Tolcapone (Monograph)
Brand name: Tasmar
Drug class: Catechol-O-Methyltransferase (COMT) Inhibitors
- Antiparkinsonian Agents
VA class: CN500
Chemical name: (3,4-Dihydroxy-5-nitrophenyl)(4-methylphenyl)-methanone
Molecular formula: C14H11NO5
CAS number: 134308-13-7
Warning
-
Tolcapone should not be initiated until the clinician has fully explained the risks and the patient (or representative) has provided written acknowledgment that the risks have been explained.1
-
Use with caution in patients with severe dystonia or dyskinesia.1 (See Rhabdomyolysis under Cautions.)
- Hepatotoxicity
-
Risk of potentially fatal, acute fulminant hepatic failure.1 30 31 32 Incidence may be 10- to 100-fold higher than the background incidence in the general population.1 32
-
Generally reserve tolcapone therapy for patients with parkinsonian syndrome receiving levodopa/carbidopa who are experiencing symptom fluctuations and are not responding adequately to or are not candidates for other adjunctive therapies (e.g., ergot- and nonergot-derivative dopamine receptor agonists, selegiline).1 30 31 32
-
Do not initiate tolcapone in patients with clinical evidence of active liver disease, ALT or AST concentrations exceeding the ULN, or any other evidence of hepatocellular dysfunction.1
-
Discontinue tolcapone if the patient does not experience symptomatic improvement within 3 weeks of initiating therapy.1
-
Discontinue tolcapone if aminotransferase concentrations exceed the ULN or if clinical manifestations suggest the onset of hepatic failure (e.g., persistent nausea, fatigue, lethargy, anorexia, jaundice, dark urine, pruritus, upper right quadrant tenderness).1
-
Advise patients of the need for self-monitoring for signs or symptoms of liver disease.1
-
Patients who develop evidence of hepatocellular injury while receiving tolcapone and in whom such therapy is discontinued for any reason may be at increased risk for hepatic injury if tolcapone is reintroduced.1 Retreatment with tolcapone ordinarily should not be considered in such patients.1
-
Perform appropriate tests to exclude hepatic disease prior to initiation of therapy1 and monitor patients receiving tolcapone for evidence of emergent liver injury.1
-
Evaluate serum AST and ALT at baseline, every 2 weeks during the first year of therapy, every 4 weeks during the next 6 months of therapy, and every 8 weeks thereafter.1 If dosage is increased to 200 mg 3 times daily, determine serum AST and ALT prior to increasing the dosage and then at the same frequency as that recommended when therapy is initiated.1
-
Not known whether baseline and periodic monitoring of liver enzymes will prevent the occurrence of fulminant tolcapone-induced hepatic failure; however, frequent laboratory monitoring for evidence of hepatocellular injury is considered essential.1 Early detection of drug-induced hepatic injury along with immediate discontinuance of the suspect drug is believed to enhance the likelihood for recovery.1 Baseline monitoring is recommended, since patients with preexisting liver disease may be more vulnerable to hepatotoxins.1
Introduction
Reversible catechol-O-methyltransferase (COMT) inhibitor.1 2 3 4 5 6 7 8 9 10 12 13 14 15 16 17 18 19 28
Uses for Tolcapone
Parkinsonian Syndrome
Adjunct to levodopa/carbidopa therapy for the symptomatic treatment of idiopathic parkinson disease; concomitant administration of tolcapone with levodopa and a decarboxylase inhibitor results in more sustained plasma levodopa concentrations compared with administration of levodopa and a decarboxylase inhibitor.1 2 3 4 5 6 7 8 9 10 12 13 14 15 16 17 18 19 23 26 28
Generally reserve therapy for patients with parkinson disease receiving levodopa/carbidopa who are experiencing symptom fluctuations and are not responding adequately to or are not candidates for other adjunctive therapies (e.g., dopamine receptor agonists, selective MAO-B inhibitors).1 31 32 (See Boxed Warning.)
Tolcapone Dosage and Administration
General
-
Symptomatic improvement generally is evident within 3 weeks following initiation of tolcapone.1 7 Discontinue tolcapone if the patient fails to show symptomatic improvement within 3 weeks of initiating therapy.1 (See Boxed Warning.)
- Concomitant Levodopa/Carbidopa Therapy
-
Administer in conjunction with levodopa/carbidopa (conventional or extended-release preparations).1 9
-
To optimize patient response, reductions in the daily levodopa/carbidopa dosage may be necessary.1 6 7 9 16 28 In clinical trials, most patients receiving levodopa dosages >600 mg daily or with moderate to severe dyskinesia prior to initiation of tolcapone required reduction of levodopa dosage (average reduction: about 30%).1 6 7 9 16 23
- Discontinuance of Tolcapone
-
Discontinuance or abrupt dosage reduction may lead to reemergence of signs and symptoms of parkinson disease or a symptom complex resembling neuroleptic malignant syndrome (e.g., hyperpyrexia, confusion).1
-
If tolcapone is discontinued, monitor the patient closely and adjust the dosage of dopaminergic therapy, if needed.1
-
If hyperpyrexia or severe rigidity occurs following drug discontinuance, the differential diagnosis should include the possibility of a symptom complex resembling neuroleptic malignant syndrome.1
-
Tapering the dosage of tolcapone has not been systematically evaluated;1 however, reducing the frequency to twice or once daily prior to discontinuance may not prevent these events, since the duration of COMT inhibition associated with tolcapone therapy is 5–6 hours or longer.1 2 4 5 8
Administration
Oral Administration
Administer orally in 3 equally divided doses daily1 6 7 9 16 23 28 without regard to meals.1
In clinical studies, the first dose of the day was administered together with the first dose of the day of levodopa/carbidopa; subsequent doses of tolcapone are administered 6 and 12 hours later.1 6 7 9 28
Dosage
Adults
Parkinsonian Syndrome
Oral
Usual dosage: 100 mg 3 times daily.1 28
Reserve higher dosage (200 mg 3 times daily) for situations when the anticipated incremental benefit is justified.1 If the patient fails to show the expected clinical benefit while receiving 200 mg 3 times daily for 3 weeks, discontinue the drug.1 (See Hepatic Effects under Cautions.)
Special Populations
Renal Impairment
Dosage adjustment not required in patients with mild to moderate renal impairment (Clcr >30 mL/minute).1 Safety not evaluated in patients with Clcr <25 mL/minute.1
Cautions for Tolcapone
Contraindications
-
Liver disease.1
-
Patients in whom tolcapone was discontinued because of evidence of tolcapone-induced hepatocellular injury.1
-
History of nontraumatic rhabdomyolysis.1
-
History of drug-related hyperpyrexia and confusion.1
-
Known hypersensitivity to tolcapone or any ingredient in the formulation.1
Warnings/Precautions
Warnings
Hepatic Effects
Risk of potentially fatal, acute fulminant hepatic failure.1 30 31 32 (See Boxed Warning.)
Increases in ALT reported more frequently in patients receiving tolcapone 200 mg 3 times daily than in those receiving 100 mg 3 times daily; not known whether the risk of fulminant hepatic failure is increased in patients receiving the higher dosage.1
Frequency of aminotransferase elevations greater in women than men.1
In clinical studies, aminotransferase elevations generally occurred 6 weeks to 6 months following initiation of therapy; concentrations generally returned to baseline within 1–3 months in about 50% of patients who continued tolcapone therapy and within 2–3 weeks up to 1–2 months in patients who discontinued the drug.1 7 16 However, rapid deterioration30 and death1 30 31 32 can occur despite drug discontinuance.30
MAO Inhibitors
Concomitant administration with a nonselective MAO inhibitor (e.g., phenelzine, tranylcypromine) could result in inhibition of the 2 principal pathways of catecholamine metabolism (i.e., metabolism by COMT and MAO1 2 3 4 5 6 7 8 9 10 13 ).1 Avoid concomitant administration with a nonselective MAO inhibitor;1 28 may administer tolcapone concomitantly with a selective inhibitor of MAO-B (e.g., selegiline).1 19 (See Interactions.)
Falling Asleep During Activities of Daily Living
Episodes of falling asleep while engaged in activities of daily living (e.g., driving) have occurred with levodopa, and tolcapone increases plasma concentrations of levodopa; these episodes have sometimes resulted in accidents.1 Some patients perceived no warning signs (e.g., excessive drowsiness) and believed they were alert immediately prior to the event.1
Falling asleep while engaged in such activities usually occurs in the setting of preexisting somnolence, although patients may not give such a history.1
Continually reassess patients for drowsiness or sleepiness during therapy.1 Patients may not acknowledge drowsiness or sleepiness until directly questioned about such adverse effects during specific activities.1 Ask patients about any factors that may increase the risk of somnolence (e.g., concomitant use of sedating drugs, presence of sleep disorders).1
Consider discontinuing therapy if a patient develops daytime sleepiness or episodes of falling asleep during activities that require active participation (e.g., conversations, eating).1 If the drug is continued, advise patient not to drive and to avoid other potentially dangerous activities.1 (See Advice to Patients.) Insufficient information to establish whether dosage reduction will eliminate this adverse event.1
General Precautions
Orthostatic Hypotension and Syncope
Increased occurrence of orthostatic instability1 2 3 6 10 13 15 16 in patients receiving tolcapone in combination with levodopa and a decarboxylase inhibitor relative to patients receiving levodopa and a decarboxylase inhibitor (17 versus 14%).1 16 Mechanism not fully established, but an increase would be expected because dopaminergic therapy in patients with parkinsonian syndrome is associated with orthostatic hypotension and tolcapone increases systemic exposure to levodopa.1
Orthostatic hypotension usually is asymptomatic;1 however, patients with orthostatic instability at baseline are more likely than patients without symptoms to experience orthostatic hypotension.1 No apparent increase in the incidence of orthostatic hypotension in patients receiving a dopamine agonist or selegiline at baseline.1 19
Possible syncope;1 reported more frequently in patients who had an episode of documented hypotension than in those who did not have an episode of documented hypotension.1
Diarrhea
Possible diarrhea,1 2 4 5 7 9 15 16 generally mild to moderate1 7 but can be severe and result in hospitalization.1
Generally occurs during the first 6–12 weeks of therapy but may occur as early as 2 weeks or as late as several months following initiation of therapy.1 7 16
Frequently is associated with anorexia, is dose related, and resolves with continued therapy or following drug discontinuance.1 7 15 16
Patients experiencing persistent diarrhea should be evaluated by appropriate clinical and laboratory studies, including fecal occult blood studies.1
Hallucinations and Psychotic-like Behavior
Hallucinations1 6 9 10 13 15 16 reported in 8–10% of patients receiving tolcapone in clinical studies, required hospitalization in up to 1.7% of patients, and resulted in drug discontinuance in 1–1.4% of patients.1 9 15
Hallucinations generally occur within first 2 weeks of therapy; are commonly accompanied by confusion and, less commonly, insomnia and excessive dreaming; and occur more frequently in patients ≥75 years of age.1
During postmarketing experience, other new or worsening mental status and behavioral changes (e.g., paranoid ideation, delusions, hallucinations, confusion, psychotic-like behavior, disorientation, aggressive behavior, agitation, delirium) reported during therapy or after initiating or increasing dosage.1 Other antiparkinsonian agents can produce similar effects.1
Dyskinesia
Addition of tolcapone may exacerbate levodopa-associated dyskinesias.1 2 6 7 9 15 16 26 Usually occurs within 24 hours after initiating tolcapone and is controlled by reducing the levodopa dosage by 20–30%.1 2 6 7 9 16 26 However, some patients continue to experience frequent dyskinesias after reduction of levodopa dosage.1
Impulse Control/Compulsive Behaviors
Intense urges and compulsive behaviors (e.g., urge to gamble, increased sexual urges, binge eating, uncontrolled spending, other intense urges) and the inability to control these urges reported in patients receiving tolcapone in conjunction with levodopa/carbidopa and other dopaminergic agents.1 These urges stopped in some cases when dosage was reduced or the drug was discontinued.1
If a patient develops any such behaviors while receiving tolcapone, consider reducing dosage or discontinuing therapy.1 (See Advice to Patients.)
Rhabdomyolysis
Severe rhabdomyolysis,1 including multiorgan system failure progressing to death, reported rarely.1 Causal relationship not established.1
Severe, prolonged motor activity (e.g., dyskinesia) may account for rhabdomyolysis; however, some cases included fever, altered consciousness, and muscular rigidity and resembled neuroleptic malignant syndrome.1
Use with caution in patients with severe dystonia or dyskinesia.1
Renal Effects
High incidence of proximal tubule cell damage (degeneration, single cell necrosis, hyperplasia, karyocytomegaly, atypical nuclei) in rats receiving tolcapone for 1 or 2 years at dosages ≥6 times the recommended human dosage; not associated with changes in clinical chemistry values.1 No established method for monitoring for occurrence of such lesions in humans.1 Species-specific mechanism postulated, but studies to confirm this theory not conducted.1
Neuroleptic Malignant Syndrome
Neuroleptic malignant syndrome has occurred in patients receiving psychotherapeutic agents and in patients with parkinson disease during withdrawal of dopaminergic agents.20
Symptom complex resembling neuroleptic malignant syndrome (elevated temperature, muscular rigidity, altered consciousness) reported rarely in association with abrupt withdrawal or dosage reduction of tolcapone.1 28 Creatine kinase concentrations may be increased.1 (See Discontinuance of Tolcapone under Dosage and Administration.)
Fibrosis
Retroperitoneal fibrosis, pulmonary infiltrates, pleural effusion, and thickening of pleura reported in patients receiving ergot-derivative dopamine receptor agonists (e.g., bromocriptine, pergolide);1 presumably related to the ergoline structure of these agents.1 However, consider the possibility that non-ergot-derived drugs that increase dopaminergic activity (e.g., tolcapone) may induce similar changes.1
Specific Populations
Pregnancy
Category C.1
Lactation
Distributed into milk in rats; not known whether distributed into human milk.1 Use with caution in nursing women.1
Pediatric Use
Safety and efficacy not established.1 No identified potential use in children.1
Geriatric Use
Safety and efficacy in geriatric patients have not been studied specifically to date; however, parkinson disease, for which safety and efficacy have been established, occurs principally in patients >50 years of age.1 6 7 8 9 Patients ≥75 years of age may be more likely to develop hallucinations but less likely to develop dystonia than younger patients.1
No evidence of age-related differences in tolcapone pharmacokinetics.1 4 5
Hepatic Impairment
Do not initiate therapy in patients with clinical evidence of active liver disease, ALT or AST concentrations exceeding the ULN, or any other evidence of hepatocellular dysfunction.1
Renal Impairment
Use with caution in patients with severe renal impairment.1
Common Adverse Effects
Many CNS and psychiatric disturbances in patients receiving tolcapone in conjunction with levodopa are likely to result from increased levodopa concentrations and CNS bioavailability induced by tolcapone.1 7 9 16 24 33
Dyskinesia, dystonia, nausea, anorexia, sleep disturbances/insomnia, orthostatic instability, muscle cramping, excessive dreaming, somnolence; these are dopaminergic effects associated with levodopa therapy.7 9 15 16 28 Most frequent nondopaminergic adverse effect: diarrhea.7 9 15 16 28 29
Drug Interactions
Metabolized in part by COMT1 2 27 28 and by CYP3A4 and CYP2A6.1 28
Inhibits COMT; has affinity for CYP2C9 in vitro.1 20
Drugs Metabolized by Hepatic Microsomal Enzymes
Clinically important interactions with drugs metabolized by CYP2C9 and CYP2D6 are not expected to occur.1 In vitro studies did not reveal important interactions with substrates for CYP isoenzymes 2A6, 1A2, 3A4, 2C19, or 2D6.1
Drugs Metabolized by COMT
Tolcapone may alter the metabolism of drugs metabolized by COMT.1
Drugs Affecting CNS Monoaminergic or Cholinergic System
Symptom complex resembling neuroleptic malignant syndrome reported in patients receiving tolcapone in combination with other drugs that affect brain monoaminergic or anticholinergic systems; caution is advised if such combinations are used.1
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Antidepressants, SSRIs |
Symptom complex resembling neuroleptic malignant syndrome reported in patients receiving tolcapone in combination with other drugs that affect brain monoaminergic systems1 |
Caution advised if such combinations are used1 |
|
Antidepressants, tricyclics |
Symptom complex resembling neuroleptic malignant syndrome reported in patients receiving tolcapone in combination with other drugs that affect brain monoaminergic systems1 No alteration of desipramine pharmacokinetics; however, regimens that include tolcapone, levodopa/carbidopa, and desipramine are not tolerated as well as regimens that do not include desipramine1 |
Caution advised if such combinations are used1 |
|
Antipsychotic agents |
Possible exacerbation of parkinsonian symptoms; may result in decreased efficacy of tolcapone1 |
|
|
Carbidopa |
No alteration of carbidopa pharmacokinetics1 |
|
|
Catecholamines (methyldopa, dobutamine, apomorphine, isoproterenol) |
||
|
CNS depressants |
Possible additive sedative effects1 |
|
|
Ephedrine |
No apparent change in tolerability of ephedrine (hemodynamic parameters or plasma catecholamine concentrations at rest or during exercise)1 |
Can administer concomitantly1 |
|
Levodopa |
Levodopa AUC increased 2-fold and half-life increased from 2 hours to 3.5 hours without an increase in peak plasma levodopa concentration or a change in the time to peak plasma concentration; the result is more stable plasma levodopa concentrations and enhanced clinical efficacy1 2 3 4 5 6 7 8 9 10 12 13 14 15 16 17 18 19 26 |
Used for therapeutic effect1 2 3 4 5 6 7 8 9 10 12 13 14 15 16 17 18 19 26 |
|
MAO inhibitors, nonselective (e.g., phenelzine, tranylcypromine) |
Possible inhibition of the principal pathways of catecholamine metabolism1 28 Symptom complex resembling neuroleptic malignant syndrome reported in patients receiving tolcapone in combination with other drugs that affect brain monoaminergic systems1 |
|
|
MAO-B inhibitors, selective (e.g., selegiline) |
Adverse effect profile associated with regimens that include tolcapone, levodopa/carbidopa, and selegiline is similar to that associated with regimens that do not include selegiline1 19 |
|
|
Phenytoin |
No displacement of phenytoin from protein binding sites in vitro1 |
|
|
Tolbutamide |
No effect on tolbutamide pharmacokinetics; no displacement of tolbutamide from protein binding sites in vitro1 |
|
|
Warfarin |
Possible increased plasma warfarin concentrations;1 28 33 no displacement of warfarin from protein binding sites in vitro1 |
Determine PT and INR frequently and adjust dosage, if needed1 28 33 |
Tolcapone Pharmacokinetics
Absorption
Bioavailability
Absolute bioavailability following oral administration is about 65–68%.1 27
Rapidly absorbed following oral administration, with peak plasma concentrations generally attained within 2 hours.1 2 3 4 5 8 14 27 28
Onset
Maximum inhibition of erythrocyte COMT activity is achieved within 1 hour and exceeds 80% following a single oral 200-mg dose in healthy individuals;1 2 4 5 8 maximum inhibition is about 80% following administration of 200 mg 3 times daily for 7 days.1 8
Duration
COMT inhibitory activity persists for 16–24 hours following a single oral 200-mg dose in healthy individuals;1 2 4 5 8 inhibition at trough tolcapone concentrations is 30–45% following administration of 200 mg 3 times daily for 7 days.1 8
Food
Administration within 1 hour before or 2 hours after a meal reduces bioavailability by 10–20% compared with administration in the fasting state.1
Distribution
Extent
Distribution into body tissues and fluids is not fully characterized;1 33 however, the drug is not widely distributed.1 2 13
Distributes into brain tissue.1 2 13
Distributes into milk in rats; not known whether tolcapone distributes into human milk.1
Plasma Protein Binding
>99.9% (principally albumin).1 27
Special Populations
In patients with moderate cirrhotic liver disease (Child-Pugh class B), volume of distribution of unbound tolcapone is reduced almost 50%.1 27
Elimination
Metabolism
Extensively metabolized by a variety of mechanisms:1 27 28 glucuronidation (principal metabolic pathway),1 27 28 metabolism by COMT to catechol-3-O-methyltolcapone,1 2 27 28 hydroxylation followed by oxidation to a carboxylic acid derivative,1 28 and reduction followed by N-acetylation.1 In vitro data indicate that CYP3A4 and CYP2A6 catalyze the oxidation reaction.1 28
Elimination Route
Excreted in urine (60%) and feces (40%);1 minimally excreted in urine as unchanged drug (<0.5%).1 27
Half-life
Terminal elimination half-life of tolcapone: 2–3 hours.2 3 4 5 8 27 28
Terminal elimination half-life of catechol-3-O-methyltolcapone: 30–60 hours (but does not appear to accumulate with multiple dosing because tolcapone inhibits COMT).2 3 4 5 8 27
Special Populations
In patients with moderate cirrhotic liver disease (Child-Pugh class B), clearance of unbound tolcapone reduced almost 50%.1 27
In patients with Clcr of 30–130 mL/minute, pharmacokinetics not altered.1
No evidence of gender-, age-, or weight-related pharmacokinetic differences.1 4 5
Stability
Storage
Oral
Tablets
Tight containers at 20–25°C.1
Actions
-
Selective, potent, peripheral and to a lesser extent central, reversible inhibitor of COMT.1 2 3 4 5 6 7 8 9 10 12 13 14 15 16 17 18 19 23 26 28
-
Lacks antiparkinsonian effects when administered as monotherapy.
-
Is believed to act principally by inhibiting COMT in peripheral tissues and altering the plasma pharmacokinetics of levodopa, resulting in more sustained plasma levodopa concentrations (see Specific Drugs under Interactions).1 2 3 4 5 6 7 8 9 10 12 13 14 15 16 17 18 19 23 26 28 When levodopa is administered concomitantly with a decarboxylase inhibitor (e.g., carbidopa), COMT is the major enzyme catalyzing the metabolism of levodopa to 3-methoxy-4-hydroxy-l-phenylalanine (3-OMD).1 2 3 4 5 6 7 8 9 10 12 13 14 15 16 17 18 19
-
Reductions in circulating 3-OMD that result from decreased peripheral metabolism of levodopa may increase distribution of levodopa into the CNS by reducing the competitive substrate (3-OMD) for transport mechanisms.26
Advice to Patients
-
Risk of hepatic toxicity.1 Necessity of laboratory monitoring of liver enzymes.1 Importance of contacting clinician immediately if signs or symptoms suggestive of hepatic failure (e.g., clay-colored stools, jaundice, fatigue, loss of appetite, lethargy) occur.1
-
Potential for tolcapone to exacerbate levodopa-associated adverse effects (e.g., dyskinesias, dystonia).1 7 9 16
-
Risk of orthostatic hypotension with or without symptoms (e.g., dizziness, nausea, syncope, sweating).1 Avoid rising rapidly after prolonged sitting or lying down, especially during the first few weeks of therapy.1
-
Possible occurrence of hallucinations.1
-
Importance of advising patients of the potential for sedating effects, including somnolence and the possibility of falling asleep while engaged in activities of daily living.1 Patients should avoid driving, operating machinery, or engaging in other potentially dangerous activities until effects on the individual are known.1 Importance of advising patients that if increased somnolence or episodes of falling asleep during activities of daily living (e.g., conversations, eating, driving) occur at any time during therapy, they should not drive or participate in potentially dangerous activities until they have contacted their clinician.1
-
Importance of asking patients whether they have developed any new or increased urges or compulsive behaviors (e.g., gambling urges, sexual urges, uncontrolled spending, binge eating) while receiving tolcapone and of advising them of the importance of reporting such urges.1
-
Risk of nausea, especially during the first 3 months of therapy.1
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.1
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses (e.g., liver disease).1
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
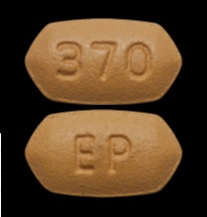
Oral |
Tablets, film-coated |
100 mg* |
Tasmar |
Valeant |
|
Tolcapone Tablets |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions May 24, 2021. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
References
1. Valeant Pharmaceuticals. Tasmar (tolcapone) tablets prescribing information. Bridgewater, NJ; 2018 Dec.
2. Gottwald MD, Bainbridge JL, Dowling GA et al. New pharmacotherapy for Parkinson’s disease. Ann Pharmacother. 1997; 31:1205-17. https://pubmed.ncbi.nlm.nih.gov/9337447
3. Dingemanse J, Jorga K, Zürcher G et al. Pharmacokinetic-pharmacodynamic interaction between the COMT inhibitor tolcapone and single-dose levodopa. Br J Clin Pharmacol. 1995; 40:253-62. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1365105/ https://pubmed.ncbi.nlm.nih.gov/8527287
4. Dingemanse J, Jorga KM, Schmitt M et al. Integrated pharmacokinetics and pharmacodynamics of the novel catechol-O-methyltransferase inhibitor tolcapone during first administration to humans. Clin Pharmacol Ther. 1995; 57:508-17. https://pubmed.ncbi.nlm.nih.gov/7768073
5. Dingemanse J, Jorga K, Zürcher G et al. Multiple-dose clinical pharmacology of the catechol-O-methyl-transferase inhibitor tolcapone in elderly subjects. Eur J Clin Pharmacol. 1996; 50:47-55. https://pubmed.ncbi.nlm.nih.gov/8739811
6. Kurth MC, Adler CH, St Hilaire M et al et al. Tolcapone improves motor function and reduces levodopa requirement in patients with Parkinson’s disease experiencing motor fluctuations: a multicenter, double-blind, randomized, placebo-controlled trial. Neurology. 1997; 48:81-7. https://pubmed.ncbi.nlm.nih.gov/9008498
7. Waters CH, Kurth M, Bailey P et al et al. Tolcapone in stable Parkinson’s disease: efficacy and safety of long-term treatment. Neurology. 1997; 49: 665-71. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2730601/
8. Jorga KM, Sedek G, Fotteler B et al. Optimizing levodopa pharmacokinetics with multiple tolcapone doses in the elderly. Clin Pharmacol Ther. 1997; 62:300-10. https://pubmed.ncbi.nlm.nih.gov/9333106
9. Rajput AH, Martin W, Saint-Hilaire MH et al. Tolcapone improves motor function in parkinsonian patients with the “wearing-off” phenomenon: a double-blind, placebo-controlled, multicenter trial. Neurology. 1997; 49:1066-71. https://pubmed.ncbi.nlm.nih.gov/9339691
10. Agid Y, Destée A, Durif F et al et al. Tolcapone, bromocriptine, and Parkinson’s disease. Lancet. 1997; 350:712-3. https://pubmed.ncbi.nlm.nih.gov/9291909
11. Catechol O-methyltransferase. In: Dorland’s illustrated medical dictionary. 28th ed. Philadlephia, PA: W.B. Saunders Co; 1994:278.
12. Byrne JM, Tipton KF. Nitrocatechol derivatives as inhibitors of catechol-O- methyltransferase. Biochem Soc Trans. 1996; 24:64S. https://pubmed.ncbi.nlm.nih.gov/8674740
13. Kaakkola S, Gordin A, Männistö PT. General properties and clinical possibilities of new selective inhibitors of catechol O-methyltransferase. Gen Pharmacol. 1994; 25:813-24. https://pubmed.ncbi.nlm.nih.gov/7835624
14. Sedek G, Jorga K, Schmitt M et al. Effect of tolcapone on plasma levodopa concentrations after coadministration with levodopa/carbidopa to healthy volunteers. Clin Neuropharmacol. 1997; 20:531-41. https://pubmed.ncbi.nlm.nih.gov/9403227
15. Dupont E, Burgunder JM, Findley LJ et al et al. Tolcapone added to levodopa in stable parkinsonian patients: a double-blind placebo-controlled study. Mov Disord. 1997; 12:928-34. https://pubmed.ncbi.nlm.nih.gov/9399217
16. Baas H, Beiske AG, Ghika J et al. Catechol-O-methyltransferase inhibition with tolcapone reduces the “wearing off” phenomenon and levodopa requirements in fluctuating parkinsonian patients. J Neurol Neurosurg Psychiatry. 1997; 63:421-8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2169755/ https://pubmed.ncbi.nlm.nih.gov/9343116
17. Männistö PT. Catechol O-methyltransferase: characterization of the protein, its gene, and the preclinical pharmacology of COMT inhibitors. Adv Pharmacol. 1998; 42:324-8. https://pubmed.ncbi.nlm.nih.gov/9327906
18. Zürcher G, Dingemanse J, Da Prada M. Potent COMT inhibition by Ro 40-7592 in the periphery and in the brain: preclinical and clinical findings. Adv Neurol. 1993; 60:641-7. https://pubmed.ncbi.nlm.nih.gov/8420203
19. Davis TL, Roznoski M, Burns RS. Effects of tolcapone in Parkinson’s patients takingl-dihydroxyphenylalanine/carbidopa and selegiline. Mov Disord. 1995; 10:349- 51. https://pubmed.ncbi.nlm.nih.gov/7651456
20. Keyser DL, Rodnitzky RL. Neuroleptic malignant syndrome in Parkinson’s disease after withdrawal or alteration of dopaminergic therapy. Arch Intern Med. 1991; 151:794- 6. https://pubmed.ncbi.nlm.nih.gov/1672810
21. Slaughter RL, Edwards DJ. Recent advances: the cytochrome P450 enzymes. Ann Pharmacother. 1995; 29:619-24. https://pubmed.ncbi.nlm.nih.gov/7663035
22. Gasparini M, Fabrizio E, Bonifati V et al. Cognitive improvement during tolcapone treatment in Parkinson’s disease. J Neural Transm. 1997; 104:887-94. https://pubmed.ncbi.nlm.nih.gov/9451720
23. Nutt JG. Catechol-O-methyltransferase inhibitors for treatment of Parkinson’s disease. Lancet. 1998; 351:1221-22. https://pubmed.ncbi.nlm.nih.gov/9643737
24. Henry C, Wilson JA. Catechol-O-methyltransferase inhibitors in Parkinson’s disease. Lancet. 1998; 351:1965-66. https://pubmed.ncbi.nlm.nih.gov/9654299
25. Xie T, Ho SL. Catechol-O-methyltransferase inhibitors in Parkinson’s disease. Lancet. 1998; 351:1966. https://pubmed.ncbi.nlm.nih.gov/9654300
26. Olanow CW, Watts Rl, Koller WC. An algorithm (decision tree) for the management of Parkinson’s disease (2001): treatment guidelines. Neurology. 2001; 56:S1-S88.
27. Jorga KM, Kroodsma JM, Fotteler B, et al. Effect of liver impairment on the pharmacokinetics of tolcapone and its metabolites. Clin Pharmacol Ther. 1998;63:646- 54.
28. Anon. Tolcapone for Parkinson’s disease. Med Lett Drugs Ther. 1998; 40:60- 61. https://pubmed.ncbi.nlm.nih.gov/9629124
29. Lang AE, Lozano AM. Parkinson’s disease: second of two parts. N Engl J Med. 1998; 339:1130-1143. https://pubmed.ncbi.nlm.nih.gov/9770561
30. Assal F, Spahr L, Hadengue A et al. Tolcapone and fulminant hepatitis. Lancet. 1998; 352:958. https://pubmed.ncbi.nlm.nih.gov/9752821
31. Anon. New warnings for Parkinson’s drug, Tasmar. FDA Talk Paper. Rockville, MD: Food and Drug Administration; 1998 Nov. 16.
32. Ellison RH. Dear health professional letter regarding appropriate use of Tasmar. Nutley, NJ: Roche Laboratories; 1998 Nov. 16.
33. Reviewers’ comments (personal observations).
Related/similar drugs
More about tolcapone
- Check interactions
- Compare alternatives
- Pricing & coupons
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: dopaminergic antiparkinsonism agents
- Breastfeeding
- En español