Raloxifene Hydrochloride (Monograph)
Brand name: Evista
Drug class: Estrogen Agonists-Antagonists
Warning
-
Increased risk for DVT and pulmonary embolism. Contraindicated in women with active or past episodes of venous thrombosis.
-
Increased risk of fatal stroke reported in women with CHD or increased risk for CHD. Weigh risks versus benefits in women at risk for stroke.
Introduction
Estrogen agonist-antagonist; a nonsteroidal benzothiophene derivative.
Uses for Raloxifene Hydrochloride
Osteoporosis in Postmenopausal Women
Prevention of osteoporosis in postmenopausal women. Risk factors for postmenopausal osteoporosis and related fractures include early menopause, advanced age, low bone mineral density (BMD), low body mass index (BMI), previous fracture or family history of fracture/osteoporosis, excessive alcohol intake, smoking, inadequate physical activity, low calcium and vitamin D intake, certain drugs (e.g., glucocorticoids), and medical conditions or diseases (e.g., rheumatoid arthritis, diabetes mellitus, Cushing syndrome, hyperparathyroidism).
Treatment of osteoporosis in postmenopausal women.
In addition to adequate intake of calcium/vitamin D and other lifestyle modifications (e.g., exercise, avoidance of excessive alcohol and tobacco use), experts recommend that pharmacologic therapy for osteoporosis be considered in postmenopausal women with high risk of fractures (generally those who have experienced a previous hip or vertebral fracture or who have low BMD); pharmacologic therapy also may be considered in postmenopausal women with low bone mass, although there is less evidence supporting overall fracture risk reduction in such patients.
Use of a drug with proven antifracture efficacy is recommended; experts generally recommend raloxifene as a second- or third-line agent after other therapies (e.g., bisphosphonates) have been attempted.
Individualize choice of therapy based on potential benefits (with respect to fracture risk reduction) and adverse effects of therapy, patient preferences, comorbidities, and risk factors.
Use supplemental calcium and/or vitamin D concomitantly if daily dietary intake is considered inadequate.
Glucocorticoid-induced Osteoporosis
Has been used for prevention and treatment of glucocorticoid-induced osteoporosis† [off-label].
American College of Rheumatology (ACR) recommends optimizing calcium and vitamin D intake and lifestyle modifications (e.g., diet, smoking cessation, weight-bearing or resistance-training exercise) in all patients receiving long-term glucocorticoid therapy; in addition, pharmacologic therapy with an oral bisphosphonate is recommended in patients at moderate-to-high risk of fracture. Oral bisphosphonates are preferred because of their demonstrated antifracture benefits, safety, and cost; experts state raloxifene may be used in postmenopausal women if no other therapy is available.
Breast Cancer
Reduction in the incidence of invasive breast cancer in postmenopausal women with osteoporosis.
Reduction in the incidence of invasive breast cancer in postmenopausal women at high risk for developing the disease. Long-term follow-up (approximately 7 years) demonstrated reduced efficacy compared with tamoxifen in reducing the risk of invasive breast cancer (STAR trial). Effect on breast cancer incidence in women with BRCA1 or BRCA2 genetic mutations not established.
Not studied in women with a history of exposure to thoracic radiation, which is considered a possible risk factor for breast cancer.
Not indicated for the treatment of breast cancer or to reduce the risk of recurrence of breast cancer. Not indicated for reduction in the risk of noninvasive breast cancer.
Raloxifene Hydrochloride Dosage and Administration
Administration
Oral Administration
Administer orally once daily without regard to meals or time of day.
Dosage
Available as raloxifene hydrochloride; dosage expressed in terms of the salt.
Adults
Osteoporosis
Prevention in Postmenopausal Women
Oral60 mg daily.
Treatment in Postmenopausal Women
Oral60 mg daily.
Breast Cancer
Reduction in the Incidence of Invasive Breast Cancer
Oral60 mg daily. Optimum duration of therapy unknown. ASCO recommends a treatment duration of 5 years. If a patient is receiving raloxifene as treatment for osteoporosis, for which breast cancer reduction is a secondary goal, ASCO suggests that treatment duration may be extended beyond 5 years.
Cautions for Raloxifene Hydrochloride
Contraindications
-
Active or past episodes of venous thrombosis, including DVT, pulmonary embolism, or retinal vein thrombosis.
-
Women who are pregnant.
Warnings/Precautions
Warnings
Cardiovascular Effects
Increased risk of venous thromboembolic events (e.g., DVT, pulmonary embolism).
Discontinue raloxifene ≥72 hours before and during prolonged immobilization (e.g., postsurgery recovery, prolonged bed rest); resume therapy once patient is fully ambulatory.
Assess potential benefit versus risk in women at risk of thromboembolic disease secondary to CHF, superficial thrombophlebitis, or active malignancy.
Increased risk for fatal stroke reported in women with CHD or increased risk for CHD (RUTH study). Assess potential benefit versus risk in women at risk of stroke secondary to history of stroke or TIA, atrial fibrillation, hypertension, or cigarette smoking.
Not indicated for the primary or secondary prevention of cardiovascular disease.
Fetal/Neonatal Morbidity and Mortality
May cause fetal harm. Embryotoxic and teratogenic effects demonstrated in animals. Not indicated for use in women of childbearing potential. If inadvertently used during pregnancy or if patient becomes pregnant, apprise of potential fetal hazard.
General Precautions
Use in Premenopausal Women
Not indicated. Safety not established.
Effects on Lipids
Potential for increased serum triglyceride concentrations in women with a history of substantial hypertriglyceridemia during oral estrogen therapy; monitor serum triglycerides in these women.
Effects on the Breast
Not studied in women with a history of breast cancer.
Investigate unexplained breast abnormality. Does not eliminate risk of breast cancer.
Use in Men
Safety and efficacy not evaluated.
GU Effects
Not associated with endometrial proliferation. Investigate unexplained uterine bleeding.
Specific Populations
Pregnancy
May cause fetal harm. Not indicated for use in women of childbearing potential.
Lactation
Not known whether raloxifene distributes into human milk or affects milk production or the nursing infant; however, because the drug is an estrogen agonist-antagonist, estrogenic effects on mammary tissue may be affected.
Pediatric Use
Not indicated.
Geriatric Use
No substantial differences in safety, efficacy, or pharmacokinetic profile relative to younger adults.
Hepatic Impairment
Use with caution; safety and efficacy not established in patients with hepatic impairment.
Renal Impairment
Use with caution in patients with moderate to severe renal impairment; safety and efficacy not established in these patients.
Common Adverse Effects
Hot flushes (flashes), leg cramps, peripheral edema, flu-like syndrome, arthralgia, sweating.
Drug Interactions
Metabolism apparently not mediated by CYP isoenzymes.
Protein-bound Drugs
Concomitant administration with other highly protein-bound drugs not expected to affect plasma raloxifene concentrations. Caution advised if used concomitantly with other highly protein-bound drugs.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Amoxicillin and ampicillin |
Ampicillin: Decreased peak plasma raloxifene concentrations; no change in systemic exposure to raloxifene Amoxicillin: No change in raloxifene concentrations |
Can be administered concomitantly |
|
Anion-exchange resins (cholestyramine) |
Decreased absorption and enterohepatic cycling of raloxifene with concomitant cholestyramine administration; similar interaction expected with other anion-exchange resins |
Concomitant administration with cholestyramine not recommended |
|
Antacids (aluminum- and magnesium-containing, calcium carbonate) |
No change in systemic exposure of raloxifene |
Can be administered concomitantly |
|
Anticoagulants, oral |
Decreased warfarin effects; no effect on warfarin pharmacokinetics observed |
Monitor PT carefully |
|
Antilipemic agents |
Concomitant use not specifically studied |
|
|
Diazepam |
Potential for altered protein binding of diazepam |
Caution advised |
|
Diazoxide |
Potential for altered protein binding of diazoxide |
Caution advised |
|
Digoxin |
No change in digoxin pharmacokinetics |
Can be administered concomitantly |
|
Estrogens |
Not studied |
Concomitant use not recommended |
|
Gemfibrozil |
No substantial change in plasma raloxifene concentrations |
|
|
Lidocaine |
Potential for altered protein binding of lidocaine |
Caution advised |
|
Methylprednisolone |
No change in methylprednisolone pharmacokinetics |
Can be administered concomitantly with corticosteroids |
|
Phenytoin |
No change in protein binding of phenytoin |
Raloxifene Hydrochloride Pharmacokinetics
Absorption
Bioavailability
Rapidly absorbed from GI tract; 60% of an oral dose is absorbed, but absolute bioavailability as unchanged drug is only 2% because of extensive first-pass glucuronidation.
Following oral administration, peak plasma concentrations achieved at 6 hours (raloxifene) and 1 hour (glucuronide conjugates).
Food
High-fat meal increases peak plasma concentration and extent of absorption of raloxifene, but does not substantially affect systemic exposure.
Special Populations
Plasma raloxifene concentrations are 150% higher in patients with cirrhosis (Child-Pugh class A) and total serum bilirubin concentrations of 0.6–2 mg/dL than in individuals with normal hepatic function. Pharmacokinetics not studied in individuals with moderate or severe hepatic impairment.
Plasma raloxifene concentrations in those with mild renal impairment are similar to values in women with normal renal function. AUC of raloxifene is 122% higher in individuals with moderate renal impairment (Clcr 31–50 mL/minute) or severe renal impairment (Clcr ≤30 mL/minute) than in individuals with normal renal function.
Distribution
Plasma Protein Binding
Raloxifene and its monoglucuronide conjugates: >95%. Raloxifene binds to albumin and α1-acid glycoprotein but not to testosterone-estradiol binding globulin (sex hormone binding globulin).
Elimination
Metabolism
Undergoes extensive first-pass metabolism to glucuronide conjugates. Does not appear to be metabolized by CYP isoenzymes. Conjugates converted back to the parent drug in various tissues.
Elimination Route
Excreted principally in feces as unabsorbed drug and via biliary elimination as glucuronide conjugates (subsequently metabolized by bacteria in GI tract to the parent drug).
Half-life
32.5 hours.
Stability
Storage
Oral
Tablets
20–25°C.
Actions
-
Selective estrogen receptor modulator (SERM); exhibits estrogen agonist activity on bone, but estrogen antagonist activity on breast and uterine tissue.
-
Differs chemically and pharmacologically from naturally occurring estrogens, synthetic steroidal and nonsteroidal compounds with estrogenic activity, and agents described as antiestrogens (e.g., clomiphene, tamoxifen, toremifene).
-
In postmenopausal women or women who have undergone oophorectomy, principal action in bone is to decrease the rate of bone resorption, thus slowing the rate of bone loss.
-
Inhibits estradiol-dependent proliferation of MCF-7 human mammary tumor cells in vitro.
Advice to Patients
-
Importance of providing patient a copy of manufacturer’s patient information.
-
Risk of venous thromboembolic events. Notify clinician if signs or symptoms of thromboembolic disorder occur. Avoid prolonged restrictions in movement while traveling. Discontinue raloxifene ≥72 hours before and during prolonged immobilization (e.g., postsurgery recovery, prolonged bed rest).
-
Potential for increased incidence of hot flushes (flashes); drug is not effective in reducing hot flushes associated with estrogen deficiency.
-
When used for osteoporosis, importance of taking supplemental calcium and/or vitamin D if daily dietary intake is inadequate. Importance of weight-bearing exercise and modification of other risk factors for osteoporosis (e.g., smoking, alcohol intake) if needed.
-
When used to reduce the incidence of invasive breast cancer, advise patient regarding benefits and risks of therapy as well as appropriate indications. Need for regular breast examinations and mammograms.
-
Importance for women who are or may become pregnant or who are lactating to avoid taking the drug.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.
-
Importance of informing patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
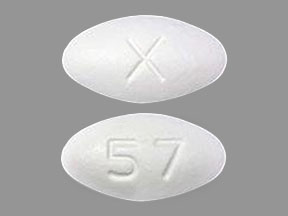
Oral |
Tablets, film-coated |
60 mg* |
Evista |
Lilly |
|
Raloxifene Hydrochloride Tablets |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions November 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Frequently asked questions
More about raloxifene
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (18)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Drug class: hormones/antineoplastics
- En español