open wound
- a dark scab
Tell your healthcare provider about any reaction at an injection site that concerns you, gets worse over time, or does not get better by two weeks after the injection.
Sudden opioid withdrawal
Anyone who receives naltrexone must not use any type of opioid (must be opioid-free), including street drugs, prescription pain medicines, cough, cold, or diarrhea medicines that contain opioids, or opioid dependence treatments, buprenorphine or methadone, for at least 7 to 14 days before starting this medication. Using opioids in the 7 to 14 days before you start receiving treatment may cause you to suddenly have symptoms of opioid withdrawal when you receive treatment. Sudden opioid withdrawal can be severe, and you may need to go to the hospital.
You must be opioid-free before receiving naltrexone unless your healthcare provider decides that you don't need to go through detox first. Instead, your doctor may decide to give this medication in a medical facility that can treat you for sudden opioid withdrawal.
Liver damage or hepatitis.
This medicine can cause liver damage or hepatitis.
Tell your healthcare provider if you have any of the following symptoms of liver problems during treatment with this medication:
- stomach area pain lasting more than a few days
- dark urine
- yellowing of the whites of your eyes
- tiredness
Your healthcare provider may need to stop treating you with this medication if you get signs or symptoms of a serious liver problem.
You must inform every doctor who treats you that you are taking Naltrexone. Non-opiate based anesthetics should be used if you require an anesthetic in an emergency situation. If you have to use opiate-containing anesthetics, you may need higher doses than usual. You may also be more sensitive to the side-effects (breathing difficulties and circulatory problems).
How should I use this medicine?
Using opioids in the 7 to 14 days before you start receiving naltrexone may cause you to suddenly have symptoms of opioid withdrawal. To avoid this, you should not use short-acting opioids for a minimum of 7-10 days before starting treatment with this medicine.
How to take naltrexone tablets
- Always take this medicine exactly as your doctor has told you. Check with your doctor or pharmacist if you are not sure.
- Take this medication once a day by mouth as your doctor tells you to.
- The amount of time you should take this medication will be decided by your doctor. In certain cases, a longer period of treatment may be beneficial.
How you will receive a naltrexone injection
- Your injection will be given by a healthcare provider every 4 weeks or once a month.
- Get your injection regularly to get the most benefit. Inform your doctor when you received the last injection.
- Do not attempt to inject yourself with this medication. Serious reactions, some that may require hospitalization, might happen.
- This medicine is given as an injection into a muscle in your buttocks using a special needle that comes with it.
- You may notice pain, redness, itching, bruising, swelling, or a hard lump where the medicine was injected. Call your doctor if you have this type of reaction, especially if it gets worse or does not clear up within 2 weeks.
- After this medication is injected, it lasts for a month, and it cannot be removed from the body.
General dosing information
Naltrexone is only part of a complete treatment program that may also include additional forms of counseling and/or monitoring. Follow your doctor's instructions very carefully.
After taking this medicine, your body will be more sensitive to opioids. If you use an opioid medicine in the future, you will need to use less than before the naltrexone treatment. Using the same amount of opioids you used before could lead to overdose or death.
Whenever you need medical treatment, be sure to tell the treating healthcare provider that you are receiving this medication and mention when you got your last dose. This is important because naltrexone can also block the effects of opioid-containing medicines that might be prescribed for you for pain, cough or colds, or diarrhea.
Carry written information with you at all times to alert healthcare providers that you are taking this medication so that they can treat you properly in an emergency. Ask your healthcare provider how you can get a wallet card to carry with you.
Naltrexone Dosing information
Naltrexone dose tablets:
- Alcohol dependence: The recommended dose is 1 tablet (50 mg) once a day.
- Opioid use disorder: Start with half a tablet (25 mg), and if no withdrawal signs occur, increase the dose to 1 tablet (50 mg) a day from then on.
Naltrexone dose intramuscular injection:
- Alcohol dependence and opioid use disorder: The recommended dose is naltrexone 380 mg delivered intramuscularly (IM) as a gluteal injection every 4 weeks or once a month, alternating buttocks for each subsequent.
Comments:
- There is no data specifically addressing switching from buprenorphine or methadone to naltrexone; however, some patients have reported severe manifestations of precipitated
- Patients switching from buprenorphine or methadone may be vulnerable to precipitated withdrawal for up to 2 weeks.
- Be prepared to manage withdrawal symptomatically with non-opioid medications.
- This drug is of value only as a part of a comprehensive management plan that includes measures to ensure the patient takes this medication.
For more detailed dosing information, click on the link below.
What happens if I miss a dose?
If you forget to take your tablet, take it as soon as possible. However, if it is almost time for your next dose, skip the missed dose and go back to your regular dosing schedule. Do not take a double dose to make up for a forgotten dose.
If you miss your appointment for your naltrexone injection, schedule another appointment as soon as possible.
What happens if I overdose?
If you take more naltrexone tablets than you should, tell your Doctor or Pharmacist or contact your nearest hospital emergency department immediately.
What should I avoid while using this medicine?
Do not drive a car, operate machinery, or do other dangerous activities until you know how this medication affects you. This medicine may make you feel dizzy and sleepy.
What other drugs will affect naltrexone?
Tell your healthcare provider about all the medicines you take, including prescription and non-prescription medicines, vitamins, and herbal supplements.
Especially tell your healthcare provider if you take any opioid-containing medicines for pain, cough or colds, or diarrhea.
If you are being treated for alcohol dependence but also use or are addicted to opioid-containing medicines or opioid street drugs, it is important that you tell your healthcare provider before starting naltrexone to avoid having sudden opioid withdrawal symptoms when you start treatment.
Know the medicines you take. Keep a list of them to show your healthcare provider and pharmacist when you get a new medicine.
Storage
- Store naltrexone tablets at 20° to 25°C.
- Store the entire carton containing a naltrexone injection in the refrigerator (2 °C to 8 °C, 36 °F to 46 °F). Unrefrigerated, naltrexone microspheres can be stored at temperatures not exceeding 25 °C (77 °F) for no more than 7 days prior to administration. Do not expose unrefrigerated product to temperatures above 25 °C (77 °F). Do not freeze.
What are the ingredients in naltrexone?
Active ingredient: naltrexone (injection), naltrexone hydrochloride (tablets)
Inactive ingredients:
Vivitrol brand injection: polylactide-co-glycolide (PLG). Diluent ingredients: carboxymethylcellulose sodium, polysorbate 20, sodium chloride, sodium hydroxide and hydrochloric acid as pH adjusters, in water for injection.
Tablets (Chartwell): lactose monohydrate, hypromellose, magnesium stearate, polyethylene glycol, titanium dioxide, colloidal silicon dioxide, hydroxypropyl cellulose, yellow ferric oxide and red ferric oxide.
Inactive ingredients vary among the different generic tablet formulations of naltrexone. Check the product label for your particular formulation for a complete list of inactive ingredients.
Company
The Vivitrol brand of naltrexone injection is manufactured and marketed by Alkermes, Inc. 852 Winter Street, Waltham, MA 02451-1420. A number of different companies manufacture and market generic tablet formulations of this medication.
Popular FAQ
What is low dose naltrexone (LDN)?
Low dose naltrexone means taking a dose of naltrexone that is up to one-tenth, or 10%, of the dose that is usually taken for opioid addiction. A low dose of naltrexone is approximately 4.5mg of naltrexone a day compared with the usual dosage of naltrexone for opioid addiction which is 50mg to 100mg a day. Continue reading
What happens if you drink alcohol while taking naltrexone?
Naltrexone blocks the feelings of intoxication (the “buzz”) from alcohol when you drink it. This allows people with alcohol use disorder to lessen their drinking behaviors enough to stay in treatment, avoid relapses, and take their medication. Over time, cravings for alcohol will decrease. However, naltrexone will not prevent you from becoming impaired while drinking alcohol. Do not use naltrexone so that you can drive or perform other activities under the influence of alcohol. Continue reading
What to avoid when taking naltrexone?
Do NOT take opiates, including heroin or other prescription or illegal opiates while using naltrexone. Taking opiates with naltrexone increases your risk for an overdose, coma and death. Do not use naltrexone if you are dependent on opioids or if you are experiencing opioid withdrawal symptoms. Naltrexone should not be used before you complete a medically-supervised opioid withdrawal lasting at least 7 to 14 days. Continue reading
Should I take naltrexone in the morning or at night?
The manufacturer does not specify if you should take naltrexone tablets in the morning or at night. Take naltrexone exactly as your doctor orders it. Many patients take their medication in the morning to help affirm their continued treatment success for either opioid use disorder or alcohol use disorder. Taking naltrexone tablets after a meal (for example: breakfast) may help to lessen any stomach side effects such as nausea or pain. Continue reading
Does naltrexone cause weight gain?
Weight gain is not a common side effect with oral naltrexone treatment. When used in combination with bupropion, naltrexone is approved to help promote weight loss. Naltrexone is known to frequently cause stomach side effects like nausea and vomiting, stomach pain or cramping, and loss of appetite which could contribute to weight loss. Weight gain and increased appetite have been reported as a possible side effect, but is not common. Continue reading
Acamprosate vs naltrexone: How do they compare?
Acamprosate and naltrexone are two different medications that are used in the treatment of alcohol use disorder. They work in different ways to help people who are dependent on alcohol to abstain from drinking it. Naltrexone is also used for the treatment of opioid use disorder.
Acamprosate was thought to be slightly more effective at helping people with alcohol use disorder remain off alcohol, while naltrexone was thought to be slightly more effective at helping reduce heavy drinking and cravings, according to the results of a meta-analysis which used data from 64 trials.
Results from two small studies, however, indicate that naltrexone is more effective than acamprosate in a number of areas. Continue reading
How long does naltrexone take to work?
Oral naltrexone is well absorbed and will usually begin working within one hour after a dose. Intramuscular naltrexone is an extended-release formulation and has two peaks, first at 2 hours then again 2 to 3 days later, although its therapeutic effect lasts for one month Continue reading
How does naltrexone make you feel?
When taken as directed, naltrexone may reduce your cravings for alcohol or opioids. You’ll feel less of a need to take drugs or drink. Continue reading
What is the mechanism of action for naltrexone?
Naltrexone is a pure opiate receptor antagonist and works by primarily binding at the mu opioid receptors. By binding to these receptors, it blocks the euphoric (pleasurable or "high") effects linked with alcohol use or opioids. Continue reading
References
- National Library of Medicine. Chartwell Naltrexone Hydrochloride Tablet Product Label.
- National Library of Medicine. Vivitrol Product Label.
- Electronic Medicines Compendium (ECM) Naltrexone Hydrochloride 50 mg Tablets Product Label.
- Singh D, Saadabadi A. Naltrexone. [Updated 2022 Jun 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-
- Center for Substance Abuse Treatment. Incorporating Alcohol Pharmacotherapies Into Medical Practice. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 2009. (Treatment Improvement Protocol (TIP) Series, No. 49.) Chapter 4—Oral Naltrexone.
- The use of low-dose naltrexone (LDN) as a novel anti-inflammatory treatment for chronic pain
More about naltrexone
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (599)
- Drug images
- Latest FDA alerts (1)
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: antidotes
- Breastfeeding
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.