Tranexamic Acid (Monograph)
Brand names: Cyklokapron, Lysteda
Drug class: Hemostatics
Introduction
Antifibrinolytic agent; synthetic derivative of lysine.
Uses for Tranexamic Acid
Prevention of Bleeding in Hemophilia Patients Undergoing Dental Procedures
IV formulation FDA-labeled for short-term (2–8 days) use to reduce or prevent hemorrhage and reduce the need for replacement therapy during and following tooth extraction in hemophilia patients. Also has been administered orally† [off-label] or topically (as a mouthwash)† [off-label] in this setting.
Reduction in bleeding and need for therapeutic clotting concentrates demonstrated.
Prevention of Bleeding in Anticoagulated Patients Undergoing Dental Procedures
Has been used topically (as a mouthwash), orally, or IV to prevent perioperative bleeding in patients on anticoagulant therapy undergoing oral or dental procedures† [off-label].
Reduces bleeding when applied locally in patients receiving vitamin K antagonist therapy undergoing minor oral surgery or dental extraction.
Data are limited in patients receiving direct oral anticoagulants undergoing oral or dental procedures.
Heavy Menstrual Bleeding
Oral formulation FDA-labeled for treatment of cyclic heavy menstrual bleeding (i.e., menorrhagia). Prior to initiating therapy, manufacturer states that any underlying pathologies should be excluded.
Current evidence indicates that tranexamic acid is an effective nonsurgical treatment option in women with abnormal uterine bleeding presumed to be associated with endometrial dysfunction.
Clinically meaningful reductions in menstrual blood loss observed. Reduced limitations on social, leisure, and physical activities also reported.
Postpartum Hemorrhage
Has been used for prevention and treatment of postpartum hemorrhage† [off-label] (defined as blood loss >500 mL in the first 24 hours after delivery).
Mortality benefit demonstrated when used for treatment of postpartum hemorrhage. In the WOMAN study, tranexamic acid substantially reduced risk of death without increasing risk of thromboembolic events. Treatment effect was most pronounced when drug was administered within 3 hours of delivery; no apparent benefit was observed in risk of death due to bleeding when given after 3 hours.
Based on findings from the WOMAN trial, WHO strongly recommends early use of tranexamic acid (within 3 hours of birth) in addition to standard of care in women with clinically diagnosed postpartum hemorrhage following vaginal birth or cesarean section.
Evidence for the prevention of postpartum hemorrhage more limited.
Acute Trauma
Has been used to reduce bleeding in patients with acute trauma† [off-label].
Mortality benefit demonstrated in adult trauma patients in the CRASH-2 study. Early treatment (within 1 hour of trauma) associated with the greatest benefit; treatment after 3 hours appeared to increase risk of death due to bleeding.
Also has been used in pediatric trauma patients, but there is less experience. Some clinicians suggest that tranexamic acid may benefit pediatric patients in a similar manner as adults given the consistency in coagulation response to tissue injury across the age spectrum; however, additional study is required in the pediatric population.
Also has been used in patients with traumatic intracranial hemorrhage†. In the CRASH-3 study, administration of tranexamic acid within 3 hours of injury reduced risk of head injury-related death.
Surgery
Has been used to reduce perioperative blood loss and need for blood transfusions in patients undergoing elective or emergency surgery†.
Has been studied extensively in cardiac surgeries; shown to reduce risk of blood loss and transfusion without increasing thromboembolic events, but increased seizure risk observed. (See Seizures under Cautions.) Weigh benefits of drug against risk of seizures.
The Society of Thoracic Surgeons and the Society of Cardiovascular Anesthesiologists recommend use of tranexamic acid for blood conservation to reduce total blood loss and decrease the number of patients who require blood transfusion during cardiac procedures.
Also evaluated in numerous studies in patients undergoing orthopedic surgery. Based on the current evidence, some clinicians recommend use of tranexamic acid in all patients undergoing total hip arthroplasty who do not have contraindications.
Epistaxis
Has been used in the management of epistaxis†. However, many studies were conducted prior to the use of modern nasal cauterization and packing techniques; additional study is therefore needed in the setting of contemporary practice.
Hemoptysis
Has been used in the management of hemoptysis† caused by various etiologies. However, evidence to date is limited.
GI Bleeding
Has been used in the management of upper GI bleeding†. Some evidence suggests the drug may have a beneficial effect on mortality; however, additional studies are needed.
Tranexamic Acid Dosage and Administration
Administration
Administer orally or by slow IV injection or IV infusion. Also has been administered topically† (as a solution via irrigation, mouthwash, or gauze pad) for local application.
IV Administration
Commercially available in single-dose vials or ampules; discard any unused portions.
Can be mixed with most solutions for IV infusion such as electrolyte, carbohydrate, amino acid, and Dextran solutions. Heparin also can be added to the solution. Do not mix with blood or with solutions containing penicillin.
Rate of Administration
Administer tranexamic acid injection (100 mg/mL) by slow IV injection at a rate no faster than 1 mL/minute to avoid hypotension.
Standardize 4 Safety
Standardized concentrations for tranexamic acid have been established through Standardize 4 Safety (S4S), a national patient safety initiative to reduce medication errors, especially during transitions of care. Because recommendations from the S4S panels may differ from the manufacturer’s prescribing information, caution is advised when using concentrations that differ from labeling, particularly when using rate information from the label. For additional information on S4S (including updates that may be available), see [Web].
|
Patient Population |
Concentration Standards |
Dosing Units |
|---|---|---|
|
Pediatric patients (<50 kg) |
100 mg/mL (straight drug) |
mg/kg/hour |
Administration Precautions
Inadvertent intrathecal administration of tranexamic acid injection reported, in most cases resulting from erroneous administration of the drug instead of a local anesthetic (e.g., bupivacaine) intended for neuraxial anesthesia.
Inadvertent intrathecal injection of tranexamic acid can cause serious life-threatening injuries, including seizures, cardiac arrhythmias, paraplegia, permanent neurologic injury, and death. (See Seizures under Cautions.) Take special precautions (e.g., storage segregation, auxiliary warning labels, careful checking of container labels) to ensure that correct drug is selected and administered.
Oral Administration
Administer orally without regard to meals. Swallow tablets whole with liquids; do not chew or break.
Dosage
Pediatric Patients
Dental Procedures
Hemophilia Patients Undergoing Tooth Extraction
Oral†In children ≥1 year of age, tranexamic acid has been administered orally at a dosage of 20 mg/kg daily (in 2–3 divided doses).
IVData are limited in pediatric patients undergoing tooth extraction. According to manufacturer, the same dosage for adults can be used in pediatric patients.
In children ≥1 year of age, has been administered by slow IV injection using the 100-mg/mL concentration (rate of 1 mL/minute) at a dosage of 20 mg/kg daily (in 2–3 divided doses).
Topical†In children ≥1 year of age, has been administered topically (as a mouthwash) at a dosage of 20 mg/kg daily (in 2–3 divided doses).
Patients on Anticoagulant Therapy Undergoing Oral or Dental Procedures†
OralIn children ≥1 year of age, has been administered orally at a dosage of 20 mg/kg daily (in 2–3 divided doses).
IVIn children ≥1 year of age, has been administered by slow IV injection using the 100-mg/mL concentration (rate of 1 mL/minute) at a dosage of 20 mg/kg daily (in 2–3 divided doses).
TopicalIn children ≥1 year of age, has been administered topically (as a mouthwash) at a dosage of 20 mg/kg daily (in 2–3 divided doses).
Heavy Menstrual Bleeding
Oral
Adolescents: 1.3 g (two 650-mg tablets) 3 times daily for a maximum of 5 days during monthly menstruation. Do not exceed 3 doses (6 tablets) in a 24-hour period or administer for more than 5 days in any menstrual cycle.
Acute Trauma†
IV
Limited information in pediatric trauma patients. Some clinicians suggest that adult dosages may be used in children ≥12 years of age, and suggest an IV loading dose of 15 mg/kg (maximum of 1 g) followed by an IV infusion of 2 mg/kg per hour for at least 8 hours or until bleeding stops in children <12 years of age.
Adults
Dental Procedures
Hemophilia Patients Undergoing Tooth Extraction
Oral†Dosage of 1–1.5 g 2–3 times daily has been used.
IVManufacturer recommends a single IV dose of 10 mg/kg administered by slow IV injection (no faster than 1 mL/minute) immediately prior to the procedure. May be continued after extraction at a dosage of 10 mg/kg 3–4 times daily for ≤2–8 days.
IV dosage of 0.5–1 g 2–3 times daily also has been used.
Topical†Has been administered topically (as a mouthwash) at a dosage of 500 mg 4 times daily.
Patients on Anticoagulant Therapy Undergoing Oral or Dental Procedures†
IVHas been administered by slow IV injection using the 100-mg/mL concentration (rate of 1 mL/minute) at a dosage of 0.5–1 g 2–3 times daily. Optimum timing of administration and duration of therapy not known; usually initiated before the dental procedure and 3–4 times daily for 1–7 days after the procedure.
OralDosage of 1–1.5 g 2–3 times daily has been used. Optimum timing of administration and duration of therapy not known; usually initiated before the dental procedure and 3–4 times daily for 1–7 days after the procedure.
TopicalHas been administered topically (as a mouthwash) at a dosage of 500 mg 4 times daily. Optimum timing of administration and duration of therapy not known; usually administered before the dental procedure and 3–4 times daily for 1–7 days after the procedure.
Heavy Menstrual Bleeding
Oral
1.3 g (two 650-mg tablets) 3 times daily for a maximum of 5 days during monthly menstruation. Do not exceed 3 doses (6 tablets) in a 24-hour period or administer for more than 5 days in any menstrual cycle.
Postpartum Hemorrhage†
IV
In women with postpartum hemorrhage, dosage used in WOMAN trial recommended (loading dose of 1 g [100 mg/mL] by slow IV injection over an approximate rate of 1 mL/minute, with a second dose of 1 g given if bleeding continues after 30 minutes or recurs within 24 hours of the first dose).
Acute Trauma†
IV
Has been administered as an IV loading dose of 1 g (in 100 mL of 0.9% sodium chloride injection) over 10 minutes followed by IV infusion of 1 g over 8 hours; this regimen was used in the CRASH-2 study that showed significant reduction in mortality with tranexamic acid. Administer as early as possible (within 3 hours of injury) for greatest mortality benefit.
Cardiac Surgery†
IV
Optimal dosage not established; various dosage regimens have been used.
In clinical studies, IV loading dose ranged from 2.5–100 mg/kg and maintenance IV infusion ranged from 0.25–4 mg/kg per hour over 1–12 hours. It s recommended that dosage in cardiac surgery patients be limited to 30–50 mg/kg since higher dosages may increase risk of seizures.
Orthopedic Surgery†
IV
Optimal dosage and timing of administration not known; IV loading dose of 10–30 mg/kg with or without a maintenance IV infusion of 1 mg/kg per hour has been used; higher dosages may increase risk of seizures.
Prescribing Limits
Pediatric Patients
Oral
When used in adolescents for the treatment of heavy menstrual bleeding, do not exceed 3 doses in a 24-hour period and more than 5 days of treatment in any menstrual cycle.
Adults
Oral
When used for the treatment of heavy menstrual bleeding, do not exceed 3 doses in a 24-hour period and more than 5 days of treatment in any menstrual cycle.
Special Populations
Hepatic Impairment
No dosage adjustment needed.
Renal Impairment
IV Tranexamic Acid
The manufacturer recommends the following dosage adjustments in hemophilia patients with renal impairment receiving IV tranexamic acid for tooth extraction (see Table 2).
|
Serum Creatinine (mg/dL) |
Dosage of IV Tranexamic Acid |
|---|---|
|
1.36–2.83 |
10 mg/kg twice daily |
|
2.83–5.66 |
10 mg/kg daily |
|
>5.66 |
10 mg/kg every 48 hours or 5 mg/kg every 24 hours |
Oral Tranexamic Acid
The manufacturer recommends the following dosage adjustments in patients with renal impairment receiving oral tranexamic acid for the treatment of cyclic heavy menstrual bleeding (see Table 3).
|
Serum Creatinine (mg/dL) |
Dosage of Oral Tranexamic Acid |
|---|---|
|
>1.4 and ≤2.8 |
1.3 g twice daily for maximum of 5 days during menstruation |
|
>2.8 and ≤5.7 |
1.3 g once daily for maximum of 5 days during menstruation |
|
>5.7 |
650 mg once daily for maximum of 5 days during menstruation |
Geriatric Patients
Select dosage carefully. (See Geriatric Use under Cautions.)
Cautions for Tranexamic Acid
Contraindications
-
Patients with acquired defective color vision. (See Ocular Toxicity under Cautions.)
-
Patients with subarachnoid hemorrhage; cerebral edema and cerebral infarction may be caused by tranexamic acid in such patients.
-
Patients with active thromboembolic disease (e.g., DVT, PE, cerebral thrombosis, active intravascular clotting) or history or risk of thromboembolism (including retinal vein or artery occlusion).
-
Concomitant use with combination hormonal contraceptives.
-
Hypersensitivity reactions to tranexamic acid or any other ingredients in the formulation.
Warnings/Precautions
Thromboembolic Complications
Risk of thromboembolic events. (See Contraindications under Cautions.) Venous and arterial thrombosis (e.g., stroke, MI) reported; however, frequency not known since reported rates have differed in clinical studies and some studies did not adequately assess for these events.
Avoid concomitant use with drugs with prothrombotic properties (e.g., factor IX complex concentrates, anti-inhibitor coagulant concentrates, hormonal contraceptives). The manufacturer of tranexamic acid tablets states that concomitant use with combination hormonal contraceptives is contraindicated. Caution is advised if tranexamic acid is used concomitantly with tretinoin. (See Specific Drugs under Interactions.)
Retinal venous and arterial occlusion also reported. If any ocular or visual symptoms occur, immediately discontinue drug and refer patient to an ophthalmologist for further evaluation.
Seizures
Risk of dose-dependent seizures. Most often observed in the cardiac surgery setting where higher than recommended doses have been used.
Seizures also have occurred following accidental neuraxial administration of tranexamic acid, often resulting from container mix-ups with a local anesthetic intended for regional anesthesia. (See Administration Precautions under Dosage and Administration.) When given via the spinal route, tranexamic acid is a potent neurotoxin that can cause considerable harm.
To minimize risk of seizures, use lower dosages and adjust dosage appropriately, particularly in high-risk patients (e.g., those with renal impairment, older age, seizure disorders, or undergoing open procedures).
Monitor patients closely during surgery. Discontinue drug if seizures occur.
Hypersensitivity Reactions
Hypersensitivity reactions, including anaphylactic reactions, reported.
Use with caution in patients with known hypersensitivity to the drug. If a serious hypersensitivity reaction occurs, permanently discontinue tranexamic acid and administer appropriate treatment. (See Contraindications under Cautions.)
Ocular Toxicity
Although not observed in humans, focal areas of retinal degeneration observed in animals. Ligneous conjunctivitis also reported, which resolved following discontinuance of the drug.
If tranexamic acid therapy is expected to exceed 3 months, consider ophthalmic monitoring, including visual acuity and optical coherence tomography at regular intervals. Discontinue therapy if ophthalmological changes occur. One manufacturer states that the drug is contraindicated in patients with acquired defective color vision since this prohibits measurement of an end point that should be monitored for ocular toxicity.
Dizziness
May cause dizziness. Risk may be increased with concomitant use of other drugs that can also cause dizziness. (See Advice to Patients.)
Subarachnoid Hemorrhage
Manufacturer of the oral formulation states that cerebral edema and cerebral infarction may be caused by tranexamic acid in women with subarachnoid hemorrhage.
Specific Populations
Pregnancy
Not known whether tranexamic acid is associated with a risk of adverse maternal or fetal outcomes; however, the drug can cross the placenta. Consider potential risks to the fetus versus potential benefits of the drug.
No adequate and well-controlled studies in pregnant women. Fatal structural abnormalities reported in 2 cases when tranexamic acid used during conception or first trimester of pregnancy; however, not clear whether these effects were related to the drug or other factors. No evidence of adverse fetal or developmental outcomes in animal reproduction studies.
Lactation
Distributed into human milk. Effects on the breastfed infant or on milk production not known.
One manufacturer states that tranexamic acid should be used during lactation only when clearly needed. Consider known benefits of breast-feeding along with the mother's clinical need for tranexamic acid and potential adverse effects on the infant from the drug or underlying maternal condition.
Pediatric Use
Data limited on use in pediatric patients with hemophilia undergoing tooth extraction.
Oral tablet formulation may be used for treatment of heavy menstrual bleeding in adolescents; however, not intended for use in premenarchal girls.
Has been used for other indications in pediatric patients (e.g., cardiac surgery†, spinal surgery†, trauma†), although evidence more limited in children compared with adults.
The available information suggests no significant pharmacokinetic differences between adults and pediatric patients.
Adverse effects in children are rare, but can include GI effects, hypotension following rapid IV administration, muscle pain, and seizures with high doses during cardiac surgery.
Geriatric Use
Clinical studies of tranexamic acid injection did not include sufficient numbers of patients ≥65 years to determine whether they respond differently from younger patients. Other reported clinical experience has not identified differences in responses between geriatric and younger patients.
The drug is substantially excreted by the kidney. Because geriatric patients are more likely to have decreased renal function, select dosage carefully and consider monitoring renal function.
Hepatic Impairment
The effects of hepatic impairment not studied; however, only a small fraction of the drug is metabolized in the liver.
Renal Impairment
Principally eliminated by kidneys via glomerular filtration. Plasma concentrations may be increased in patients with renal impairment; use caution in such patients and reduce dosage appropriately. (See Renal Impairment under Dosage and Administration.)
Common Adverse Effects
IV tranexamic acid: Nausea, vomiting, diarrhea, allergic dermatitis, giddiness, hypotension, thromboembolic events.
Oral tranexamic acid: Headache, sinus and nasal symptoms, back pain, abdominal pain, musculoskeletal pain, joint pain, muscle cramps, migraine, anemia, fatigue.
Drug Interactions
Manufacturers state that no drug interaction studies have been conducted.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Factor IX complex and anti-inhibitor coagulant concentrates |
May increase thrombotic risk associated with tranexamic acid |
Avoid concomitant use |
|
Hormonal contraceptives |
May increase the thrombotic risk associated with tranexamic acid |
Avoid concomitant use; use alternative (nonhormonal) forms of contraception |
|
Tissue plasminogen activators |
May decrease efficacy of both drugs |
Caution is advised |
|
Tretinoin |
Possible exacerbation of the procoagulant effects of tretinoin Deaths due to thrombotic complications have occurred in patients with acute promyelocytic leukemia who received oral tretinoin and tranexamic acid concomitantly |
Caution is advised |
Tranexamic Acid Pharmacokinetics
Absorption
Plasma Concentrations
Following oral administration, peak plasma concentrations are obtained in approximately 3 hours.
Bioavailability
Absolute bioavailability following oral administration is approximately 45%.
Food
Food does not appear to affect time to peak plasma concentrations.
Special Populations
Plasma concentrations are increased in patients with renal impairment; degree of increase is directly correlated with severity of impairment.
Distribution
Plasma Protein Binding
3% with no apparent binding to albumin.
Elimination
Metabolism
Only a small fraction of the drug is metabolized.
Elimination Route
Eliminated principally by urinary excretion via glomerular filtration; more than 95% of a dose is excreted as unchanged drug.
Half-life
Mean terminal half-life of orally administered tranexamic acid is about 11 hours.
Following IV administration, apparent elimination half-life is approximately 2 hours.
Stability
Storage
Oral
Tablets
25°C (may be exposed to 15–30°C).
Parenteral
Injection
20–25°C (may be exposed to 15–30°C).
Diluted solutions may be stored up to 4 hours at room temperature.
Actions
-
Synthetic lysine derivative that acts as an antifibrinolytic agent; reduces bleeding by preventing the breakdown of fibrin clots.
-
Blocks lysine binding sites of plasminogen; inhibits fibrin binding to plasminogen, resulting in preservation and stabilization of fibrin matrix structure.
-
Binding affinity of tranexamic acid to plasminogen and plasmin is about 6–10 times more potent than aminocaproic acid.
Advice to Patients
-
Importance of instructing patients on proper administration of tranexamic acid and advising them to read the manufacturer's patient information carefully.
-
Inform patients that tranexamic acid may increase the risk of venous and arterial thrombosis or thromboembolism and to contact their clinician if any signs or symptoms suggestive of thromboembolism occur.
-
Advise patients using hormonal contraception that combined use with tranexamic acid may increase the risk for thromboembolic adverse reactions and to use effective alternative (nonhormonal) contraception during therapy with tranexamic acid.
-
Inform patients that tranexamic acid may cause seizures and to contact their clinician if any signs or symptoms suggestive of seizures occur.
-
Inform patients that tranexamic acid may cause hypersensitivity reactions and to immediately discontinue the drug and contact their clinician if any signs or symptoms of a severe allergic reaction (e.g., shortness of breath, tightening of the throat) occur.
-
Inform patients that tranexamic acid can cause visual disturbance and that they should report any eye symptoms or changes in their vision to their clinician and to follow-up with an ophthalmologist for a complete evaluation, including dilated retinal examination of the retina.
-
Risk of dizziness; caution patients about driving, operating machinery, or performing hazardous tasks while taking the drug.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as any concomitant illnesses.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
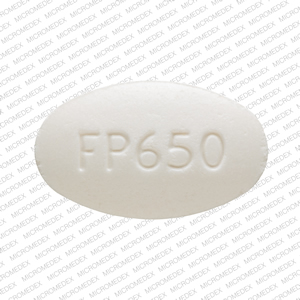
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
650 mg* |
Lysteda |
Ferring |
|
Tranexamic Acid Tablets |
||||
|
Parenteral |
Injection |
100 mg/mL* |
Cyklokapron |
Pfizer |
|
Tranexamic Acid Injection |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
More about tranexamic acid
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (281)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: miscellaneous coagulation modifiers
- Breastfeeding