Tretinoin (Monograph)
Drug class: Antineoplastic Agents
Warning
- Embryo-fetal Toxicity
-
Can cause embryo-fetal loss and malformations when given to pregnant women.
-
Inform patients of the potential fetal risk. Females of reproductive potential must have a negative pregnancy test prior to initiating tretinoin.
-
Advise females of reproductive potential to use 2 effective contraceptive methods during treatment and for 1 month after the last dose.
-
Male patients with female partners of reproductive potential should use effective contraception during treatment and for 1 week after the last dose.
- Differentiation Syndrome
-
Differentiation syndrome, which can be life-threatening or fatal, has occurred in about 26% of patients with acute promyelocytic leukemia administered tretinoin.
-
High-dose corticosteroid therapy and hemodynamic monitoring should be implemented immediately upon initial signs or symptoms of differentiation syndrome and continue until resolution.
-
Consider withholding tretinoin therapy for moderate and severe differentiation syndrome until resolution.
Introduction
Antineoplastic agent; retinoid.
Uses for Tretinoin
Acute Promyelocytic Leukemia
Used orally for the induction of remission in adults and pediatric patients ≥1 year of age with acute promyelocytic leukemia (APL), characterized by the presence of certain genetic markers (i.e., 15;17 chromosomal translocation and/or PML/RAR-α gene) in patients with relapsed or refractory disease following anthracycline-based chemotherapy or in patients for whom anthracycline therapy is contraindicated.
May initiate tretinoin therapy based on the morphologic diagnosis of APL, but perform cytogenetic evaluation to confirm presence of the t(15;17) translocation genetic marker or molecular diagnostic testing for the PML/RAR-α fusion protein. Tretinoin is not recommended for use in patients without these genetic markers.
Also has been used as initial treatment in patients with newly diagnosed APL† [off-label].
Current guidelines for APL include various treatment options; selection of an appropriate regimen is determined by patient's risk category (low, intermediate, or high based on WBC counts). With the inclusion of arsenic trioxide in current treatment regimens for APL, use of traditional chemotherapy is generally restricted to the induction phase for high-risk patients.
Experts currently recommend use of tretinoin in combination with arsenic trioxide for initial treatment† [off-label] of APL in patients with low- to intermediate-risk disease (WBC count ≤10,000/mm3). The combination of tretinoin and chemotherapy, followed by arsenic trioxide-based consolidation therapy, is recommended for newly-diagnosed patients with high-risk disease (WBC >10,000/mm3).
In children with APL, experts recommend use of tretinoin and arsenic trioxide in standard-risk patients, and with short-course chemotherapy during induction in high-risk patients.
Although tretinoin is only FDA-labeled for use in induction therapy, the drug also has been used for consolidation therapy† [off-label]. For patients who are treated with tretinoin and arsenic trioxide, maintenance therapy not likely to be necessary.
Tretinoin Dosage and Administration
General
Pretreatment Screening
-
Verify pregnancy status in females of reproductive potential within 1 week prior to initiating tretinoin treatment with a pregnancy test with a sensitivity of at least 50 mIU/mL.
-
Monitor fasting triglycerides and cholesterol and liver function at baseline.
Patient Monitoring
-
Monitor for signs or symptoms of differentiation syndrome, especially during the first month of treatment.
-
Monitor for signs and symptoms of intracranial hypertension, especially in pediatric patients.
-
Monitor fasting triglycerides and cholesterol periodically during treatment.
-
Monitor liver function tests during treatment as clinically indicated.
Administration
Oral Administration
Administer orally in 2 equally divided doses. Take capsules with a meal. Swallow whole with water; do not chew, dissolve, or open capsules.
If a dose is missed, do not take missed dose unless it is >10 hours until the next scheduled dose.
If vomiting occurs after administration, do not take an additional dose. Continue with the next scheduled dose.
Dosage
Pediatric Patients
Acute Promyelocytic Leukemia
Oral
Induction of remission in patients ≥1 year of age: 45 mg/m2 daily administered in 2 evenly divided doses until complete remission documented.
Continue until 30 days after complete remission is achieved or 90 days of treatment have elapsed, whichever occurs first.
Maximum tolerated dose is lower in pediatric patients than adults. Consider dosage reduction if serious or intolerable drug toxicity. A lower daily dose of 25 mg/m2 has been used in the pediatric population, which is thought to decrease the incidence of intracranial hypertension.
Adults
Acute Promyelocytic Leukemia
Oral
Induction of remission: 45 mg/m2 daily administered in 2 evenly divided doses until complete remission documented.
Continue until 30 days after complete remission was achieved or 90 days of treatment have elapsed, whichever occurs first.
Although tretinoin not FDA-labeled for consolidation therapy† [off-label] in patients with APL, the drug has been administered at a dosage of 45 mg/m2 alternating 7 days on and 7 days off for a total of 28 weeks for consolidation. Alternatively, a consolidation regimen of 45 mg/m2 daily for 2 weeks every 4 weeks for a total of 7 cycles (28 weeks total) has been used.
Dosage Modification for Toxicity
Consider withholding tretinoin therapy until resolution in patients experiencing moderate or severe differentiation syndrome and in patients with liver function test results >5 times the upper limit of normal.
Cautions for Tretinoin
Contraindications
-
Known hypersensitivity to tretinoin, any of its components, or other retinoids.
Warnings/Precautions
Warnings
Embryo-fetal Toxicity
May cause fetal harm; embryo-fetal loss and malformations occur when administered to pregnant women (see Boxed Warning).
Apprise pregnant women of potential fetal risk. Advise females of reproductive potential to use 2 effective contraceptive methods during treatment and for 1 month following last tretinoin dose. Advise male patients with female partners of reproductive potential to use effective contraception during treatment and for 1 week following last dose.
Differentiation Syndrome
Differentiation syndrome reported in patients with APL treated with tretinoin (see Boxed Warning). May be accompanied by impaired myocardial contractility and episodic hypotension, and can occur with or without concomitant leukocytosis. Onset generally occurs within first month of treatment and can occur after a single dose. Endotracheal intubation and mechanical ventilation were required in some cases and several fatalities have occurred.
At first signs or symptoms, immediately administer dexamethasone 10 mg IV every 12 hours and continue until signs and symptoms have abated for at least 3 days. Hemodynamic monitoring should also occur until sign and symptom resolution. Consider withholding tretinoin therapy for moderate and severe disease until resolution.
Other Warnings and Precautions
Leukocytosis
Rapidly evolving leukocytosis associated with an increased risk of life-threatening complications has been reported. Patients with a baseline WBC >5000 cells/mm3 have an increased risk while those who receive concomitant chemotherapy may be at reduced risk.
Consider administration of cytoreductive chemotherapy (e.g., anthracycline if not contraindicated or hydroxyurea) with tretinoin in patients with leukocytosis as clinically indicated.
Patients Without the t(15;17) Translocation or PML/RARα Fusion
May initiate therapy based on the morphologic diagnosis of APL. However, confirm diagnosis with detection of the t(15;17) translocation genetic marker or PML/RARα fusion. Tretinoin is not recommended for use in patients without these genetic markers.
Intracranial hypertension
Intracranial hypertension reported, especially in pediatric patients. Early signs and symptoms include papilledema, headache, nausea, vomiting, and visual disturbances. Evaluate patients with symptoms and, if present, perform a neurological assessment and initiate appropriate therapy.
Consider dose reduction, interruption of therapy, or discontinuation of tretinoin as necessary. Avoid concomitant use of tretinoin with other agents that cause intracranial hypertension.
Lipid Abnormalities
Hypercholesterolemia and/or hypertriglyceridemia, which may be reversible upon completion of therapy, reported. Venous thrombosis and myocardial infarction reported in patients who would ordinarily be at low risk for such events. Monitor fasting triglycerides and cholesterol at baseline and periodically during treatment.
Hepatotoxicity
Elevated liver function tests reported; test abnormalities usually resolve during or after treatment.
Monitor liver function tests at baseline and during treatment as clinically indicated. Consider withholding therapy if liver function test results are >5 times the ULN until resolution.
Thromboembolic Events
Venous and arterial thromboembolic events reported. May occur during initial month of treatment and patients given anti-fibrinolytics may be at increased risk.
Avoid concomitant use of tretinoin and anti-fibrinolytics.
Specific Populations
Pregnancy
Can cause severe, life-threatening birth defects or fetal death if taken during pregnancy.
Lactation
Not known whether tretinoin is distributed into human milk. Do not breastfeed during treatment with tretinoin and for 1 week after last dose.
Females and Males of Reproductive Potential
Tretinoin can cause embryo-fetal loss and malformations when administered to pregnant women.
Verify pregnancy status in females of reproductive potential prior to therapy. Must have a negative pregnancy test within 1 week prior to therapy initiation with a test sensitivity of at least 50 mIU/mL.
Females of reproductive potential should either abstain from sexual intercourse or use 2 effective contraceptive methods during therapy and for 1 month after last dose. Male patients with female partners of reproductive potential should use effective contraception during therapy and for 1 week after last dose.
May impair male fertility. Reversibility of this effect unknown.
Pediatric Use
Safety and efficacy established in pediatric patients ≥1 year of age. Maximum tolerated dose is lower in pediatric patients as compared to adults.
Some pediatric patients experience severe headache and intracranial hypertension, requiring treatment with analgesics and lumbar puncture.
May need to reduce dosage if serious and/or intolerable adverse effects occur.
Geriatric Use
Safety and efficacy in those ≥60 years of age similar to those in younger patients.
Hepatic Impairment
Manufacturer states that the pharmacokinetics of tretinoin have not been evaluated in individuals with hepatic impairment.
Renal Impairment
Manufacturer states that the pharmacokinetics of tretinoin have not been evaluated in individuals with renal impairment.
Common Adverse Effects
Most common adverse reactions (≥30%): headache, fever, skin/mucous membrane dryness, bone pain, malaise, shivering, upper respiratory tract disorders, dyspnea, hemorrhage, infections, nausea/vomiting, rash, peripheral edema, leukocytosis, pain, GI hemorrhage, chest discomfort, abdominal pain.
Drug Interactions
Metabolized by CYP isoenzymes.
Drugs Affecting Hepatic Microsomal Enzymes
Concomitant use of drugs that affect CYP3A may alter metabolism of tretinoin.
Strong inducers of CYP3A: Potential pharmacokinetic interaction (decreased plasma tretinoin concentrations). Avoid coadministration if possible.
Strong inhibitors of CYP3A: Potential pharmacokinetic interaction (increased plasma tretinoin concentrations). Avoid coadministration if possible. If coadministration is necessary, monitor more frequently for adverse effects.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Antifibrinolytic agents (e.g., tranexamic acid, aminocaproic acid) |
Fatal thrombotic complications may occur with concomitant use |
Avoid concomitant use |
|
Hydroxyurea |
Concomitant use may cause a synergistic effect leading to massive cell lysis Bone marrow necrosis, sometimes fatal, has been reported |
Use concomitantly with caution |
|
Ketoconazole |
Possible increased plasma tretinoin concentrations; administration of ketoconazole associated with 72% increase in tretinoin AUC |
Avoid coadministration if possible; if coadministration is necessary, monitor more frequently for adverse effects |
|
Tetracyclines |
Increased risk of intracranial hypertension |
Avoid concomitant use |
|
Vitamin A |
Concomitant use may aggravate symptoms of hypervitaminosis A |
Avoid concomitant use |
Tretinoin Pharmacokinetics
Absorption
Bioavailability
About 50%.
Food
Effect of food on tretinoin absorption not evaluated; generally, retinoid absorption is enhanced by food.
Plasma Concentrations
Time to reach peak concentrations was 1 to 2 hours.
Distribution
Extent
Not known whether tretinoin distributes into human milk.
Plasma Protein Binding
>95% (mainly albumin).
Elimination
Metabolism
Evidence that tretinoin induces its own metabolism.
Metabolized in the liver by CYP450 3A4, 2C8, and 2E and undergoes glucuronidation by UGT2B7.
Metabolites 4-oxo retinoic acid and 4-oxo trans retinoic acid glucuronide have 33% of activity of parent compound.
Elimination Route
>90% in urine and feces; 63% in urine within 72 hours, and 31% in feces within 6 days.
Half-life
0.5–2 hours after initial dose.
Special Populations
The effect of age, sex, race, renal impairment, and hepatic impairment on pharmacokinetics unknown.
Stability
Storage
Oral
Capsules
20–25°C. Protect from light.
Actions
-
Precise mechanism(s) of action not fully elucidated.
-
PML/RAR-α fusion protein resulting from 15;17 chromosomal translocation apparently blocks myeloid differentiation at the promyelocyte stage; induces cellular differentiation and decreases proliferation of APL cells.
-
Causes initial maturation of primitive promyelocytes (derived from the cellular leukemic clone) followed by normal, polyclonal hematopoietic cell repopulation of bone marrow and peripheral blood.
-
Apoptosis (programmed cell death) may be a mechanism for eliminating malignant cells.
-
Tretinoin alone does not eradicate the leukemic clone because PML/RAR-α fusion protein usually can be detected following induction.
Advice to Patients
-
Advise patients to swallow tretinoin capsules whole with water and not to chew, dissolve, or open the capsules.
-
Advise patients not to take a missed dose of tretinoin unless it is more than 10 hours until the next scheduled dose. Inform patients that if vomiting occurs after tretinoin administration, they should not take an additional dose, but continue with the next scheduled dose.
-
Advise patients that their ability to drive or operate machinery might be impaired, especially if experiencing dizziness or severe headache.
-
Advise patients of the risk of differentiation syndrome. Advise patients to immediately report any symptoms of differentiation syndrome, such as fever, cough or difficulty breathing, decreased urinary output, low blood pressure, rapid weight gain, or swelling of their arms or legs, to their clinician.
-
Advise patients that tretinoin is not recommended for use in patients without t(15;17) translocation or PML/RAR-α fusion.
-
Inform patients of the risk of leukocytosis that can be rapidly evolving and life-threatening.
-
Inform patients of the risk of intracranial hypertension, especially in pediatric patients.
-
Inform patients of the risk of hypercholesterolemia and/or hypertriglyceridemia during treatment with tretinoin and the need for periodic laboratory monitoring.
-
Inform patients of the risk of hepatotoxicity during treatment with tretinoin and the need for periodic laboratory monitoring.
-
Inform patients that venous and arterial thromboembolic events, including cerebrovascular accident, myocardial infarction, and renal infarct can occur during treatment.
-
Advise females to inform their clinician if they are or plan to become pregnant or plan to breast-feed. Perform pregnancy testing before initiation of tretinoin and advise patients of the potential risk to the fetus.
-
Inform women to use effective contraception (i.e., 2 reliable forms of contraception simultaneously unless abstinence is the chosen method) during tretinoin therapy and for 1 month following discontinuance. Advise male patients with female partners of reproductive potential to use effective contraception during tretinoin therapy and for 1 week after the last dose.
-
Advise women not to breast-feed during treatment with tretinoin and for 1 week after the final dose.
-
Advise patients to inform their healthcare provider about all concomitant medications, including prescription medicine, over the counter drugs, vitamins, and herbal products.
-
Inform patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
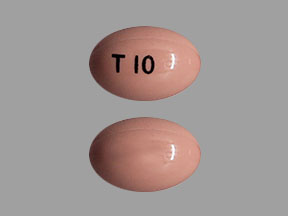
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules |
10 mg* |
Tretinoin Capsules |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions July 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Frequently asked questions
- What are the most common skin conditions? (with photos)
- Is tazarotene better than tretinoin?
- Can you use Winlevi and tretinoin together?
- What is the difference between Altreno and other topical tretinoin acne formulations?
More about tretinoin
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (3)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Support group
- Drug class: miscellaneous antineoplastics
- Breastfeeding
- En español