Atezolizumab
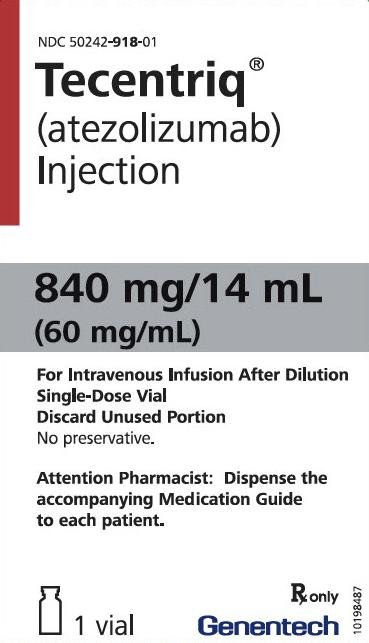
Generic name: atezolizumab
Brand name: Tecentriq
Dosage form: intravenous (infusion) injection
Drug class: Anti-PD-1 and PD-L1 monoclonal antibodies (immune checkpoint inhibitors)
What is atezolizumab?
Atezolizumab is a type of immunotherapy drug that helps the body's immune system to track down and fight cancer. It is a monoclonal antibody that works by blocking a protein called programmed death-ligand 1 (PD-L1). It is part of a group of drugs called immune checkpoint inhibitors, which help to extend the amount of time a person can live with cancer or life without their cancer getting worse.
Atezolizumab. was first approved by the US Food and Drug Administration (FDA) in 2016.
What is atezolizumab used for?
Atezolizumab is a prescription medicine used to treat adults with:
- a type of bladder and urinary tract cancer called urothelial carcinoma. Atezolizumab may be used when your bladder cancer has spread or cannot be removed by surgery, and if you have any one of the following conditions:
- you are not able to take chemotherapy that contains a medicine called cisplatin, and your cancer tests positive for "PD-L1", or
- you are not able to take chemotherapy that contains any platinum regardless of "PD-L1" status.
- a type of lung cancer called non-small cell lung cancer (NSCLC).
- Atezolizumab may be used alone as a treatment for your lung cancer:
- to help prevent your lung cancer from coming back after your tumor(s) has been removed by surgery and you have received platinum-based chemotherapy, and
- you have stage 2 to stage 3A NSCLC (talk to your healthcare provider about what these stages mean), and
- your cancer tests positive for "PD-L1".
- Atezolizumab may be used alone as your first treatment when your lung cancer:
- has spread or grown, and
- your cancer tests positive for "high PD-L1", and
- your tumor does not have an abnormal "EGFR" or "ALK" gene.
- Atezolizumab may be used with the medicines bevacizumab, paclitaxel, and carboplatin as your first treatment when your lung cancer:
- has spread or grown, and
- is a type called "non-squamous NSCLC", and
- your tumor does not have an abnormal "EGFR" or "ALK" gene.
- Atezolizumab may be used with the medicines paclitaxel protein-bound and carboplatin as your first treatment when your lung cancer:
- has spread or grown, and
- is a type called "non-squamous NSCLC", and
- your tumor does not have an abnormal "EGFR" or "ALK" gene.
- Atezolizumab may also be used alone when your lung cancer:
- has spread or grown, and
- you have tried chemotherapy that contains platinum, and it did not work or is no longer working.
- if your tumor has an abnormal "EGFR" or "ALK" gene, you should have also tried an FDA-approved therapy for tumors with these abnormal genes, and it did not work or is no longer working.
- Atezolizumab may be used alone as a treatment for your lung cancer:
- a type of lung cancer called small cell lung cancer (SCLC). Atezolizumab may be used with the chemotherapy medicines carboplatin and etoposide as your first treatment when your lung cancer
- is a type called "extensive-stage SCLC," which means that it has spread or grown.
- a type of liver cancer called hepatocellular carcinoma (HCC). Atezolizumab may be used with the medicine bevacizumab when your liver cancer:
- has spread or cannot be removed by surgery, and
- you have not received other medicines by mouth or injection through your vein (IV) to treat your cancer.
- a type of skin cancer called melanoma. Atezolizumab may be used with the medicines cobimetinib and vemurafenib when your melanoma:
- has spread to other parts of the body or cannot be removed by surgery, and
- has a certain type of abnormal "BRAF" gene. Your healthcare provider will perform a test to make sure this atezolizumab combination is right for you.
It is not known if atezolizumab is safe and effective in children.
Important information
Atezolizumab is a medicine that may treat certain cancers by working with your immune system. Atezolizumab can cause your immune system to attack normal organs and tissues in any area of your body and can affect the way they work. These problems can sometimes become severe or life-threatening and can lead to death. You can have more than one of these problems at the same time. These problems may happen anytime during your treatment or even after your treatment has ended.
Call or see your healthcare provider right away if you develop any new or worse signs or symptoms, including:
- Lung problems.
- cough
- shortness of breath
- chest pain
- Intestinal problems.
- diarrhea (loose stools) or more frequent bowel movements than usual
- stools that are black, tarry, sticky, or have blood or mucus
- severe stomach-area (abdomen) pain or tenderness
- Liver problems.
- yellowing of your skin or the whites of your eyes
- severe nausea or vomiting
- pain on the right side of your stomach area (abdomen)
- dark urine (tea colored)
- bleeding or bruising more easily than normal
- Hormone gland problems.
- headaches that will not go away or unusual headaches
- eye sensitivity to light
- eye problems
- rapid heart beat
- increased sweating
- extreme tiredness
- weight gain or weight loss
- feeling more hungry or thirsty than usual
- urinating more often than usual
- hair loss
- feeling cold
- constipation
- your voice gets deeper
- dizziness or fainting
- changes in mood or behavior, such as decreased sex drive, irritability, or forgetfulness
- Kidney problems.
- decrease in your amount of urine
- blood in your urine
- swelling of your ankles
- loss of appetite
- Skin problems.
- rash
- itching
- skin blistering or peeling
- painful sores or ulcers in mouth or nose, throat, or genital area
- fever or flu-like symptoms
- swollen lymph nodes
- Problems can also happen in other organs.
These are not all of the signs and symptoms of immune system problems that can happen with atezolizumab. Call or see your healthcare provider right away for any new or worse signs or symptoms, including:- chest pain, irregular heartbeat, shortness of breath, or swelling of ankles
- confusion, sleepiness, memory problems, changes in mood or behavior, stiff neck, balance problems, tingling or numbness of the arms or legs
- double vision, blurry vision, sensitivity to light, eye pain, changes in eye sight
- persistent or severe muscle pain or weakness, muscle cramps
- low red blood cells, bruising
- Infusion reactions that can sometimes be severe or life-threatening. Signs and symptoms of infusion reactions may include:
- chills or shaking
- itching or rash
- flushing
- shortness of breath or wheezing
- dizziness
- feeling like passing out
- fever
- back or neck pain
- Complications, including graft-versus-host disease (GVHD), in people who have received a bone marrow (stem cell) transplant that uses donor stem cells (allogeneic). These complications can be serious and can lead to death. These complications may happen if you underwent transplantation either before or after being treated with atezolizumab. Your healthcare provider will monitor you for these complications.
Getting medical treatment right away may help keep these problems from becoming more serious.
Your healthcare provider will check you for these problems during your treatment with atezolizumab. Your healthcare provider may treat you with corticosteroid or hormone replacement medicines. Your healthcare provider may also need to delay or completely stop treatment with atezolizumab if you have severe side effects.
What should I tell my doctor before receiving atezolizumab?
Before receiving atezolizumab, tell your healthcare provider about all of your medical conditions, including if you:
- have immune system problems such as Crohn's disease, ulcerative colitis, or lupus
- have received an organ transplant
- have received or plan to receive a stem cell transplant that uses donor stem cells (allogeneic)
- have received radiation treatment to your chest area
- have a condition that affects your nervous system, such as myasthenia gravis or Guillain-Barré syndrome
How should I receive atezolizumab?
- Your healthcare provider will give you atezolizumab into your vein through an intravenous (IV) line over 30 to 60 minutes.
- Atezolizumab is usually given every 2, 3, or 4 weeks.
- Your healthcare provider will decide how many treatments you need.
- Your healthcare provider will test your blood to check you for certain side effects.
- For treatment of a type of skin cancer called melanoma, your healthcare provider will also prescribe you cobimetinib and vemurafenib. Take cobimetinib and vemurafenib exactly as your healthcare provider tells you.
What happens if I miss a dose?
If you miss any appointments, call your healthcare provider as soon as possible to reschedule your appointment.
Dosing information
- Urothelial Carcinoma. Administer atezolizumab as a single agent as 840 mg every 2 weeks, 1200 mg every 3 weeks, or 1680 mg every 4 weeks.
- NSCLC. In the adjuvant setting, administer atezolizumab following resection and up to 4 cycles of platinum-based chemotherapy as 840 mg every 2 weeks, 1200 mg every 3 weeks or 1680 mg every 4 weeks for up to 1 year. In the metastatic setting, administer atezolizumab as 840 mg every 2 weeks, 1200 mg every 3 weeks, or 1680 mg every 4 weeks. When administering with chemotherapy with or without bevacizumab, administer atezolizumab prior to chemotherapy and bevacizumab when given on the same day.
- Small Cell Lung Cancer. Administer atezolizumab as 840 mg every 2 weeks, 1200 mg every 3 weeks, or 1680 mg every 4 weeks. When administering with carboplatin and etoposide, administer atezolizumab prior to chemotherapy when given on the same day.
- Hepatocellular Carcinoma. Administer atezolizumab as 840 mg every 2 weeks, 1200 mg every 3 weeks, or 1680 mg every 4 weeks. Administer TECENTRIQ prior to bevacizumab when given on the same day. Bevacizumab is administered at 15 mg/kg every 3 weeks.
- Melanoma. Following completion of a 28 day cycle of cobimetinib and vemurafenib, administer atezolizumab 840 mg every 2 weeks, 1200 mg every 3 weeks, or 1680 mg every 4 weeks with cobimetinib 60 mg orally once daily (21 days on /7 days off) and vemurafenib 720 mg orally twice daily.
What are the side effects of atezolizumab?
Atezolizumab can cause serious side effects, including:
- See "Important information" above.
The most common side effects of atezolizumab when used alone include:
- feeling tired or weak
- decreased appetite
- nausea
- cough
- shortness of breath
The most common side effects of atezolizumab when used in lung cancer with other anti-cancer medicines include:
- feeling tired or weak
- nausea
- hair loss
- constipation
- diarrhea
- decreased appetite
The most common side effects of atezolizumab when used in hepatocellular carcinoma with bevacizumab include:
- high blood pressure
- feeling tired or weak
- too much protein in the urine
The most common side effects of atezolizumab when used in melanoma with cobimetinib and vemurafenib include:
- skin rash
- joint, muscle, or bone pain
- feeling tired or weak
- liver injury
- fever
- nausea
- itching
- swelling of legs or arms
- mouth swelling (sometimes with sores)
- low thyroid hormone levels
- sunburn or sun sensitivity
Atezolizumab may cause fertility problems in females, which may affect the ability to have children. Talk to your healthcare provider if you have concerns about fertility.
These are not all the possible side effects of atezolizumab.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Related/similar drugs
Opdivo Qvantig
Opdivo Qvantig is used to treat adults with melanoma, non-small cell lung cancer, renal cell ...
Rybrevant
Rybrevant is used to treat adults with non-small cell lung cancer (NSCLC) that has spread to other ...
Opdivo
Opdivo is used to treat many cancers, such as melanoma, non-small cell lung cancer, malignant ...
Keytruda
Keytruda is used to treat multiple types of cancer such as melanoma, non-small cell lung cancer ...
Avastin
Avastin is used to brain tumors and cancers of the kidney, colon, rectum, or lung. Learn about side ...
Taxol
Taxol (paclitaxel) is used to treat breast cancer, lung cancer, and ovarian cancer. Includes Taxol ...
Tagrisso
Tagrisso (osimertinib) may be used to treat adults with non-small cell lung cancer (NSCLC) whose ...
Lenvima
Lenvima (lenvatinib) is used to treat thyroid cancer, advanced renal cell carcinoma, hepatocellular ...
Nivolumab
Nivolumab (brand name Opdivo) is an immunotherapy treatment that treats many cancers, such as ...
Paclitaxel
Paclitaxel systemic is used for breast cancer, breast cancer, adjuvant, breast cancer, metastatic ...
Interactions
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
Pregnancy and breastfeeding
Tell your doctor if you are pregnant or plan to become pregnant. atezolizumab can harm your unborn baby. Tell your healthcare provider right away if you become pregnant or think you may be pregnant during treatment with atezolizumab.
Females who are able to become pregnant:
- Your healthcare provider should do a pregnancy test before you start treatment with atezolizumab.
- You should use an effective method of birth control during your treatment and for at least 5 months after the last dose of atezolizumab.
Tell your doctor if you are breastfeeding or plan to breastfeed. It is not known if atezolizumab passes into your breast milk. Do not breastfeed during treatment and for at least 5 months after the last dose of atezolizumab.
Storage
Store atezolizumab vials under refrigeration at 2°C to 8°C (36°F to 46°F) in original carton to protect from light. Do not freeze. Do not shake.
What are the ingredients in atezolizumab?
Active ingredient: atezolizumab
Inactive ingredients: glacial acetic acid, L-histidine, polysorbate 20 and sucrose
Atezolizumab is manufactured by Genentech, Inc., a member of the Roche Group, 1 DNA Way, South San Francisco, CA 94080-4990 USA, under the brandname Tecentiq.
Atezolizumab Biosimilars
Biosimilar and interchangeable products are biological products that are highly similar to and have no clinically meaningful differences from the reference product.
Reference products
These are biological products that have already been approved by the FDA, against which biosimilar products are compared. There is 1 for atezolizumab.
Tecentriq (atezolizumab) - Genentech, Inc.
| Formulation type | Strength |
|---|---|
| Single-Dose Vial | 1,200 mg/20 mL (60 mg/mL) |
| Single-Dose Vial | 840 mg/14 mL (60 mg/mL) |
View Tecentriq information in detail.
Popular FAQ
Are there cost-saving programs for Tecentriq?
Tecentriq is an expensive cancer medication, but there may be options to help you afford this medicine, no matter the type of insurance you have or if you have no insurance at all. You can also call Genentech at 1-888-249-4918 (6AM-5PM PST, Monday through Friday) to determine which financial programs may be right for you. Continue reading
How effective is it?
Atezolizumab (Tecentriq) is approved to treat several different types of cancer. Cancer treatment is always individualized for each patient. It’s effectiveness and your length of response will depend upon your diagnosis, previous treatments, and other medical conditions, among other factors. Continue reading
Is atezolizumab (Tecentriq) a chemotherapy or immunotherapy drug?
Atezolizumab (brand name: Tecentriq) is a type of immunotherapy drug called an “immune checkpoint inhibitor”. It helps to stimulate the body’s immune system to fight certain types cancer, including lung, liver and skin cancer. Continue reading
Does atezolizumab (Tecentriq) cause hair loss?
Hair loss (alopecia) is listed as a common side effect with atezolizumab (Tecentriq) when used with certain other cancer treatments. Hair loss was not reported as a side effect when used as a single agent for urothelial (bladder) cancer treatment (but Tecentriq is no longer FDA-approved to be used in bladder cancer). Continue reading
How is atezolizumab (Tecentriq) administered?
Atezolizumab (Tecentriq) is given by a slow intravenous (IV) infusion into your vein, usually once every 2, 3 or 4 weeks. Your initial infusion typically lasts for 60 minutes, and infusions after this may be reduced to 30 minutes, based on your tolerability. Atezolizumab and hyaluronidase-tqjs (Tecentriq Hybreza) is given as a subcutaneous (under the skin) injection that takes about 7 minutes and is normally given once every 3 weeks. These products are administered by your healthcare provider. Continue reading
What type of cancer is Tecentriq used to treat?
Tecentriq (atezolizumab) is an immune checkpoint inhibitor used to treat non-small cell lung cancer (NSCLC), small cell lung cancer (SCLC), heptatocellular (liver) carcinoma (HCC), melanoma (skin cancer), and alveolar soft part sarcoma (ASPS), a rare soft tissue tumor. Continue reading
References
More about atezolizumab
- Check interactions
- Compare alternatives
- Reviews (6)
- Latest FDA alerts (2)
- Side effects
- Dosage information
- During pregnancy
- Drug class: anti-PD-1 and PD-L1 monoclonal antibodies (immune checkpoint inhibitors)
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.