Sulfadiazine (Monograph)
Drug class: Sulfonamides
VA class: AM650
Chemical name: N1-2-pyrimidinylsulfanilamide
Molecular formula: C10H10N4O2S
CAS number: 68-35-9
Introduction
Antibacterial; intermediate-acting sulfonamide.a b
Uses for Sulfadiazine
Prevention of Rheumatic Fever Recurrence
Alternative for prevention of recurrent attacks of rheumatic fever (secondary prophylaxis).123 292 375
IM penicillin G benzathine is drug of choice for secondary prophylaxis of rheumatic fever;292 375 alternatives include oral penicillin V, oral sulfadiazine, and oral sulfisoxazole (only available in the US in fixed combination with erythromycin).292 375
AHA and AAP recommend long-term (continuous) secondary prophylaxis in patients who have been treated for documented acute rheumatic fever (even if manifested solely by Sydenham chorea) and in those with evidence of rheumatic heart disease (even after prosthetic valve replacement).292 375
Do not use for treatment of Streptococcus pyogenes (group A β-hemolytic streptococci, GAS) infections (e.g., pharyngitis and tonsillitis).123 292 375 580 Sulfadiazine will not eradicate S. pyogenes and, therefore, will not prevent sequelae such as rheumatic fever and glomerulonephritis.123 375 580
Toxoplasmosis
Treatment of toxoplasmosis caused by Toxoplasma gondii;123 134 155 156 184 185 usually used in conjunction with pyrimethamine (and leucovorin).123 134 155 156 184 185 Designated an orphan drug by FDA for use in conjunction with pyrimethamine for treatment of T. gondii encephalitis in patients with or without HIV infection.137
CDC, NIH, IDSA, and AAP recommend sulfadiazine in conjunction with pyrimethamine (and leucovorin) as the regimen of choice for initial treatment of toxoplasmosis in HIV-infected adults and adolescents155 and for treatment of acquired CNS, ocular, or systemic toxoplasmosis in HIV-infected children.156
Sulfadiazine in conjunction with atovaquone is recommended by CDC, NIH, and IDSA as one of several alternative regimens for treatment of toxoplasmosis in HIV-infected adults and adolescents who cannot tolerate or do not respond to or relapsed with the regimen of choice;155 sulfadiazine and atovaquone regimen not adequately studied for treatment of toxoplasmosis in children.156
Sulfadiazine in conjunction with pyrimethamine (and leucovorin) is the regimen of choice for treatment of congenital toxoplasmosis.156 Empiric treatment of congenital toxoplasmosis should be strongly considered if the mother had symptomatic or asymptomatic Toxoplasma infection during pregnancy, even if the mother received toxoplasmosis treatment during the pregnancy.156
Sulfadiazine used in conjunction with pyrimethamine (and leucovorin) is the regimen of choice for chronic maintenance therapy (secondary prophylaxis) to prevent relapse of T. gondii encephalitis† [off-label] in HIV-infected adults, adolescents, and children who have completed initial treatment of the disease.155 156
Acute Otitis Media (AOM)
Has been used in conjunction with penicillin for treatment of AOM caused by susceptible Haemophilus influenzae.123 b
When anti-infective therapy indicated for treatment of AOM, AAP recommends high-dose amoxicillin or fixed combination of amoxicillin and clavulanate as drugs of first choice for initial treatment and certain cephalosporins (cefdinir, cefpodoxime, cefuroxime, ceftriaxone) as alternatives for initial treatment in penicillin-allergic patients who do not have a history of severe and/or recent penicillin-allergic reactions.321 AAP states that sulfonamides should not be used as alternatives in patients who do not respond to amoxicillin.321
Chancroid
Has been used for treatment of chancroid caused by H. ducreyi.123 b CDC recommends azithromycin, ceftriaxone, ciprofloxacin, or erythromycin as the drugs of choice for chancroid;344 sulfadiazine not included in CDC recommendations.344
Chlamydial Infections
Has been used for treatment of infections caused by Chlamydia trachomatis (e.g., inclusion conjunctivitis, trachoma).123 Other anti-infectives (e.g., azithromycin, erythromycin) usually drugs of choice for these infections.292
Haemophilus influenzae Infections
Has been used for treatment of meningitis caused by H. influenzae as an adjunct to streptomycin.123 Other anti-infectives (e.g., ceftriaxone, cefotaxime, chloramphenicol, cefepime, meropenem, fluoroquinolones) usually recommended.506
Malaria
Has been used as an adjunct in the treatment of malaria caused by chloroquine-resistant Plasmodium falciparum.123 Not included in recommendations for treatment of malaria.134
Neisseria meningitidis Infections
Has been used for chemoprophylaxis in close contacts of individuals with invasive meningococcal disease caused by sulfonamide-susceptible Neisseria meningitidis serogroup A.123 No longer recommended because of high prevalence of N. meningitidis resistant to sulfonamides.b CDC and AAP recommend rifampin, ciprofloxacin, or ceftriaxone for such prophylaxis.292 376
Has been used for treatment of infections caused by susceptible N. meningitidis (including meningitis).123 Other anti-infectives (e.g., ceftriaxone, cefotaxime, penicillin G, ampicillin, chloramphenicol, fluoroquinolones, aztreonam) usually recommended.506
Nocardia Infections
Has been used for treatment of nocardiosis.123 292 Fixed combination of sulfamethoxazole and trimethoprim (co-trimoxazole) usually treatment of choice for Nocardia infections;197 292 some experts suggest avoiding sulfonamides that are less urine soluble (e.g., sulfadiazine).292
Multiple-drug regimens may be necessary in immunocompromised patients or those with severe or disseminated infections.292 Other drugs used alone or in multiple-drug regimens for treatment of nocardiosis include amikacin, tetracyclines, cephalosporins (ceftriaxone), carbapenems (imipenem, meropenem), fixed combination of amoxicillin and clavulanate, clarithromycin, cycloserine, or linezolid.197 292 In vitro susceptibility testing, if available, recommended to guide selection of anti-infectives for treatment of severe nocardiosis or for those who cannot tolerate or fail to respond to sulfonamide treatment.292
Plague
Has been used for treatment of plague† [off-label] caused by Yersinia pestis.688 May reduce mortality in patients with bubonic plague, but sulfonamides not generally recommended for pneumonic plague.688
Not considered a preferred or alternative agent for treatment of plague;197 688 sulfonamides appear to be less effective than other anti-infectives used in the treatment of plague (e.g., streptomycin, tetracycline, doxycycline).688
Urinary Tract Infections (UTIs)
Has been used for treatment of UTIs (e.g., pyelonephritis, pyelitis, cystitis) in the absence of obstructive uropathy or foreign bodies.123
Use only when UTIs are caused by susceptible Escherichia coli, Klebsiella, Enterobacter, Staphylococcus aureus, Proteus mirabilis, or P. vulgaris and only when other more soluble sulfonamides have been ineffective.123
Sulfadiazine Dosage and Administration
Administration
Oral Administration
Administer orally with a full glass (250 mL) of water.123
Maintain adequate fluid intake during therapy to minimize risk of crystalluria and stone formation.123
Dosage
Pediatric Patients
General Pediatric Dosage
Oral
Infants and children >2 months of age: Manufacturer recommends 75 mg/kg or 2 g/m2 initially, followed by 150 mg/kg or 4 g/m2 daily given in 4–6 equally divided doses.123
Children beyond neonatal period: AAP recommends 120–150 mg/kg daily given in 4–6 divided doses for the treatment of mild, moderate, or severe infections.292
Prevention of Rheumatic Fever Recurrence
Oral
Infants and children >2 months of age: Manufacturer recommends 500 mg once daily in those weighing <30 kg or 1 g once daily in those weighing >30 kg.123
AHA and AAP recommend 500 mg once daily in those weighing ≤27 kg or 1 g once daily in those weighing >27 kg.292 375
Long-term, continuous prophylaxis required.292 375 (See Adults under Dosage and Administration.)
Toxoplasmosis
Treatment of Congenital Toxoplasmosis
Oral50 mg/kg twice daily in conjunction with oral pyrimethamine (2 mg/kg once daily for 2 days, then 1 mg/kg once daily for 2–6 months, then 1 mg/kg 3 times weekly) and oral or IM leucovorin (10 mg with each pyrimethamine dose).156
Recommended duration in HIV-infected infants is 12 months.156
Treatment of Toxoplasmosis in HIV-infected Infants and Children
Oral25–50 mg/kg (up to 1–1.5 g) 4 times daily in conjunction with oral pyrimethamine (2 mg/kg [up to 50 mg] once daily for 3 days, then 1 mg/kg [up to 25 mg] once daily) and oral leucovorin (10–25 mg once daily).156
Treatment duration at least 6 weeks;156 longer duration may be appropriate if disease is extensive or response incomplete at 6 weeks.156
Treatment of Toxoplasmosis in HIV-infected Adolescents
Oral1 g every 6 hours in those weighing <60 kg or 1.5 g every 6 hours in those weighing ≥60 kg in conjunction with oral pyrimethamine (200-mg loading dose, then 50 mg once daily in those weighing <60 kg or 75 mg once daily in those weighing ≥60 kg) and oral leucovorin (10–25 mg once daily; may be increased to 50 mg once or twice daily).155
Alternatively, 1 g every 6 hours in those weighing <60 kg or 1.5 g every 6 hours in those weighing ≥60 kg in conjunction with oral atovaquone (1.5 g twice daily).155
Treatment duration at least 6 weeks;155 longer duration may be appropriate if clinical or radiologic disease is extensive or response incomplete at 6 weeks.155
Prevention of Recurrence (Secondary Prophylaxis) of Toxoplasmosis in HIV-infected Infants and Children† [off-label]
Oral42.5–60 mg/kg twice daily (up to 2–4 g daily) in conjunction with oral pyrimethamine (1 mg/kg or 15 mg/m2 [up to 25 mg] once daily) and oral leucovorin (5 mg once every 3 days).156
Safety of discontinuing secondary prophylaxis against toxoplasmosis in HIV-infected children receiving potent antiretroviral therapy not extensively studied.156 If child has completed initial toxoplasmosis treatment, is asymptomatic for toxoplasmosis, and has received ≥6 months of antiretroviral therapy, can consider discontinuing secondary prophylaxis in those 1 to <6 years of age if CD4+ T-cell percentages remain ≥15% for >6 consecutive months or in those ≥6 years of age if CD4+ T-cell counts remain >200/mm3 for >6 consecutive months.156
Reinitiate secondary toxoplasmosis prophylaxis if CD4+ T-cell percentages decrease to <15% in HIV-infected children <6 years of age or if CD4+ T-cell counts decrease to <200/mm3 in HIV-infected children ≥6 years of age.156
Prevention of Recurrence (Secondary Prophylaxis) of Toxoplasmosis in HIV-infected Adolescents† [off-label]
Oral2–4 g daily in 2–4 divided doses in conjunction with oral pyrimethamine (25–50 mg once daily) and oral leucovorin (10–25 mg once daily).155
Criteria for initiating or discontinuing secondary prophylaxis against toxoplasmosis in adolescents are the same as those for adults.155 (See Adults under Dosage and Administration.)
Adults
General Adult Dosage
Oral
2–4 g initially, followed by 2–4 g daily in 3–6 equally divided doses.123
Prevention of Rheumatic Fever Recurrence
Oral
Adults weighing >30 kg: Manufacturer recommends 1 g once daily.123
Adults weighing >27 kg: AHA and AAP recommend 1 g once daily.292 375
AHA and AAP recommend long-term, continuous prophylaxis.292 375 (See Table 1.)
|
Patient Category |
Duration |
|---|---|
|
Rheumatic fever without carditis |
5 years or until 21 years of age, whichever is longer |
|
Rheumatic fever with carditis but no residual heart disease (no valvular disease) |
10 years since last episode or until 21 years of age, whichever is longer |
|
Rheumatic fever with carditis and residual heart disease (persistent valvular disease) |
10 years since last episode or until 40 years of age, whichever is longer; sometimes for life |
Toxoplasmosis
Treatment of Toxoplasmosis in HIV-infected Adults
Oral1 g every 6 hours in those weighing <60 kg or 1.5 g every 6 hours in those weighing ≥60 kg in conjunction with oral pyrimethamine (200-mg loading dose, then 50 mg once daily in those weighing <60 kg or 75 mg once daily in those weighing ≥60 kg) and oral leucovorin (10–25 mg once daily; may be increased to 50 mg once or twice daily).155
Alternatively, 1 g every 6 hours in those weighing <60 kg or 1.5 g every 6 hours in those weighing ≥60 kg in conjunction with oral atovaquone (1.5 g twice daily).155
Treatment duration at least 6 weeks; longer duration may be appropriate if clinical or radiologic disease is extensive or response incomplete at 6 weeks.155
Prevention of Recurrence (Secondary Prophylaxis) of Toxoplasmosis in HIV-infected Adults† [off-label]
Oral2–4 g daily in 2–4 divided doses in conjunction with oral pyrimethamine (25–50 mg once daily) and oral leucovorin (10–25 mg once daily).155
Initiate secondary toxoplasmosis prophylaxis in all HIV-infected adults who have been treated for T. gondii encephalitis.155
Consider discontinuing secondary toxoplasmosis prophylaxis in adults who completed toxoplasmosis treatment, are asymptomatic with respect to toxoplasmic encephalitis, and have responded to antiretroviral therapy with CD4+ T-cell counts that have remained >200/mm3 for >6 months.155
Reinitiate secondary toxoplasmosis prophylaxis if CD4+ T-cell count decreases to <200/mm3.155
Nocardiosis
Oral
4–8 g daily for a minimum of 6 weeks.a Continue for several months after apparent cure to prevent relapse.a
Prescribing Limits
Pediatric Patients
General Pediatric Dosage
Oral
Maximum 6 g daily.123
Toxoplasmosis
Treatment in HIV-infected Infants and Children
OralMaximum 1–1.5 g per dose 4 times daily.156
Prevention of Recurrence (Secondary Prophylaxis) of Toxoplasmosis in HIV-infected Infants and Children†
OralMaximum 2–4 g daily.156
Special Populations
No specific dosage recommendations.123
Cautions for Sulfadiazine
Contraindications
-
Hypersensitivity to sulfonamides123 or other chemically related drugs (e.g., sulfonylureas, thiazides).b
-
Infants <2 months of age (except as adjunctive therapy with pyrimethamine for treatment of congenital toxoplasmosis).123 (See Toxoplasmosis under Uses.)
-
Pregnancy at term.123
-
Nursing women.123
-
Porphyria.b
Warnings/Precautions
Warnings
Severe Reactions
Severe (sometimes fatal) reactions, including Stevens-Johnson syndrome, toxic epidermal necrolysis, fulminant hepatic necrosis, agranulocytosis, aplastic anemia, and other blood dyscrasias, reported with sulfonamides.123 b
Sore throat, fever, pallor, purpura, or jaundice may be early indications of serious reactions.123
Discontinue sulfadiazine at first appearance of rash or any sign of adverse reactions.b
Sensitivity Reactions
Hypersensitivity Reactions
Deaths associated with sulfonamide hypersensitivity reactions reported.123
Serum sickness syndrome or serum sickness-like reactions (e.g., fever, chills, rigors, flushing, joint pain, urticarial eruptions, conjunctivitis, bronchospasm, leukopenia) reported with sulfonamides.b
Various dermatologic reactions, including rash, pruritus, urticaria, erythema nodosum, erythema multiforme (Stevens-Johnson syndrome), Lyell’s syndrome (may be associated with corneal damage), Behcet’s syndrome, toxic epidermal necrolysis, and exfoliative dermatitis, reported in patients receiving sulfonamides.b
Photosensitivity reported.b
Incidence of hypersensitivity reactions appears to increase with increased sulfonamide dosage.b
Use with caution in patients with severe allergy or bronchial asthma.123
If a hypersensitivity reaction occurs during sulfonamide therapy, immediately discontinue the drug.b
Desensitization
Desensitization to sulfadiazine has been performed when use of the drug for the treatment of toxoplasmosis was considered necessary in HIV-infected patients who had a history of sulfadiazine hypersensitivity.107
Consult specialized references for specific information on desensitization procedures and dosage.107
Cross-sensitivity
Although cross-sensitization has been reported to occur between the various anti-infective sulfonamides, some diuretics such as acetazolamide and the thiazides, some goitrogens, and sulfonylurea antidiabetic agents,119 123 the association between hypersensitivity to sulfonamide anti-infectives and subsequent sensitivity reactions to non-anti-infective sulfonamides (e.g., thiazides, sulfonylurea antidiabetic agents, furosemide, dapsone, probenecid) appears to result from a predisposition to allergic reactions in general rather than to cross-sensitivity to the sulfa moiety per se.119
General Precautions
Renal Effects
Sulfonamides have been associated with renal toxicity manifested by renal colic, nephritis, urolithiasis, toxic nephrosis with anuria and oliguria, hematuria, proteinuria, crystalluria, kidney stone formation, and elevation of BUN and serum creatinine concentrations.b Nephritis and hemolytic-uremic syndrome also have been reported.b
Adverse renal effects usually are the result of crystalluria.b Risk of crystalluria may be decreased by maintaining an adequate urinary output and by increasing urinary pH.b Unless the urine is highly acidic and/or the drug is relatively insoluble, alkalinization of the urine usually is not necessary if urinary output is maintained at a minimum of 1.5 L daily.b
Perform urinalysis and assess kidney function frequently during sulfonamide therapy.b Maintain adequate fluid intake to minimize risk of crystalluria and stone formation.123 b
If persistent, heavy crystalluria, hematuria, or oliguria occurs, sulfonamide therapy should be discontinued and alkali therapy maintained.b
Patients with G6PD Deficiency
Hemolysis may occur in individuals with glucose-6-phosphate dehydrogenase (G6PD) deficiency; this effect may be dose-related.123 b
Laboratory Monitoring
Perform CBCs frequently during sulfadiazine therapy.123
Perform urinalysis (with careful microscopic examination) frequently during sulfadiazine therapy, especially in patients with impaired renal function.123
Considerable interindividual variations in sulfadiazine plasma concentrations occur with a given dosage.123 Measure sulfadiazine blood concentrations in patients being treated for serious infections.123 Free sulfonamide concentrations of 5–15 mg/100 mL may be considered therapeutically effective for most infections; concentrations of 12–15 mg/100 mL may be considered optimal for serious infections.123 Do not exceed total blood concentrations of 20 mg/100 mL since adverse reactions occur more frequently above this level.123
Selection and Use of Anti-infectives
To reduce development of drug-resistant bacteria and maintain effectiveness of sulfadiazine and other antibacterials, use only for treatment or prevention of infections proven or strongly suspected to be caused by susceptible bacteria.b
When selecting or modifying anti-infective therapy, use results of culture and in vitro susceptibility testing.123 b Consider that in vitro susceptibility tests are not always reliable for sulfonamides.123 If the patient is already taking sulfonamides, ensure that follow-up cultures have aminobenzoic acid added to the culture media.123
Specific Populations
Pregnancy
Category C.123
Contraindicated in pregnant women at term.123 Crosses placenta;123 may increase risk of neonatal hyperbilirubinemia and kernicterus.123
Lactation
Contraindicated in nursing women;123 discontinue drug or nursing.123
Distributed into milk;123 may cause kernicterus in the infant.123
Pediatric Use
Contraindicated in infants <2 months of age (except when considered necessary for adjunctive use with pyrimethamine for treatment of congenital toxoplasmosis).123 (See Toxoplasmosis under Uses.)
Kernicterus, caused by displacement of bilirubin from protein binding sites, has occurred in neonates treated with sulfonamides.b
Hepatic Impairment
Use with caution.123
Renal Impairment
Use with caution.123 (See Renal Effects under Cautions.)
Common Adverse Effects
GI effects (anorexia, nausea, vomiting, abdominal pain), headache, peripheral neuritis, fever, rash, pancreatitis, stomatitis, depression.123
Drug Interactions
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Anticoagulants, oral (warfarin) |
Sulfonamides may potentiate effects of warfarin by displacing it from its protein-binding sites123 b |
Closely monitorb |
|
Antidiabetic agents |
Sulfonamides may potentiate hypoglycemic effects of oral antidiabetic agents, including sulfonylurea agents123 b |
Increased glucose monitoring warrantedb |
|
Methotrexate |
Sulfonamides may increase concentrations and potentiate effects of methotrexate by displacing it from protein-binding sites or inhibiting renal transport of the drug123 b |
Use concomitantly with cautionb |
|
Probenecid |
May displace sulfonamides from plasma albumin and increase concentrations of free drug in plasma123 |
|
|
NSAIAs (indomethacin) |
May displace sulfonamides from binding sites and increase concentrations of free drug in plasma123 b |
Observe patient for possible adverse effectsb |
|
Salicylates |
May displace sulfonamides from plasma albumin and increase concentrations of free drug in plasma123 b |
Observe patient for possible adverse effectsb |
|
Thiazide diuretics |
Sulfonamides may potentiate diuretic effects by displacing thiazide diuretics from their protein-binding sites123 |
|
|
Uricosuric agents |
Sulfonamides may potentiate effects of uricosuric agents by displacing the agents from their protein-binding sites123 |
Sulfadiazine Pharmacokinetics
Absorption
Bioavailability
Readily absorbed from GI tract.123
Peak plasma concentrations attained within 3–7 hours.123 b Considerable interindividual variations in plasma sulfadiazine concentrations attained with a given dosage.123
Exists in blood as free, conjugated, and protein-bound drug; only the free form is microbiologically active.123
Distribution
Extent
Distributed into most body tissues; appears to freely cross cell membranes.a
Distributed into CSF.123 Free and total CSF concentrations may reach 32–65 and 40–60% of concurrent blood concentrations, respectively.123 Higher sulfonamide CSF concentrations may be reached if meninges are inflamed.a
Crosses placenta.123
Distributed into milk.123
Plasma Protein Binding
38–48%.123
Elimination
Metabolism
Liver; undergoes N4-acetylation (up to 40%).b
Elimination Route
Excreted principally in urine in the N4-acetylated form (about 15–40%) and unchanged (about 43–60%).123 a Approximately 50% of a single dose is excreted in the urine within 24 hours; 60–85% can be recovered within 72 hours.123 a
Half-life
About 7–17 hours.b
Stability
Storage
Oral
Tablets
20–25°C in tight, light-resistant container.123
Actions and Spectrum
-
Competitively inhibits bacterial synthesis of folic acid (pteroylglutamic acid) from aminobenzoic acid.123
-
Bacteriostatic in action.123
-
Inhibits only microorganisms that synthesize their own folic acid.b Animal cells and bacteria capable of utilizing folic acid precursors or preformed folic acid are resistant to sulfonamides.b
Advice to Patients
-
Advise patients to drink a full glass of water (250 mL) with each dose and at frequent intervals throughout the day to prevent crystalluria and stone formation.123
-
Importance of reporting the occurrence of sore throat, fever, pallor, purpura, or jaundice to a clinician since this may indicate a serious blood disorder.123
-
Advise patients that photosensitivity has been reported with sulfonamides and they should avoid exposure to UV light or prolonged exposure to sunlight.b
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.123
-
Importance of women informing clinician if they are or plan to become pregnant or plan to breast-feed.123
-
Importance of advising patients of other important precautionary information.123 (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
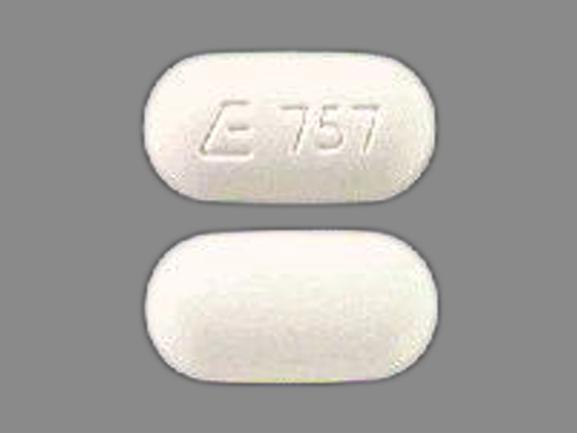
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
500 mg* |
Sulfadiazine Tablets |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions October 20, 2015. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
107. Bell ET, Tapper ML, Pollock AA. Sulphadiazine desensitisation in AIDS patients. Lancet. 1985; 1:163. https://pubmed.ncbi.nlm.nih.gov/2857234
119. Strom BL, Schinnar R, Apter AJ et al. Absence of cross-reactivity between sulfonamide antibiotics and sulfonamide nonantibiotics. N Engl J Med. 2003; 349:1628-35. https://pubmed.ncbi.nlm.nih.gov/14573734
123. Sandoz Inc. Sulfadiazine tablets prescribing information. Princeton, NJ; 2012 Mar.
134. Anon. Drugs for parasitic infections. Treat Guidel Med Lett. 2010; 8:e1-16. http://www.medletter.com
137. Food and Drug Administration. FDA Application: Search Orphan Drug Designations and Approvals. Rockville, MD. From FDA website. Accessed 2015 Aug 4. http://www.accessdata.fda.gov/scripts/opdlisting/oopd/index.cfm
155. Panel on Opportunistic Infections in HIV-infected Adults and Adolescents. Guidelines for prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: recommendations from the Centers for Disease Control and Prevention, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America (May 7, 2013). Updates may be available at HHS AIDS Information (AIDSinfo) website. http://www.aidsinfo.nih.gov
156. Panel on Opportunistic Infection in HIV-exposed and HIV-infected children, US Department of Health and Human Services (HHS). Guidelines for the prevention and treatment of opportunistic infections in HIV-exposed and HIV-infected children: recommendations from the National Institutes of Health, Centers for Disease Control and Prevention, the HIV Medicine Association of the Infectious Diseases Society of America, the Pediatric Infectious Diseases Society, and the American Academy of Pediatrics (Nov 6, 2013). Updates may be available at HHS AIDS Information (AIDSinfo) website. http://www.aidsinfo.nih.gov
184. Dannemann B, McCutchan A, Israelski D et al. Treatment of toxoplasmic encephalitis in patients with AIDS: a randomized trial comparing pyrimethamine plus clindamycin to pyrimethamine plus sulfadiazine. Ann Intern Med. 1992; 116:33-43. https://pubmed.ncbi.nlm.nih.gov/1727093
185. Porter SB, Sande MA. Toxoplasmosis of the central nervous system in the acquired immunodeficiency syndrome. N Engl J Med. 1992; 327:1643-8. https://pubmed.ncbi.nlm.nih.gov/1359410
197. Anon. Drugs for bacterial infections. Med Lett Treat Guid. 2010; 8:43-52.
292. American Academy of Pediatrics. Red Book: 2015 Report of the Committee on Infectious Diseases. 30th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2015.
321. Lieberthal AS, Carroll AE, Chonmaitree T et al. The diagnosis and management of acute otitis media. Pediatrics. 2013; 131:e964-99. https://pubmed.ncbi.nlm.nih.gov/23439909
344. Workowski KA, Bolan GA. Sexually Transmitted Diseases Treatment Guidelines, 2015. MMWR Recomm Rep. 2015; 64(RR-03):1-137. https://pubmed.ncbi.nlm.nih.gov/26042815
375. Gerber MA, Baltimore RS, Eaton CB et al. Prevention of rheumatic fever and diagnosis and treatment of acute Streptococcal pharyngitis: a scientific statement from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee of the Council on Cardiovascular Disease in the Young, the Interdisciplinary Council on Functional Genomics and Translational Biology, and the Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Academy of Pediatrics. Circulation. 2009; 119:1541-51. https://pubmed.ncbi.nlm.nih.gov/19246689
376. Cohn AC, MacNeil JR, Clark TA et al. Prevention and control of meningococcal disease: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2013; 62(RR-2):1-28. https://pubmed.ncbi.nlm.nih.gov/23515099
506. Tunkel AR, Hartman BJ, Kaplan SL et al. Practice guidelines for the management of bacterial meningitis. Clin Infect Dis. 2004; 39:1267-84. https://pubmed.ncbi.nlm.nih.gov/15494903
580. Shulman ST, Bisno AL, Clegg HW et al. Clinical practice guideline for the diagnosis and management of group A streptococcal pharyngitis: 2012 update by the Infectious Diseases Society of America. Clin Infect Dis. 2012; 55:1279-82. https://pubmed.ncbi.nlm.nih.gov/23091044
688. Inglesby TV, Dennis DT, Henderson DA et al for the Working Group on Civilian Biodefense. Plague as a biological weapon: medical and public health management. JAMA. 2000; 283:2281-90. https://pubmed.ncbi.nlm.nih.gov/10807389
a. AHFS Drug Information 2016. McEvoy GK, ed. Sulfadiazine. Bethesda, MD: American Society of Health-System Pharmacists. 2016.
b. AHFS Drug Information 2016. McEvoy GK, ed. Sulfonamides General Statement. Bethesda, MD: American Society of Health-System Pharmacists; 2016.
Related/similar drugs
More about sulfadiazine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: sulfonamides
- En español