Oxaprozin (Monograph)
Brand name: Daypro
Drug class: Reversible COX-1/COX-2 Inhibitors
Warning
- Cardiovascular Risk
-
Increased risk of serious (sometimes fatal) cardiovascular thrombotic events (e.g., MI, stroke).1 500 502 508 Risk may occur early in treatment and may increase with duration of use.500 502 505 506 508 (See Cardiovascular Thrombotic Effects under Cautions.)
-
Contraindicated in the setting of CABG surgery.508
- GI Risk
-
Increased risk of serious (sometimes fatal) GI events (e.g., bleeding, ulceration, perforation of the stomach or intestine).1 Serious GI events can occur at any time and may not be preceded by warning signs and symptoms.1 Geriatric individuals are at greater risk for serious GI events.1 (See GI Effects under Cautions.)
Introduction
Prototypical NSAIA;1 2 3 4 5 6 7 8 propionic acid derivative.1 2 3 4 5 6 7 8
Uses for Oxaprozin
Consider potential benefits and risks of oxaprozin therapy as well as alternative therapies before initiating therapy with the drug.1 Use lowest effective dosage and shortest duration of therapy consistent with the patient’s treatment goals.1
Inflammatory Diseases
Symptomatic treatment of osteoarthritis and rheumatoid arthritis.1 2 3
Management of juvenile rheumatoid arthritis in children 6-16 years of age.1
Oxaprozin Dosage and Administration
General
-
Consider potential benefits and risks of oxaprozin therapy as well as alternative therapies before initiating therapy with the drug.1
Administration
Oral Administration
Administer orally once daily;1 2 3 6 7 divided doses may improve tolerance in some patients.1
Dosage
To minimize the potential risk of adverse cardiovascular and/or GI events, use lowest effective dosage and shortest duration of therapy consistent with the patient’s treatment goals.1 Adjust dosage based on individual requirements and response; attempt to titrate to lowest effective dosage.1
Pediatric Patients
Inflammatory Disease
Juvenile Rheumatoid Arthritis
Oral|
Weight (kg) |
Dosage |
|---|---|
|
22–31 |
600 mg once daily |
|
32–54 |
900 mg once daily |
|
≥55 |
1.2 g once daily |
Adults
Inflammatory Diseases
Osteoarthritis or Rheumatoid Arthritis
OralInitially, 1.2 g once daily.1 2 3 Reserve long-term use of dosages >1.2 g daily for adults with severe disease who weigh >50 kg, have normal renal and hepatic function, and low risk for GI toxicity.1
If rapid onset of action needed, administer one-time loading dose of 1.2–1.8 g (up to 26 mg/kg).1
Patients with low body weight: Initially, 600 mg once daily.1 May increase to 1.2 g daily if needed.1
Prescribing Limits
Pediatric Patients
Juvenile Rheumatoid Arthritis
Oral
Doses >1.2 g daily not studied.1
Adults
Inflammatory Diseases
Osteoarthritis or Rheumatoid Arthritis
OralMaximum 1.8 g or 26 mg/kg daily (whichever is lower).1 Maximum loading dose is 26 mg/kg.1
Special Populations
Renal Impairment
Severe renal impairment and in those undergoing hemodialysis: Initially, 600 mg once daily.1 3 8 May increase to 1.2 g daily if needed.1 8 Supplemental doses after hemodialysis not needed.1
Hepatic Impairment
Dosage adjustment not needed in patients with well-compensated cirrhosis.1 2 3
Geriatric Patients
Dosage adjustment may be necessary in patients with low body weight, decreased renal function, or age-related concomitant disease.1
Cautions for Oxaprozin
Contraindications
-
Known hypersensitivity to oxaprozin or any ingredient in the formulation.1
-
History of asthma, urticaria, or other sensitivity reaction precipitated by aspirin or other NSAIAs.1
-
In the setting of CABG surgery.508
Warnings/Precautions
Warnings
Cardiovascular Thrombotic Effects
NSAIAs (selective COX-2 inhibitors, prototypical NSAIAs) increase the risk of serious adverse cardiovascular thrombotic events (e.g., MI, stroke) in patients with or without cardiovascular disease or risk factors for cardiovascular disease.500 502 508
Findings of FDA review of observational studies, meta-analysis of randomized controlled trials, and other published information500 501 502 indicate that NSAIAs may increase the risk of such events by 10–50% or more, depending on the drugs and dosages studied.500
Relative increase in risk appears to be similar in patients with or without known underlying cardiovascular disease or risk factors for cardiovascular disease, but the absolute incidence of serious NSAIA-associated cardiovascular thrombotic events is higher in those with cardiovascular disease or risk factors for cardiovascular disease because of their elevated baseline risk.500 502 506 508
Increased risk may occur early (within the first weeks) following initiation of therapy and may increase with higher dosages and longer durations of use.500 502 505 506 508
In controlled studies, increased risk of MI and stroke observed in patients receiving a selective COX-2 inhibitor for analgesia in first 10–14 days following CABG surgery.508
In patients receiving NSAIAs following MI, increased risk of reinfarction and death observed beginning in the first week of treatment.505 508
Increased 1-year mortality rate observed in patients receiving NSAIAs following MI;500 508 511 absolute mortality rate declined somewhat after the first post-MI year, but the increased relative risk of death persisted over at least the next 4 years.508 511
Some systematic reviews of controlled observational studies and meta-analyses of randomized studies suggest naproxen may be associated with lower risk of cardiovascular thrombotic events compared with other NSAIAs.11 12 13 500 501 502 503 506 FDA states that limitations of these studies and indirect comparisons preclude definitive conclusions regarding relative risks of NSAIAs.500
Use NSAIAs with caution and careful monitoring (e.g., monitor for development of cardiovascular events throughout therapy, even in those without prior cardiovascular symptoms) and at the lowest effective dosage for the shortest duration necessary.1 500 508
Some clinicians suggest that it may be prudent to avoid NSAIA use, whenever possible, in patients with cardiovascular disease.505 511 512 516 Avoid use in patients with recent MI unless benefits of therapy are expected to outweigh risk of recurrent cardiovascular thrombotic events; if used, monitor for cardiac ischemia.508 Contraindicated in the setting of CABG surgery.508
No consistent evidence that concomitant use of low-dose aspirin mitigates the increased risk of serious adverse cardiovascular events.1 502 508 (See Specific Drugs under Interactions.)
GI Effects
Serious GI toxicity (e.g., bleeding, ulceration, perforation) can occur with or without warning symptoms; increased risk in those with a history of GI bleeding or ulceration, geriatric patients, smokers, those with alcohol dependence, and those in poor general health.1
For patients at high risk for complications from NSAIA-induced GI ulceration (e.g., bleeding, perforation), consider concomitant use of misoprostol;c d e f alternatively, consider concomitant use of proton pump inhibitor (e.g., omeprazole)c d e or use of an NSAIA that is a selective inhibitor of COX-2 (e.g., celecoxib).e
Hypertension
Hypertension and worsening of preexisting hypertension reported; either event may contribute to the increased incidence of cardiovascular events.1 Use with caution in patients with hypertension; monitor BP.1
Impaired response to ACE inhibitors, angiotensin II receptor antagonists, β-blockers, and certain diuretics may occur.1 508 (See Specific Drugs under Interactions.)
Heart Failure and Edema
Fluid retention and edema reported.1 508
NSAIAs (selective COX-2 inhibitors, prototypical NSAIAs) may increase morbidity and mortality in patients with heart failure.500 501 504 507 508
NSAIAs may diminish cardiovascular effects of diuretics, ACE inhibitors, or angiotensin II receptor antagonists used to treat heart failure or edema.508 (See Specific Drugs under Interactions.)
Manufacturer recommends avoiding use in patients with severe heart failure unless benefits of therapy are expected to outweigh risk of worsening heart failure; if used, monitor for worsening heart failure.508
Some experts recommend avoiding use, whenever possible, in patients with reduced left ventricular ejection fraction and current or prior symptoms of heart failure.507
Renal Effects
Direct renal injury, including renal papillary necrosis, reported in patients receiving long-term NSAIA therapy.1
Potential for overt renal decompensation.1 Increased risk of renal toxicity in patients with renal or hepatic impairment or heart failure, in geriatric patients, in patients with volume depletion, and in those receiving a diuretic, ACE inhibitor, or angiotensin II receptor antagonist.1 b
Sensitivity Reactions
Hypersensitivity
Anaphylactoid reactions (e.g., anaphylaxis, angioedema) reported.1 Immediate medical intervention and discontinuance for anaphylaxis.1
Avoid in patients with aspirin triad (aspirin sensitivity, asthma, nasal polyps); caution in patients with asthma.1
Potentially fatal or life-threatening syndrome of multi-organ hypersensitivity (i.e., drug reaction with eosinophilia and systemic symptoms [DRESS]) reported in patients receiving NSAIAs.1202 Clinical presentation is variable, but typically includes eosinophilia, fever, rash, lymphadenopathy, and/or facial swelling, possibly associated with other organ system involvement (e.g., hepatitis, nephritis, hematologic abnormalities, myocarditis, myositis).1202 Symptoms may resemble those of acute viral infection.1202 Early manifestations of hypersensitivity (e.g., fever, lymphadenopathy) may be present in the absence of rash.1202 If signs or symptoms of DRESS develop, discontinue the NSAIA and immediately evaluate the patient.1202
Dermatologic Reactions
Serious skin reactions (e.g., exfoliative dermatitis, Stevens-Johnson syndrome, toxic epidermal necrolysis) reported; can occur without warning.1 Discontinue at first appearance of rash or any other signs of hypersensitivity (e.g., blisters, fever, pruritus).1
Photosensitivity
Rash on sun-exposed areas of the body reported.1
General Precautions
Hepatic Effects
Severe reactions including jaundice, fatal fulminant hepatitis, liver necrosis, and hepatic failure (sometimes fatal) reported rarely with NSAIAs.1
Elevations of serum ALT or AST reported.1
Monitor for symptoms and/or signs suggesting liver dysfunction; monitor abnormal liver function test results.1 Discontinue if signs or symptoms of liver disease or systemic manifestation (e.g., eosinophilia, rash) occur or if liver function test abnormalities persist or worsen.1
Hematologic Effects
Anemia reported rarely.1 Determine hemoglobin concentration or hematocrit in patients receiving long-term therapy if signs or symptoms of anemia occur.1
May inhibit platelet aggregation and prolong bleeding time.1
Other Precautions
Not a substitute for corticosteroid therapy; not effective in the management of adrenal insufficiency.1
May mask certain signs of infection.1
Obtain CBC and chemistry profile periodically during long-term use.1
Specific Populations
Pregnancy
Use of NSAIAs during pregnancy at about ≥30 weeks’ gestation can cause premature closure of the fetal ductus arteriosus; use at about ≥20 weeks’ gestation associated with fetal renal dysfunction resulting in oligohydramnios and, in some cases, neonatal renal impairment.1200 1202
Effects of NSAIAs on the human fetus during third trimester of pregnancy include prenatal constriction of the ductus arteriosus, tricuspid incompetence, and pulmonary hypertension; nonclosure of the ductus arteriosus during the postnatal period (which may be resistant to medical management); and myocardial degenerative changes, platelet dysfunction with resultant bleeding, intracranial bleeding, renal dysfunction or renal failure, renal injury or dysgenesis potentially resulting in prolonged or permanent renal failure, oligohydramnios, GI bleeding or perforation, and increased risk of necrotizing enterocolitis.1202
Avoid use of NSAIAs in pregnant women at about ≥30 weeks’ gestation; if use required between about 20 and 30 weeks’ gestation, use lowest effective dosage and shortest possible duration of treatment, and consider monitoring amniotic fluid volume via ultrasound examination if treatment duration >48 hours; if oligohydramnios occurs, discontinue drug and follow up according to clinical practice.1200 1202 (See Advice to Patients.)
Fetal renal dysfunction resulting in oligohydramnios and, in some cases, neonatal renal impairment observed, on average, following days to weeks of maternal NSAIA use; infrequently, oligohydramnios observed as early as 48 hours after initiation of NSAIAs.1200 1202 Oligohydramnios is often, but not always, reversible (generally within 3–6 days) following NSAIA discontinuance.1200 1202 Complications of prolonged oligohydramnios may include limb contracture and delayed lung maturation.1200 1202 In limited number of cases, neonatal renal dysfunction (sometimes irreversible) occurred without oligohydramnios.1200 1202 Some neonates have required invasive procedures (e.g., exchange transfusion, dialysis).1200 1202 Deaths associated with neonatal renal failure also reported.1200 Limitations of available data (lack of control group; limited information regarding dosage, duration, and timing of drug exposure; concomitant use of other drugs) preclude a reliable estimate of the risk of adverse fetal and neonatal outcomes with maternal NSAIA use.1202 Available data on neonatal outcomes generally involved preterm infants; extent to which risks can be generalized to full-term infants is uncertain.1202
Animal data indicate important roles for prostaglandins in kidney development and endometrial vascular permeability, blastocyst implantation, and decidualization.1201 In animal studies, inhibitors of prostaglandin synthesis increased pre- and post-implantation losses; also impaired kidney development at clinically relevant doses.1201
No adequate and well-controlled studies of oxaprozin in pregnant women.1201 In animal studies, teratogenicity observed in rabbits, but no evidence of teratogenicity or embryotoxicity observed in mice or rats.1201 Failure to deliver and a reduction in live birth index observed in rats.1201
Effects of oxaprozin on labor and delivery not known.1201 In animal studies, NSAIAs delayed parturition and increased stillbirths.1201
Lactation
Distributed into milk in rats; not known whether distributed into human milk.1 Discontinue nursing or the drug.1
Fertility
NSAIAs may be associated with reversible infertility in some women.1201 Reversible delays in ovulation observed in limited studies in women receiving NSAIAs; animal studies indicate that inhibitors of prostaglandin synthesis can disrupt prostaglandin-mediated follicular rupture required for ovulation.1201
Consider withdrawal of NSAIAs in women experiencing difficulty conceiving or undergoing evaluation of infertility.1201
Testicular degeneration with oxaprozin administration observed in dogs, but not confirmed in other species; clinical relevance not known.1201
Pediatric Use
Safety and efficacy not established in children <6 years of age.1
Safety and efficacy in pediatric patients 6–16 years of age with juvenile rheumatoid arthritis supported by studies in adults with rheumatoid arthritis and by safety and pharmacokinetic data from trials in children with juvenile rheumatoid arthritis.1
Geriatric Use
No overall differences in efficacy or safety were observed between geriatric and younger adults.1 Possibility exists of greater sensitivity in some geriatric individuals.1
Caution advised.1 Geriatric adults appear to tolerate NSAIA-induced adverse effects less well than younger individuals.1
Select dosage with caution because of age-related decreases in renal function.1 May be useful to monitor renal function.1
Hepatic Impairment
Use with caution in patients with severe hepatic impairment.1
Renal Impairment
Use not recommended in patients with advanced renal disease; close monitoring of renal function advised if used.1 Dosage adjustment needed.1 (See Renal Impairment under Dosage and Administration.)
Common Adverse Effects
Abdominal pain, anorexia, constipation, diarrhea, flatulence, GI ulcers, GI bleeding/perforation, dyspepsia, heartburn, nausea, vomiting, renal function abnormalities, anemia, confusion, depression, sleep disturbance, dizziness, dysuria or increased frequency, edema, liver function test abnormalities, headache, prolonged bleeding time, pruritus, rash, sedation, somnolence, tinnitus.1
Drug Interactions
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
ACE inhibitors |
Reduced BP response to ACE inhibitor 1 |
Monitor BP1 |
|
Acetaminophen |
Pharmacokinetic interaction unlikely1 |
|
|
Angiotensin II receptor antagonists |
Reduced BP response to angiotensin II receptor antagonistb |
Monitor BPb |
|
Antacids |
Change in oxaprozin bioavailability unlikely1 |
|
|
Aspirin |
Increased risk of GI ulceration and other complications1 No consistent evidence that low-dose aspirin mitigates the increased risk of serious cardiovascular events associated with NSAIAs 1 502 508 a Possible pharmacokinetic interaction (altered plasma protein binding)1 |
Manufacturer states that concomitant use not recommended1 |
|
β-Adrenergic blocking agents |
Reduced BP response to metoprolol reported1 |
Monitor BP1 |
|
Diuretics (furosemide, thiazides) |
Reduced natriuretic effects possible1 |
Monitor for diuretic efficacy and renal failure1 |
|
Estrogens, conjugated |
Pharmacokinetic interaction unlikely1 |
|
|
Glyburide |
Pharmacokinetic interaction; no effect on hypoglycemic effects1 |
Monitor blood glucose if concomitant therapy initiated1 |
|
Histamine H2-receptor antagonists (cimetidine, ranitidine) |
Decreased clearance of oxaprozin1 |
|
|
Lithium |
Increased plasma lithium concentrations 1 |
Monitor for lithium toxicity1 |
|
Methotrexate |
Possible toxicity associated with increased plasma methotrexate concentration1 |
Caution advised1 |
|
Pemetrexed |
Possible increased risk of pemetrexed-associated myelosuppression, renal toxicity, and GI toxicity1201 |
Short half-life NSAIAs (e. g., diclofenac, indomethacin): Avoid administration beginning 2 days before and continuing through 2 days after pemetrexed administration1201 Longer half-life NSAIAs (e.g., meloxicam, nabumetone): In the absence of data, avoid administration beginning at least 5 days before and continuing through 2 days after pemetrexed administration1201 Patients with Clcr 45–79 mL/minute: Monitor for myelosuppression, renal toxicity, and GI toxicity1201 |
|
Warfarin |
Possibility of bleeding complications1 |
Caution advised1 |
Oxaprozin Pharmacokinetics
Absorption
Bioavailability
Well absorbed following oral administration.1
Food
Food may reduce the rate of absorption, but does not affect extent of absorption.1 2 3 4 6
Distribution
Extent
Distributed into synovial tissues in patients with rheumatoid arthritis.1
Plasma Protein Binding
99% (mainly albumin).1
Elimination
Metabolism
Metabolized, principally in the liver, to inactive metabolites.1
Elimination Route
Excreted in urine (65%) and in feces (35%) as metabolites; approximately 5% is excreted in urine as unchanged drug.1
Half-life
Approximately 38–44 hours.1
Special Populations
Renal clearance decreased in patients with renal impairment; renal clearance contributes minimally to excretion of oxaprozin.1 Not removed by hemodialysis or continuous ambulatory peritoneal dialysis (CAPD).1
Stability
Storage
Oral
Tablets
Tight, light resistant containers at 25°C (may be exposed to 15–30°C).1
Actions
-
Inhibits cyclooxygenase-1 (COX-1) and COX-2.1
-
Pharmacologic actions similar to those of other prototypical NSAIAs; exhibits anti-inflammatory, analgesic, and antipyretic activity.1
Advice to Patients
-
Importance of reading the medication guide for NSAIAs that is provided each time the drug is dispensed.1
-
Risk of serious cardiovascular events (e.g., MI, stroke).1 500 508
-
Risk of GI toxicity and ulceration.1
-
Risk of serious skin reactions,1 DRESS,1202 and anaphylactoid and other sensitivity reactions.1
-
Risk of hepatotoxicity.1
-
Importance of seeking immediate medical attention if signs and symptoms of a cardiovascular event (chest pain, dyspnea, weakness, slurred speech) occur.1 500 508
-
Importance of notifying clinician if signs and symptoms of GI ulceration or bleeding, unexplained weight gain, or edema develops.1
-
Advise patients to stop taking the drug immediately if they develop any type of rash or fever and to promptly contact their clinician.1202 Importance of seeking immediate medical attention if an anaphylactic reaction occurs.1
-
Importance of discontinuing therapy and contacting clinician immediately if signs and symptoms of hepatotoxicity (nausea, fatigue, lethargy, pruritus, jaundice, upper right quadrant tenderness, flu-like symptoms) occur.1
-
Risk of heart failure or edema; importance of reporting dyspnea, unexplained weight gain, or edema.508
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.1
-
Importance of avoiding NSAIA use beginning at 20 weeks’ gestation unless otherwise advised by a clinician; importance of avoiding NSAIAs beginning at 30 weeks’ gestation because of risk of premature closure of the fetal ductus arteriosus; monitoring for oligohydramnios may be necessary if NSAIA therapy required for >48 hours’ duration between about 20 and 30 weeks’ gestation.1200 1202
-
Advise women who are trying to conceive that NSAIAs may be associated with a reversible delay in ovulation.1201
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant diseases.1
-
Importance of informing patients of other important precautionary information.1 (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
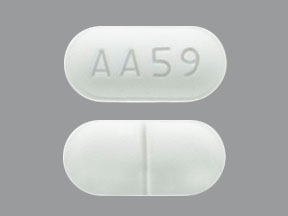
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
600 mg* |
Daypro (scored) |
Searle |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
References
1. Searle. Daypro (oxaprozin) caplets prescribing information. New York, NY; 2006 Mar.
2. Miller LG. Oxaprozin: a once-daily nonsteroidal anti- inflammatory drug. Clin Pharm. 1992; 11:591-603. https://pubmed.ncbi.nlm.nih.gov/1617910
3. Todd PA, Brogden RN. Oxaprozin: a preliminary review of its pharmacodynamic and pharmacokinetic properties, and therapeutic efficacy. Drugs. 1986; 32:291-312. https://pubmed.ncbi.nlm.nih.gov/3536423
4. Chiang ST, Knowles JA, Hubsher JA et al. Effects of food on oxaprozin bioavailability. J Clin Pharmacol. 1984; 24:381-5. https://pubmed.ncbi.nlm.nih.gov/6480879
5. Lewis AJ, Carlson RP, Chang J et al. The pharmacological profile of oxaprozin, an antiinflammatory and analgesic agent with low gastrointestinal toxicity. Curr Ther Res. 1983; 34:777-94.
6. Janssen FW, Chiang ST, Walker BR et al. Disposition of oxaprozin in healthy subjects and certain disease states. Curr Ther Res. 1984; 35:363-76.
7. Greenblatt DJ, Matlis R, Scavone JM et al. Oxaprozin pharmacokinetics in the elderly. Br J Clin Pharmacol. 1985; 19:373-8. https://pubmed.ncbi.nlm.nih.gov/3986088 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1463728/
8. Chiang ST, Morrison G, Knowles JA et al. Oxaprozin disposition in renal disease. Clin Pharmacol Ther. 1982; 31:509-15. https://pubmed.ncbi.nlm.nih.gov/7060332
9. Searle. Skokie, IL: Personal communication.
11. McGettigan P, Henry D. Cardiovascular risk and inhibition of cyclooxygenase: a systematic review of observational studies of selective and nonselective inhibitors of cyclooxygenase 2. JAMA. 2006; 296: 1633-44. https://pubmed.ncbi.nlm.nih.gov/16968831
12. Kearney PM, Baigent C, Godwin J et al. Do selective cyclo-oxygenase-2 inhibitors and traditional non-steroidal anti-inflammatory drugs increase the risk of atherothrombosis? Meta-analysis of randomised trials. BMJ. 2006; 332: 1302-5. https://pubmed.ncbi.nlm.nih.gov/16740558 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1473048/
13. Graham DJ. COX-2 inhibitors, other NSAIDs, and cardiovascular risk; the seduction of common sense. JAMA. 2006; 296:1653-6. https://pubmed.ncbi.nlm.nih.gov/16968830
500. Food and Drug Administration. Drug safety communication: FDA strengthens warning that non-aspirin nonsteroidal anti-inflammatory drugs (NSAIDs) can cause heart attacks or strokes. Silver Spring, MD; 2015 Jul 9. From the FDA web site. Accessed 2016 Mar 22. http://www.fda.gov/Drugs/DrugSafety/ucm451800.htm
501. Coxib and traditional NSAID Trialists' (CNT) Collaboration, Bhala N, Emberson J et al. Vascular and upper gastrointestinal effects of non-steroidal anti-inflammatory drugs: meta-analyses of individual participant data from randomised trials. Lancet. 2013; 382:769-79. https://pubmed.ncbi.nlm.nih.gov/23726390 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3778977/
502. Food and Drug Administration. FDA briefing document: Joint meeting of the arthritis advisory committee and the drug safety and risk management advisory committee, February 10-11, 2014. From FDA web site http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/ArthritisAdvisoryCommittee/UCM383180.pdf
503. Trelle S, Reichenbach S, Wandel S et al. Cardiovascular safety of non-steroidal anti-inflammatory drugs: network meta-analysis. BMJ. 2011; 342:c7086. https://pubmed.ncbi.nlm.nih.gov/21224324 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3019238/
504. Gislason GH, Rasmussen JN, Abildstrom SZ et al. Increased mortality and cardiovascular morbidity associated with use of nonsteroidal anti-inflammatory drugs in chronic heart failure. Arch Intern Med. 2009; 169:141-9. https://pubmed.ncbi.nlm.nih.gov/19171810
505. Schjerning Olsen AM, Fosbøl EL, Lindhardsen J et al. Duration of treatment with nonsteroidal anti-inflammatory drugs and impact on risk of death and recurrent myocardial infarction in patients with prior myocardial infarction: a nationwide cohort study. Circulation. 2011; 123:2226-35. https://pubmed.ncbi.nlm.nih.gov/21555710
506. McGettigan P, Henry D. Cardiovascular risk with non-steroidal anti-inflammatory drugs: systematic review of population-based controlled observational studies. PLoS Med. 2011; 8:e1001098. https://pubmed.ncbi.nlm.nih.gov/21980265 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3181230/
507. Yancy CW, Jessup M, Bozkurt B et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013; 62:e147-239. https://pubmed.ncbi.nlm.nih.gov/23747642
508. Pfizer. Daypro (oxaprozin) caplets prescribing information. New York, NY; 2016 May.
511. Olsen AM, Fosbøl EL, Lindhardsen J et al. Long-term cardiovascular risk of nonsteroidal anti-inflammatory drug use according to time passed after first-time myocardial infarction: a nationwide cohort study. Circulation. 2012; 126:1955-63. https://pubmed.ncbi.nlm.nih.gov/22965337
512. Olsen AM, Fosbøl EL, Lindhardsen J et al. Cause-specific cardiovascular risk associated with nonsteroidal anti-inflammatory drugs among myocardial infarction patients--a nationwide study. PLoS One. 2013; 8:e54309.
516. Bavry AA, Khaliq A, Gong Y et al. Harmful effects of NSAIDs among patients with hypertension and coronary artery disease. Am J Med. 2011; 124:614-20. https://pubmed.ncbi.nlm.nih.gov/21596367 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4664475/
1200. US Food and Drug Administration. FDA drug safety communication: FDA recommends avoiding use of NSAIDs in pregnancy at 20 weeks or later because they can result in low amniotic fluid. 2020 Oct 15. From the FDA website. https://www.fda.gov/drugs/drug-safety-and-availability/fda-recommends-avoiding-use-nsaids-pregnancy-20-weeks-or-later-because-they-can-result-low-amniotic
1201. Pfizer. Daypro (oxaprozin) caplets prescribing information. New York, NY; 2020 Dec.
1202. Actavis Pharma. Sulindac tablets prescribing information. Parsippany, NJ; 2020 Oct.
a. Food and Drug Administration. Analysis and recommendations for agency action regarding non-steroidal anti-inflammatory drugs and cardiovascular risk. 2005 Apr 6.
b. Merck & Co. Clinoril (sulindac) tablets prescribing information. Whitehouse Station, NJ; 2006 Feb.
c. Anon. Drugs for rheumatoid arthritis. Med Lett Drugs Ther. 2000; 42:57-64. https://pubmed.ncbi.nlm.nih.gov/10887424
d. Wolfe MM, Lichtenstein DR, Singh G. Gastrointestinal toxicity of nonsteroidal antiinflammatory drugs. N Engl J Med. 1999; 340:1888-99. https://pubmed.ncbi.nlm.nih.gov/10369853
e. American College of Rheumatology Subcommittee on Rheumatoid Arthritis Guidelines. Guidelines for the management of rheumatoid arthritis: 2002 update. Arthritis Rheum. 2002; 46:328-46. https://pubmed.ncbi.nlm.nih.gov/11840435
f. Lanza Fl, and the members of the Ad Hoc Committee on Practice Parameters of the American College of Gastroenterology. A guideline for the treatment and prevention of NSAID-induced ulcers. Am J Gastroenterol. 1998; 93:2037-46. https://pubmed.ncbi.nlm.nih.gov/9820370
Related/similar drugs
More about oxaprozin
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (8)
- Drug images
- Latest FDA alerts (4)
- Side effects
- Dosage information
- During pregnancy
- Drug class: Nonsteroidal anti-inflammatory drugs
- Breastfeeding