Rifaximin (Monograph)
Brand name: Xifaxan
Drug class: Rifamycins
([Web])
Introduction
Rifamycin antibiotic;11 12 structural analog of rifampin.1 11 12
Uses for Rifaximin
Hepatic Encephalopathy
Reduction of risk of recurrence of overt hepatic encephalopathy in adults.1 20 21 36
Guidelines generally recommend rifaximin as an adjunct to lactulose for prevention of hepatic encephalopathy recurrence in patients who have had at least 1 episode of overt hepatic encephalopathy while receiving lactulose alone.36
Has been used in the treatment of hepatic encephalopathy† [off-label] to reduce blood ammonia concentrations and decrease severity of neurologic manifestations;6 7 8 9 10 11 17 21 36 37 designated an orphan drug by FDA for treatment of this condition.5
Information from the American Association for the Study of Liver Diseases (AASLD) and European Association for the Study of the Liver (EASL) regarding the management of hepatic encephalopathy, including recommendations for treatment and prevention of recurrence, is available at [Web].36 Treatment of overt hepatic encephalopathy first includes lactulose, while rifaximin is recommended as add-on therapy to prevent recurrence.36
Irritable Bowel Syndrome with Diarrhea
Treatment of irritable bowel syndrome (IBS) with diarrhea in adults.1 22 38 Guidelines for diarrhea-predominant IBS generally include use of rifaximin for treating global symptoms.2000 2001 Rifaximin is also recommended for retreatment in those who had a response to rifaximin and develop recurrent symptoms.2000
Travelers’ Diarrhea
Treatment of travelers’ diarrhea caused by noninvasive strains of Escherichia coli in adults and adolescents ≥12 years of age.1 3 4 12 13 18 19
Not effective in and should not be used for treatment of diarrhea complicated by fever or bloody stools.1
Not effective in and should not be used for treatment of diarrhea known or suspected to be caused by pathogens other than E. coli (e.g., Campylobacter jejuni, Shigella, Salmonella).1
Travelers' diarrhea caused by bacteria may be self-limited and often resolves within 3–7 days without anti-infective treatment.19 Guidelines generally consider rifaximin an alternative to fluoroquinolones or azithromycin for noninvasive moderate-to-severe travelers’ diarrhea.18 19 1002 1003
Has been used for prevention of travelers’ diarrhea† [off-label].14 15 16 18 19 42 1002 1003 CDC and others state that anti-infective prophylaxis for prevention of travelers' diarrhea is not recommended for most travelers.18 19
Other Uses
Has been used in some adults as treatment for the prevention of recurrence following standard treatment for Clostridioides difficile infection (CDI) in patients with multiple recurrences† [off-label].43 44 45 46
Has been used in combination therapy for patients with refractory acute pouchitis,† [off-label] although safety and efficacy have not been established.47 48 49
Has been used for treatment of small intestinal bacterial overgrowth,† [off-label] although safety and efficacy have not been established.50 51
Rifaximin Dosage and Administration
General
Patient Monitoring
-
Monitor for signs and symptoms of hypersensitivity reactions to rifaximin.1
-
Monitor for worsening or persistence of travelers’ diarrhea for more than 24–48 hours after initiation of rifaximin.1 Discontinue rifaximin if either occurs, and consider treatment with an alternative anti-infective.1
Administration
Oral Administration
Administer orally without regard to meals.1
Dosage
Pediatric Patients
Travelers’ Diarrhea
Treatment
OralAdolescents ≥12 years of age: 200 mg three times daily for 3 days.1
If diarrhea worsens or persists >24–48 hours after drug initiated, discontinue and consider alternative anti-infective.1
Adults
Hepatic Encephalopathy
Reduction of Risk of Recurrence of Overt Hepatic Encephalopathy
Oral550 mg twice daily.1
Treatment of Hepatic Encephalopathy†
Oral600–1200 mg daily (usually in 3 divided doses) for 7–21 days.6 7 8 9 10 17
Irritable Bowel Syndrome with Diarrhea
Oral
550 mg three times daily for 14 days.1
If symptoms recur, up to 2 additional courses may be given using the same 14-day regimen.1
Travelers’ Diarrhea
Treatment
Oral200 mg three times daily for 3 days.1
If diarrhea worsens or persists >24–48 hours after drug initiated, discontinue and consider alternative anti-infective.1
Prevention†
Oral200–1100 mg daily, divided into 1–3 doses.1002
Clostridioides difficile Infection - Patients With Multiple Recurrences†
Oral
400 mg three times daily for 20 days or 400 mg three times daily for 14 days, followed by 200 mg three times daily for an additional 14 days.43 45 46
Refractory Acute Pouchitis†
Oral
400 mg three times daily for 4 weeks or 1 gram twice daily for 15 days.48 49
Small Intestinal Bacterial Overgrowth†
Oral
400 mg three times daily for 10 days.50
Special Populations
Hepatic Impairment
Dosage adjustment not needed; use with caution in those with severe hepatic impairment (Child-Pugh class C).1
Renal Impairment
No specific dosage recommendations at this time.1
Geriatric Use
No specific dosage recommendations at this time.1
Cautions for Rifaximin
Contraindications
-
Hypersensitivity to rifaximin, other rifamycin anti-infectives, or any ingredient in the formulation.1
Warnings/Precautions
Travelers’ Diarrhea Not Caused by Escherichia Coli
Do not use for treatment of diarrhea complicated by fever or bloody stools.1
Do not use for treatment of travelers’ diarrhea known or suspected to be caused by C. jejuni, Shigella, or Salmonella.1 Rifaximin was not effective for diarrhea due to pathogens other than E. coli.1
If diarrhea worsens or persists >24–48 hours after initiating rifaximin, discontinue and consider use of another anti-infective.1
Clostridium difficile-associated Diarrhea (CDAD)
Treatment with anti-infectives alters normal colon flora and may permit overgrowth of Clostridium difficile.1 CDI and CDAD (also known as antibiotic-associated diarrhea and colitis or pseudomembranous colitis) are reported with nearly all anti-infectives, including rifaximin, and may range in severity from mild diarrhea to fatal colitis.1 C. difficile produces toxins A and B, which contribute to development of CDAD;1 hypertoxin-producing strains of C. difficile are associated with increased morbidity and mortality since they may be refractory to anti-infectives and colectomy may be required.1
Consider CDAD if diarrhea develops during or after therapy and manage accordingly.1 Obtain careful medical history since CDAD may occur as late as ≥2 months after anti-infective therapy is discontinued.1
If CDAD suspected or confirmed, discontinue anti-infectives not directed against C. difficile whenever possible.1 Initiate appropriate supportive therapy, anti-infective therapy directed against C. difficile, and surgical evaluation as clinically indicated.1
Development of Drug-Resistant Bacteria
Use for travelers’ diarrhea in absence of bacterial infection or a prophylactic indication is unlikely to provide benefit and increases risk of drug-resistant bacteria.1
Severe (Child-Pugh Class C) Hepatic Impairment
Systemic exposure increased in severe hepatic impairment.1 Exercise caution when administering rifaximin to patients with severe hepatic impairment (Child-Pugh Class C).1
Concomitant Use With P-glycoprotein Inhibitors
Concomitant use with P-glycoprotein (P-gp) transport inhibitors (e.g., cyclosporine) may substantially increase rifaximin systemic exposure.1 In patients with hepatic impairment, a potential additive effect of reduced hepatic metabolism and concomitant use with P-gp inhibitors may further increase rifaximin exposure.1 Exercise caution.1
Specific Populations
Pregnancy
Data not available regarding use in pregnant women.1 Teratogenic effects (e.g., ocular, oral and maxillofacial, cardiac, and lumbar spine malformations) observed in animal reproduction studies.1
Lactation
Not known whether distributed into human milk; effects on human milk production or effects on breast-fed infant are not known.1
Consider benefits of breast-feeding and importance of rifaximin to the female;1 also consider potential adverse effects on the breast-fed child from the drug or from the underlying maternal condition.1
Pediatric Use
Hepatic encephalopathy: Safety and efficacy not established in children and adolescents <18 years of age.1
IBS with diarrhea: Safety and efficacy not established in children and adolescents <18 years of age.1
Travelers' diarrhea: Safety and efficacy not established in children <12 years of age.1
Geriatric Use
Hepatic encephalopathy: No overall differences in safety or effectiveness observed between patients ≥65 years of age and younger adults.1
IBS with diarrhea: No overall differences in safety or effectiveness observed between patients ≥65 years of age and younger adults.1
Travelers' diarrhea: Experience in those ≥65 years of age insufficient to determine whether they respond differently than younger patients.1
Hepatic Impairment
Although dosage adjustments are not needed in patients with hepatic impairment, severe hepatic impairment (Child-Pugh class C) results in increased rifaximin systemic exposure and additional awareness and monitoring for rifaximin-related adverse effects would be suggested.1
Hepatic encephalopathy: Clinical trials did not include patients with MELD scores >25.1
Renal Impairment
Not specifically studied in renal impairment.1
Common Adverse Effects
Hepatic encephalopathy: Adverse effects (≥10%): peripheral edema, nausea, constipation, dizziness, fatigue, urinary tract infection, insomnia, anemia, pruritus, ascites.1
IBS with diarrhea: Adverse effects (≥2%): nausea, increased ALT concentration.1
Travelers' diarrhea: Adverse effects (≥2%): headache.1
Drug Interactions
Substrate of CYP3A4.1 Does not inhibit CYP1A2, 2A6, 2B6, 2C9, 2C19, 2D6, 2E1, or 3A4 in vitro.1 Has induced CYP3A4 in vitro, but clinically important effects on intestinal or hepatic CYP3A4 unlikely.1
Substrate of P-gp transport in vitro.1 Inhibits P-gp in vitro, but effect in vivo is unknown.1
Substrate of organic anion transport polypeptides (OATP) 1A2, 1B1, and 1B3, but in vivo effect is unknown.1 Not a substrate of OATP2B1.1 Inhibits OATP1B1, 1A2, and 1B3 in vitro, but effect in vivo is unknown.1
Drugs Affected by Hepatic Microsomal Enzymes
CYP3A4 substrates: Pharmacokinetic interactions not expected in patients with normal hepatic function;1 not known whether interactions occur in those with hepatic impairment resulting in increased rifaximin systemic exposure.1
CYP1A2, 2A6, 2B6, 2C9, 2C19, 2D6, and 2E1 substrates: Pharmacokinetic interactions not expected.1
Drugs Affecting or Affected by Transport Systems
P-gp inhibitors: Substantially increased rifaximin exposures may occur.1 Exercise caution with concomitant use; impaired hepatic function may further increase exposure to rifaximin.1
P-gp substrates: Possible effects in vivo are unknown.1
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Cyclosporine |
Substantially increased rifaximin concentrations and AUC1 Impaired hepatic function may result in additive exposure to rifaximin1 |
Clinical importance unknown; exercise caution1 |
|
Hormonal contraceptives (ethinyl estradiol and norgestimate) |
Decreased ethinyl estradiol and norgestimate concentrations1 |
Clinical importance unknown1 |
|
Midazolam |
No substantial changes in pharmacokinetics of midazolam or its major metabolite (1′-hydroxymidazolam) 1 |
Degree of interaction not clinically important1 |
|
Warfarin |
Changes in INR1 |
Monitor PT and INR; dosage adjustments of warfarin may be necessary1 |
Rifaximin Pharmacokinetics
Absorption
Bioavailability
Poor and variable absorption; not suitable for treatment of systemic bacterial infections.1
Systemic exposure dose proportional over a dosage range of 200–400 mg; less than dose-proportional over a dosage range of 400–600 mg.1
No evidence of accumulation following multiple doses.1
History of hepatic encephalopathy (rifaximin 550 mg twice daily): Mean AUC approximately 12-fold higher compared with healthy adults.1
IBS with diarrhea (rifaximin 550 mg three times daily for 14 days): AUC similar to healthy adults.1
Food
When administered 30 minutes after high-fat meal, time to peak plasma concentrations delayed from 0.75 hours to 1.5 hours after a dose,1 AUC increased twofold,1 peak plasma concentrations unchanged.1
Plasma Concentrations
Healthy adults (single or multiple rifaximin doses of 550 mg): Peak plasma concentrations attained 1 hour after dose;1 mean peak plasma concentrations range from 2.4–4 ng/mL.1
IBS with diarrhea (rifaximin 550 mg three times daily for 14 days): Peak plasma concentrations attained 1 hour after dose;1 mean peak plasma concentrations similar to healthy adults.1
Distribution
Unknown if distributed into breastmilk.1
Plasma Protein Binding
Healthy individuals: 67.5%.1
Hepatic impairment: 62%.1
Elimination
Metabolism
Systemically absorbed drug metabolized principally by CYP3A4.1
Elimination Route
Approximately 97% of an oral dose excreted in feces (mostly as unchanged drug);1 0.3% eliminated in urine (mostly as metabolites).1
Half-life
Healthy individuals: 5.6 hours.1
IBS with diarrhea: 6 hours.1
Special Populations
History of hepatic encephalopathy and with mild, moderate, or severe hepatic impairment: Systemic exposures approximately 10-, 14-, or 21-fold higher, respectively, compared with healthy adults.1
Stability
Storage
Oral
Tablets
20–25°C (excursions permitted between 15–30°C).1
Actions and Spectrum
-
Like other rifamycins, rifaximin inhibits RNA synthesis in susceptible bacteria by binding to the β subunit of bacterial DNA-dependent RNA polymerase.1
-
Escherichia coli: Active in vitro and in clinical infections (i.e., infectious diarrhea) against enterotoxigenic E. coli (ETEC) and enteroaggregative E. coli (EAEC).1
-
Not effective against C. jejuni and has not been proven effective against Shigella and Salmonella.1
-
Resistance generally is associated with mutations in the rpoB gene that change the binding site on DNA-dependent RNA polymerase and decrease rifaximin binding affinity.1
-
Cross-resistance between rifaximin and other classes of anti-infectives not observed.1
Advice to Patients
-
Advise patients that antibacterials (including rifaximin) should only be used to treat bacterial infections and not used to treat viral infections (e.g., the common cold).1
-
Advise patients that rifaximin may be taken with or without food.1
-
If used for treatment of travelers' diarrhea, advise patients of the importance of discontinuing rifaximin and seeking medical care if diarrhea worsens or persists for >24–48 hours after the drug is initiated or if fever and/or bloody diarrhea develop.1
-
Advise patients that diarrhea is a common problem caused by anti-infectives and usually ends when the drug is discontinued.1 Importance of contacting a clinician if watery and bloody stools (with or without stomach cramps and fever) occur during or as late as 2 months or longer after the last dose as this may be related to CDAD.1
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, and any concomitant illnesses.1
-
Advise females of child bearing potential to inform clinicians if they are or plan to become pregnant or plan to breast-feed.1
-
Inform patients of other important precautionary information.1
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
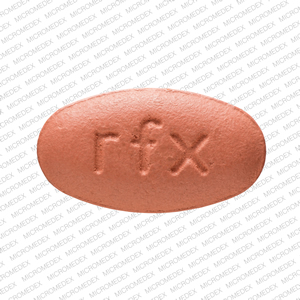
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
200 mg |
Xifaxan |
Salix |
|
550 mg |
Xifaxan |
Salix |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions December 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
1. Salix Pharmaceuticals, Inc. Xifaxan tablets prescribing information. Raleigh, NC; 2023 Oct.
3. Steffen R, Sack DA, Riopel L, et al. Therapy of traveler’s diarrhea with rifaximin on various continents. Am J Gastroenterol. 2003; 98:1073-8. https://pubmed.ncbi.nlm.nih.gov/12809830
4. Infante RM, Ericsson CD, Jiang Z, et al. Enteroaggregative Escherichia coli diarrhea in travelers: response to rifaximin therapy. Clin Gastroenterol Hepatol. 2003; 2:136-8.
5. Food and Drug Administration. FDA Application: Search Orphan Drug Designations and Approvals. Rockville, MD. From FDA website. Accessed 2024 May 29. https://www.accessdata.fda.gov/scripts/opdlisting/oopd/index.cfm
6. Riordan SM, Williams R. Treatment of hepatic encephalopathy. N Engl J Med. 1997;337:473-9.
7. Williams R, James OF, Warnes TW et al. Evaluation of the efficacy and safety of rifaximin in the treatment of hepatic encephalopathy: a double-blind, randomized, dose-finding multi-centre study. Eur J Gastroenterol Hepatol. 2000;12:203-8.
8. Puxeddu A, Quartini M, Massimetti A et al. Rifaximin in the treatment of chronic hepatic encephalopathy. Curr Med Res Opin. 1995;13:274-81.
9. Pedretti G, Calzetti C, Missale G et al. Rifaximin versus neomycin on hyperammoniemia in chronic portal systemic encephalopathy of cirrhotics. A double-blind, randomized trial. Ital J Gastroenterol. 1991;23:175-8.
10. Bucci L, Palmieri GC. Double-blind, double-dummy comparison between treatment with rifaximin and lactulose in patients with medium to severe degree hepatic encephalopathy. Curr Med Res Opin. 1993;13:109-18.
11. Gillis JC, Brogden RN.. Rifaximin. A review of its antibacterial activity, pharmacokinetic properties and therapeutic potential in conditions mediated by gastrointestinal bacteria. Drugs 1995;49:467-84.
12. Steffen R. Rifaximin: a nonabsorbed antimicrobial as a new tool for treatment of travelers’ diarrhea. J Travel Med. 2001;8:34-9.
13. DuPont HL, Ericsson CD, Mathewson JJ, et al. Rifaximin: a nonabsorbed antimicrobial in the therapy of travelers’ diarrhea. Digestion. 1998;59:708-14.
14. Flores J, Dupont HL, Jiang ZD et al. A randomized, double-blind, pilot study of rifaximin 550 mg versus placebo in the prevention of travelers' diarrhea in Mexico during the dry season. J Travel Med. 2011 Sep-Oct; 18:333-6.
15. Armstrong AW, Ulukan S, Weiner M et al. A randomized, double-blind, placebo-controlled study evaluating the efficacy and safety of rifaximin for the prevention of travelers' diarrhea in US military personnel deployed to Incirlik Air Base, Incirlik, Turkey. J Travel Med. 2010 Nov-Dec; 17:392-4.
16. Hu Y, Ren J, Zhan M et al. Efficacy of rifaximin in prevention of travelers' diarrhea: a meta-analysis of randomized, double-blind, placebo-controlled trials. J Travel Med. 2012; 19:352-6. https://pubmed.ncbi.nlm.nih.gov/23379704
17. Miglio F, Valpiani D, Rossellini SR, et al. Rifaximin, a non-absorbable rifamycin, for the treatment of hepatic encephalopathy. A double-blind, randomised trial. Curr Med Res Opin. 1997;13:593-601.
18. . Advice for travelers. Med Lett Drugs Ther. 2019; 61:153-60. https://pubmed.ncbi.nlm.nih.gov/25853663
19. Centers for Disease Control and Prevention. CDC health information for international travel, 2019. Atlanta, GA: US Department of Health and Human Services. Updates may be available at CDC website. https://wwwnc.cdc.gov/travel/yellowbook/2024/preparing/travelers-diarrhea
20. Bass NM, Mullen KD, Sanyal A et al. Rifaximin treatment in hepatic encephalopathy. N Engl J Med. 2010; 362:1071-81. https://pubmed.ncbi.nlm.nih.gov/20335583
21. Eltawil KM, Laryea M, Peltekian K et al. Rifaximin vs. conventional oral therapy for hepatic encephalopathy: a meta-analysis. World J Gastroenterol. 2012; 18:767-77. https://pubmed.ncbi.nlm.nih.gov/22371636
22. Pimentel M, Lembo A, Chey WD et al. Rifaximin therapy for patients with irritable bowel syndrome without constipation. N Engl J Med. 2011; 364:22-32. https://pubmed.ncbi.nlm.nih.gov/21208106
25. American Society of Health-System Pharmacists Commission on Therapeutics. ASHP therapeutic position statement on the preferential use of metronidazole for the treatment of Clostridium difficile-associated disease. Am J Health-Syst Pharm. 1998; 55:1407-11. https://pubmed.ncbi.nlm.nih.gov/9659970
26. Ouyang-Latimer J, Jafri S, VanTassel A et al. In vitro antimicrobial susceptibility of bacterial enteropathogens isolated from international travelers to Mexico, Guatemala, and India from 2006 to 2008. Antimicrob Agents Chemother. 2011; 55:874-8. https://pubmed.ncbi.nlm.nih.gov/21115800
27. Kothary V, Scherl EJ, Bosworth B et al. Rifaximin resistance in Escherichia coli associated with inflammatory bowel disease correlates with prior rifaximin use, mutations in rpoB, and activity of Phe-Arg-β-naphthylamide-inhibitable efflux pumps. Antimicrob Agents Chemother. 2013; 57:811-7. https://pubmed.ncbi.nlm.nih.gov/23183443
28. Hopkins KL, Mushtaq S, Richardson JF et al. In vitro activity of rifaximin against clinical isolates of Escherichia coli and other enteropathogenic bacteria isolated from travellers returning to the UK. Int J Antimicrob Agents. 2014; 43:431-7. https://pubmed.ncbi.nlm.nih.gov/24661532
29. Ruiz J, Mensa L, Pons MJ et al. Development of Escherichia coli rifaximin-resistant mutants: frequency of selection and stability. J Antimicrob Chemother. 2008; 61:1016-9. https://pubmed.ncbi.nlm.nih.gov/18325895
30. Dogan B, Scherl E, Bosworth B et al. Multidrug resistance is common in Escherichia coli associated with ileal Crohn's disease. Inflamm Bowel Dis. 2013; 19:141-50. https://pubmed.ncbi.nlm.nih.gov/22508665
31. Gomi H, Jiang ZD, Adachi JA et al. In vitro antimicrobial susceptibility testing of bacterial enteropathogens causing traveler's diarrhea in four geographic regions. Antimicrob Agents Chemother. 2001; 45:212-6. https://pubmed.ncbi.nlm.nih.gov/11120968
32. Scrascia M, Forcillo M, Maimone F et al. Susceptibility to rifaximin of Vibrio cholerae strains from different geographical areas. J Antimicrob Chemother. 2003; 52:303-5. https://pubmed.ncbi.nlm.nih.gov/12837732
33. Sierra JM, Navia MM, Vargas M et al. In vitro activity of rifaximin against bacterial enteropathogens causing diarrhoea in children under 5 years of age in Ifakara, Tanzania. J Antimicrob Chemother. 2001; 47:904-5. https://pubmed.ncbi.nlm.nih.gov/11389133
34. O'Connor JR, Galang MA, Sambol SP et al. Rifampin and rifaximin resistance in clinical isolates of Clostridium difficile. Antimicrob Agents Chemother. 2008; 52:2813-7. https://pubmed.ncbi.nlm.nih.gov/18559647
35. Carman RJ, Boone JH, Grover H et al. In vivo selection of rifamycin-resistant Clostridium difficile during rifaximin therapy. Antimicrob Agents Chemother. 2012; 56:6019-20. https://pubmed.ncbi.nlm.nih.gov/22908175
36. American Association for the Study of Liver Diseases (AASLD). and European Association for the Study of the Liver (EASL). Hepatic encephalopathy in chronic liver disease: 2014 practice guideline by AASLD and EASL. From the AASLD website. Accessed 2024 May 29. https://www.aasld.org/sites/default/files/2022-07/Hepatic%20Encephalopathy%20in%20Chronic%20Liver%20Disease%202014.pdf
37. Cheng J, Chen Y, Cao W, Zuo G. Is rifaximin better than nonabsorbable disaccharides in hepatic encephalopathy?: A meta-analysis. Medicine (Baltimore). 2021;100(51):e28232.
38. Lembo A, Pimentel M, Rao SS, et al. Repeat Treatment With Rifaximin Is Safe and Effective in Patients With Diarrhea-Predominant Irritable Bowel Syndrome. Gastroenterology. 2016;151(6):1113-1121.
39. Black CJ, Burr NE, Camilleri M, et al. Efficacy of pharmacological therapies in patients with IBS with diarrhoea or mixed stool pattern: systematic review and network meta-analysis. Gut. 2020;69(1):74-82.
40. Ford AC, Harris LA, Lacy BE, Quigley EMM, Moayyedi P. Systematic review with meta-analysis: the efficacy of prebiotics, probiotics, synbiotics and antibiotics in irritable bowel syndrome. Aliment Pharmacol Ther. 2018;48(10):1044-1060.
41. Riddle MS, Connor P, Fraser J, et al. Trial Evaluating Ambulatory Therapy of Travelers' Diarrhea (TrEAT TD) Study: A Randomized Controlled Trial Comparing 3 Single-Dose Antibiotic Regimens With Loperamide. Clin Infect Dis. 2017;65(12):2008-2017.
42. Fan H, Gao L, Yin Z, Ye S, Zhao H, Peng Q. Probiotics and rifaximin for the prevention of travelers' diarrhea: A systematic review and network meta-analysis. Medicine (Baltimore). 2022;101(40):e30921.
43. Kelly CR, Fischer M, Allegretti JR, et al. ACG Clinical Guidelines: Prevention, Diagnosis, and Treatment of Clostridioides difficile Infections [published correction appears in Am J Gastroenterol. 2022 Feb 1;117(2):358]. Am J Gastroenterol. 2021;116(6):1124-1147.
44. Johnson S, Lavergne V, Skinner AM, et al. Clinical Practice Guideline by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA): 2021 Focused Update Guidelines on Management of Clostridioides difficile Infection in Adults. Clin Infect Dis. 2021;73(5):e1029-e1044.
45. Garey KW, Ghantoji SS, Shah DN, et al. A randomized, double-blind, placebo-controlled pilot study to assess the ability of rifaximin to prevent recurrent diarrhoea in patients with Clostridium difficile infection. J Antimicrob Chemother. 2011;66(12):2850-2855.
46. Major G, Bradshaw L, Boota N, et al. Follow-on RifAximin for the Prevention of recurrence following standard treatment of Infection with Clostridium Difficile (RAPID): a randomised placebo controlled trial. Gut. 2019;68(7):1224-1231.
47. Poo S, Sriranganathan D, Segal JP. Network meta-analysis: efficacy of treatment for acute, chronic, and prevention of pouchitis in ulcerative colitis. Eur J Gastroenterol Hepatol. 2022;34(5):518-528.
48. Isaacs KL, Sandler RS, Abreu M, et al. Rifaximin for the treatment of active pouchitis: a randomized, double-blind, placebo-controlled pilot study. Inflamm Bowel Dis. 2007;13(10):1250-1255.
49. Gionchetti P, Rizzello F, Venturi A, et al. Antibiotic combination therapy in patients with chronic, treatment-resistant pouchitis. Aliment Pharmacol Ther. 1999;13(6):713-718.
50. Pimentel M, Saad RJ, Long MD, Rao SSC. ACG Clinical Guideline: Small Intestinal Bacterial Overgrowth. Am J Gastroenterol. 2020;115(2):165-178.
51. Gatta L, Scarpignato C. Systematic review with meta-analysis: rifaximin is effective and safe for the treatment of small intestine bacterial overgrowth. Aliment Pharmacol Ther. 2017;45(5):604-616.
1002. Riddle MS, Connor BA, Beeching NJ, et al. Guidelines for the prevention and treatment of travelers' diarrhea: a graded expert panel report. J Travel Med. 2017;24(suppl_1):S57-S74.
1003. Riddle MS, DuPont HL, Connor BA. ACG Clinical Guideline: Diagnosis, Treatment, and Prevention of Acute Diarrheal Infections in Adults. Am J Gastroenterol. 2016;111(5):602-622.
2000. Lembo A, Sultan S, Chang L, Heidelbaugh JJ, Smalley W, Verne GN. AGA Clinical Practice Guideline on the Pharmacological Management of Irritable Bowel Syndrome With Diarrhea. Gastroenterology. 2022;163(1):137-151.
2001. Lacy BE, Pimentel M, Brenner DM, et al. ACG Clinical Guideline: Management of Irritable Bowel Syndrome. Am J Gastroenterol. 2021;116(1):17-44.
Related/similar drugs
More about rifaximin
- Check interactions
- Compare alternatives
- Reviews (160)
- Side effects
- Dosage information
- During pregnancy
- Drug class: miscellaneous antibiotics
- Breastfeeding
- En español