Olaparib (Monograph)
Brand name: Lynparza
Drug class: Antineoplastic Agents
Introduction
Antineoplastic agent; inhibitor of poly(adenosine diphosphate [ADP]-ribose) polymerase (PARP).
Uses for Olaparib
Ovarian Cancer
Used as a single agent for the maintenance treatment of adults with confirmed or suspected deleterious germline or somatic BRCA-mutated advanced epithelial ovarian, fallopian tube, or primary peritoneal cancer who are in complete or partial response to first-line platinum-based chemotherapy; designated an orphan drug by FDA for this use. FDA-approved companion diagnostic test required to confirm presence of specific biomarkers prior to initiation of therapy.
Used in combination with bevacizumab for the maintenance treatment of adults with advanced epithelial ovarian, fallopian tube, or primary peritoneal cancer who are in complete or partial response to first-line platinum-based chemotherapy and whose cancer is associated with homologous recombination deficiency (HRD)-positive status (defined by a confirmed or suspected deleterious BRCA mutation and/or genomic instability); designated an orphan drug by FDA for this use. FDA-approved companion diagnostic test required to confirm presence of specific biomarkers prior to initiation of therapy.
Used as a single agent for the maintenance treatment of adults with confirmed or suspected deleterious germline or somatic BRCA-mutated recurrent epithelial ovarian, fallopian tube, or primary peritoneal cancer who are in complete or partial response to platinum-based chemotherapy designated an orphan drug by FDA for this use. FDA-approved companion diagnostic test required to confirm presence of specific biomarkers prior to initiation of therapy.
Guidelines from the American Society of Clinical Oncology (ASCO) state that patients with newly diagnosed stage III or IV epithelial ovarian cancer in complete or partial response to first-line platinum-based chemotherapy should be offered PARP inhibitors as maintenance therapy in the presence of high-grade serous or endometroid ovarian cancer. Options for patients with germline or somatic pathogenic or likely pathogenic variants in BRCA1 or BRCA2 include olaparib, niraparib, or rucaparib.
For recurrent ovarian cancer, ASCO states that PARP inhibitor monotherapy may be used for second-line or greater maintenance treatment in PARP inhibitor-naïve patients with epithelial ovarian cancer who have responded to platinum-based regimens, regardless of BRCA mutation status. However, FDA-labeled use for olaparib maintenance therapy in recurrent ovarian cancer is restricted to patients with a tumor BRCA mutation.
Breast Cancer
Used as adjuvant treatment in adults with confirmed or suspected deleterious germline BRCA-mutated, human epidermal growth factor receptor type 2 (HER2)-negative high-risk early breast cancer who have been treated with neoadjuvant or adjuvant chemotherapy. FDA-approved companion diagnostic test required to confirm presence of specific biomarkers prior to initiation of therapy.
Used as a single agent for the treatment of adults with confirmed or suspected deleterious germline BRCA-mutated, HER2-negative metastatic breast cancer previously treated with chemotherapy in the neoadjuvant, adjuvant, or metastatic setting. Patients with hormone receptor-positive breast cancer should have received prior endocrine therapy, unless clinically inappropriate. FDA-approved companion diagnostic test required to confirm presence of specific biomarkers prior to initiation of therapy.
Treatment of early breast cancer typically involves surgery; systemic therapies may be administered preoperatively (neoadjuvant) or postoperatively (adjuvant), depending on factors such as stage, grade, and molecular status of the tumor. Specific role for olaparib in early breast cancer not yet established.
Guidelines from ASCO state that patients with metastatic hormone receptor-positive, HER2-negative breast cancer with germline BRCA1 or BRCA2 mutations who are no longer benefiting from endocrine therapy may be offered an oral PARP inhibitor in the first- through third-line setting rather than chemotherapy. Patients with metastatic triple-negative breast cancer with germline BRCA1 or BRCA2 mutations who have previously been treated with chemotherapy in the neoadjuvant, adjuvant, or metastatic setting may be offered an oral PARP inhibitor (olaparib or talazoparib) rather than chemotherapy.
Pancreatic Adenocarcinoma
Used as a single agent for the first-line maintenance treatment of adults with confirmed or suspected deleterious germline BRCA-mutated metastatic pancreatic adenocarcinoma whose disease has not progressed on at least 16 weeks of a first-line platinum-based chemotherapy regimen; designated an orphan drug by FDA for this use. FDA-approved companion diagnostic test required to confirm presence of specific biomarkers prior to initiation of therapy.
ASCO states that olaparib is recommended as an option for maintenance therapy for patients with metastatic pancreatic cancer harboring an identified germline BRCA mutation; decision to continue chemotherapy or switch to maintenance therapy with olaparib should be based on patient preference and consideration of response to chemotherapy, cumulative toxicities associated with chemotherapy, convenience, toxicity, goals of care, cost, and clinical evidence (e.g., lack of overall survival benefit).
Prostate Cancer
Used as a single agent for the treatment of adults with confirmed or suspected deleterious germline or somatic homologous recombination repair (HRR) gene-mutated metastatic castration-resistant prostate cancer who have progressed following prior treatment with enzalutamide or abiraterone. FDA-approved companion diagnostic test required to confirm presence of specific biomarkers prior to initiation of therapy.
Used in combination with abiraterone and prednisone or prednisolone for the treatment of adults with confirmed or suspected deleterious BRCA-mutated metastatic castration-resistant prostate cancer. FDA-approved companion diagnostic test required to confirm presence of specific biomarkers prior to initiation of therapy.
American Urological Association (AUA) recommends offering a PARP inhibitor to patients with confirmed or suspected deleterious germline or somatic HRR gene-mutated (including BRCA-mutated) metastatic castration-resistant prostate cancer following prior treatment with enzalutamide or abiraterone acetate, and/or a taxane-based chemotherapy.
Olaparib Dosage and Administration
General
Pretreatment Screening
-
Obtain CBC at baseline.
-
Do not initiate therapy in patients with grade 2 or greater hematologic toxicity caused by previous chemotherapy.
-
Perform pregnancy testing in females of reproductive potential.
-
Confirm presence of specific biomarkers prior to initiation of therapy for certain indications (see Table 1). Consult FDA website for list of FDA-approved companion diagnostic tests ([Web]).
If testing fails or tissue sample is unavailable/insufficient, or when germline testing is negative, consider using an alternative test, if available
|
Indication |
Biomarker |
Sample Type |
|---|---|---|
|
First-line maintenance treatment of germline or somatic BRCA-mutated advanced ovarian cancer |
BRCA1m, BRCA2m |
Tumor, blood |
|
First-line maintenance treatment of HRD-positive advanced ovarian cancer in combination with bevacizumab |
BRCA1m, BRCA2m and/or genomic instability |
Tumor |
|
Maintenance treatment of germline or somatic BRCA-mutated recurrent ovarian cancer |
BRCA1m, BRCA2m |
Tumor, blood |
|
Adjuvant treatment of germline BRCA-mutated, HER2-negative high-risk early breast cancer |
Germline BRCA1m, germline BRCA2m |
Blood |
|
Germline BRCA-mutated, HER2-negative metastatic breast cancer |
Germline BRCA1m, germline BRCA2m |
Blood |
|
First-line maintenance treatment of germline BRCA-mutated metastatic pancreatic adenocarcinoma |
Germline BRCA1m, germline BRCA2m |
Blood |
|
Germline or somatic HRR gene-mutated metastatic castration-resistant prostate cancer |
ATMm, BRCA1m, BRCA2m, BARD1m, BRIP1m, CDK12m, CHEK1m, CHEK2m, FANCLm, PALB2m, RAD51Bm, RAD51Cm, RAD51Dm, RAD54Lm |
Tumor |
|
Germline BRCA1m, germline BRCA2m |
Blood |
|
|
ATMm, BRCA1m, BRCA2m |
Plasma (circulating tumor DNA) |
|
|
BRCA-mutated metastatic castration-resistant prostate cancer in combination with abiraterone and prednisone or prednisolone |
BRCA1m, BRCA2m |
Tumor, blood, plasma (circulating tumor DNA) |
Patient Monitoring
-
Monitor CBC monthly during therapy.
-
Monitor for signs or symptoms of venous thrombosis and pulmonary embolism.
Other General Considerations
-
Tachyphylaxis of nausea symptoms usually occurs during the first cycle of PARP inhibitor therapy, often without antiemetic therapy or dose reduction.
-
A light meal or snack prior to each dose of a PARP inhibitor may mitigate nausea.
-
If persistent nausea/vomiting, weight loss >5%, and/or reduction in performance status occurs in the absence of other etiology (e.g., bowel obstruction), ASCO recommends temporarily withholding therapy followed by dosage reduction.
Administration
Oral Administration
Administer orally twice daily with or without food.
Swallow tablets whole; do not chew, dissolve, crush, or divide.
Dosage
Adults
Ovarian Cancer
First-line Maintenance Treatment of BRCA-mutated Advanced Ovarian Cancer
Oral300 mg twice daily.
Continue therapy until disease progression or unacceptable toxicity occurs, or until 2 years of therapy are complete. Patients with a complete response at 2 years should discontinue therapy. Patients with evidence of disease at 2 years may continue therapy beyond 2 years if they may derive clinical benefit from an extended duration of therapy.
First-line Maintenance Treatment of HRD-positive Advanced Ovarian Cancer
Oral300 mg twice daily in combination with bevacizumab (15 mg/kg IV every 3 weeks).
Continue olaparib until disease progression or unacceptable toxicity occurs, or until 2 years of therapy are complete. Patients with a complete response at 2 years should discontinue therapy. Patients with evidence of disease at 2 years may continue olaparib beyond 2 years if they may derive clinical benefit from an extended duration of therapy.
Continue bevacizumab for a total of 15 months (including use during primary chemotherapy and maintenance treatment).
Maintenance Treatment of BCRA-mutated Recurrent Ovarian Cancer
Oral300 mg twice daily. Continue therapy until disease progression or unacceptable toxicity occurs.
Breast Cancer
Adjuvant Treatment of BRCA-mutated HER2-negative High-risk Early Breast Cancer
Oral300 mg twice daily. Continue therapy for 1 year, or until disease progression or unacceptable toxicity occurs.
Continue concomitant endocrine therapy in patients with hormone receptor-positive disease as recommended in clinical guidelines.
BRCA-mutated, HER2-negative Metastatic Breast Cancer
Oral300 mg twice daily. Continue therapy until disease progression or unacceptable toxicity occurs.
Pancreatic Adenocarcinoma
Oral
300 mg twice daily. Continue therapy until disease progression or unacceptable toxicity occurs.
Prostate Cancer
Treatment of Homologous Recombination Repair (HRR) Gene-mutated Metastatic Castration-resistant Prostate Cancer
Oral300 mg twice daily. Continue therapy until disease progression or unacceptable toxicity occurs.
Use with a gonadotropin-releasing hormone (GnRH) analog in patients who have not previously undergone bilateral orchiectomy.
Treatment of BRCA-mutated Metastatic Castration-Resistant Prostate Cancer in Combination with Abiraterone and Prednisone or Prednisolone
Oral300 mg twice daily in combination with abiraterone 1000 mg once daily and prednisone or prednisolone 5 mg twice daily. Continue therapy until disease progression or unacceptable toxicity occurs.
Use with a GnRH analog in patients who have not previously undergone bilateral orchiectomy.
Dosage Modifications for Toxicity
Oral
If adverse reactions occur, consider interruption of therapy or dosage reduction.
If dosage reduction is necessary, reduce dosage to 250 mg twice daily.
If further reduction is necessary, reduce dosage to 200 mg twice daily.
Concomitant Use with Drugs Affecting Hepatic Microsomal Enzymes
Oral
Avoid concomitant use of moderate or potent inhibitors of CYP3A.
If concomitant use of a potent CYP3A inhibitor cannot be avoided, reduce olaparib dosage to 100 mg twice daily.
If concomitant use of a moderate CYP3A inhibitor cannot be avoided, reduce olaparib dosage to 150 mg twice daily.
If concomitant use of CYP3A inhibitor is discontinued, return olaparib dosage to the dosage used prior to initiation of the CYP3A inhibitor (after 3–5 terminal half-lives of the CYP3A inhibitor).
Special Populations
Hepatic Impairment
Mild to moderate hepatic impairment (Child-Pugh class A or B): No initial dosage adjustment necessary.
Severe hepatic impairment (Child-Pugh class C): Not studied; no specific dosage recommendation.
Renal Impairment
Mild renal impairment (Clcr 51–80 mL/minute): No initial dosage adjustment necessary.
Moderate renal impairment (Clcr 31–50 mL/minute): Reduce dosage to 200 mg twice daily.
Severe renal impairment or end-stage renal disease (Clcr ≤30 mL/minute): Not studied; no specific dosage recommendations.
Geriatric Patients
No specific dosage recommendations at this time.
Cautions for Olaparib
Contraindications
-
None.
Warnings/Precautions
Myelodysplastic Syndrome (MDS)/Acute Myeloid Leukemia (AML)
MDS and AML, sometimes fatal, reported. All patients with MDS/AML received previous chemotherapy with platinum-containing agents and/or other DNA-damaging antineoplastic agents, including radiation therapy. The median duration of therapy in patients who developed MDS/AML was 2 years, but duration ranged from <6 months to >4 years.
Monitor CBC at baseline and monthly thereafter. Delay initiation of therapy until patients have recovered to grade 1 or less from hematologic toxicity caused by previous chemotherapy.
If prolonged hematologic toxicity occurs during therapy, interrupt therapy and monitor CBC weekly until recovery to grade 1 or less.
If myelosuppression persists for >4 weeks following interruption of therapy, refer patient to a hematologist for further evaluation, including bone marrow analysis and cytogenetic testing of a blood sample. If MDS/AML is confirmed, discontinue therapy.
Pneumonitis
Pneumonitis, sometimes fatal, reported in 0.8% of patients.
If new or worsening pulmonary symptoms or a radiologic abnormality occurs, interrupt therapy and initiate prompt diagnostic evaluation. If pneumonitis is confirmed, discontinue therapy and treat appropriately.
Fetal/Neonatal Morbidity and Mortality
May cause fetal harm based on mechanism of action and animal findings; teratogenicity, embryotoxicity, and fetotoxicity demonstrated in animals.
Avoid pregnancy during therapy. Verify pregnancy status prior to initiating therapy. Females of reproductive potential should use effective contraceptive methods while receiving olaparib and for ≥6 months after drug is discontinued. Males with such female partners or partners who are pregnant should use effective contraceptive methods while receiving olaparib and for 3 months after the drug is discontinued. Males should be advised to refrain from donating sperm while receiving olaparib and for 3 months after the drug is discontinued. If used during pregnancy or patient becomes pregnant, apprise of potential fetal hazard and risk for loss of the pregnancy.
Venous Thromboembolic Events
Venous thromboembolic events (VTE), including PE, reported.
Monitor patients for signs and symptoms of venous thrombosis or PE. If venous thrombosis or PE occurs, treat patient as medically appropriate (e.g., long-term anticoagulation).
Specific Populations
Pregnancy
May cause fetal harm.
Verify pregnancy status prior to initiating olaparib.
Lactation
Not known whether olaparib is distributed into human milk. Avoid breast-feeding during olaparib therapy and for 1 month after the last dose of olaparib.
Females and Males of Reproductive Potential
May cause fetal harm if administered during pregnancy. Verify pregnancy status prior to initiating olaparib.
Advise females of reproductive potential to use effective contraceptive methods while receiving olaparib and for ≥6 months after the drug is discontinued.
Advise males with female partners of reproductive potential or partners who are pregnant to use effective contraceptive methods while receiving olaparib and for 3 months after the drug is discontinued.
Advise males to refrain from donating sperm while receiving olaparib and for 3 months after the drug is discontinued.
Pediatric Use
Safety and efficacy not established in pediatric patients.
Geriatric Use
In clinical studies in patients with advanced solid tumors receiving olaparib monotherapy, 23% were ≥65 years of age, 7% were ≥75 years of age, and 0.4% were ≥85 years of age.
In clinical studies in patients with advanced solid tumors receiving olaparib in combination with bevacizumab, 38% were ≥65 years of age and 6% were ≥75 years of age.
In clinical studies in patients with advanced solid tumors receiving olaparib in combination with abiraterone and prednisone or prednisolone, 67% were ≥65 years of age and 24% were ≥75 years of age.
No differences in overall safety or effectiveness were observed in these patients compared to younger patients.
Hepatic Impairment
Increased exposure observed in mild or moderate hepatic impairment (Child-Pugh class A and B); no initial dosage adjustment necessary.
Not studied in severe hepatic impairment (Child-Pugh class C).
Renal Impairment
Increased exposure observed in mild or moderate renal impairment (Clcr31-80 mL/minute); dosage reduction recommended in moderate renal impairment (Clcr 31-50 mL/minute).
Not studied in severe renal impairment or end-stage renal disease (Clcr ≤30 mL/minute).
Common Adverse Effects
Olaparib monotherapy (≥10%): Nausea, fatigue (including asthenia), anemia, vomiting, diarrhea, decreased appetite, headache, dysgeusia, cough, neutropenia, dyspnea, dizziness, dyspepsia, leukopenia, thrombocytopenia.
Combination therapy with bevacizumab (≥10%): Nausea, fatigue (including asthenia), anemia, lymphopenia, vomiting, diarrhea, neutropenia, leukopenia, urinary tract infection, headache.
Combination therapy with abiraterone and prednisone or prednisolone (≥10%): Anemia, fatigue, nausea, diarrhea, decreased appetite, lymphopenia, dizziness, abdominal pain.
Drug Interactions
Metabolized principally by CYP3A. Substrate and inhibitor of P-glycoprotein (P-gp) in vitro.
Induces CYP2B6 and both inhibits and induces CYP3A in vitro; predicted to be a weak CYP3A inhibitor.
Inhibitor of UGT1A1 in vitro.
Inhibitor of breast cancer resistance protein (BCRP), organic anion transport protein (OATP) 1B1, organic cation transporter (OCT) 1 and OCT2, organic anion transporter (OAT) 3, and multidrug and toxic compound extrusion (MATE) 1 and MATE2K.
Drugs Affecting Hepatic Microsomal Enzymes
Moderate and potent CYP3A inhibitors: Potential increased plasma concentrations and AUC of olaparib. Avoid concomitant use; consider choosing an alternative agent with less CYP3A inhibition potential. If concomitant use of a potent CYP3A inhibitor cannot be avoided, reduce olaparib dosage to 100 mg twice daily. If concomitant use of a moderate CYP3A inhibitor cannot be avoided, reduce olaparib dosage to 150 mg twice daily. If concomitant use of the CYP3A inhibitor is discontinued, return olaparib dosage to the dosage used prior to initiation of the CYP3A inhibitor (after 3–5 terminal half-lives of the CYP3A inhibitor).
CYP3A inducers: Potential pharmacokinetic interaction (decreased plasma concentrations and AUC of olaparib). Avoid concomitant use of moderate or potent CYP3A inducers.
Specific Drugs and Foods
|
Drug or Food |
Interaction |
Comments |
|---|---|---|
|
Efavirenz |
Efavirenz: May decrease peak concentrations and AUC of olaparib by 31 and 60%, respectively |
Avoid concomitant use |
|
Fluconazole |
Increased peak concentrations and AUC of olaparib by 14 and 121%, respectively |
Avoid concomitant use; consider choosing alternative agent with less CYP3A inhibition potential If concomitant use cannot be avoided, reduce olaparib dosage to 150 mg twice daily |
|
Grapefruit |
Known to inhibit CYP3A |
Avoid concomitant use |
|
Itraconazole |
Increased olaparib peak concentrations and AUC by 42 and 170%, respectively |
Avoid concomitant use; consider choosing alternative agent with less CYP3A inhibition potential If concomitant use cannot be avoided, reduce olaparib dosage to 100 mg twice daily |
|
Seville Orange |
Known to inhibit CYP3A |
Avoid concomitant use |
|
Rifampin |
Decreased peak concentrations and AUC of olaparib by 71 and 87%, respectively |
Avoid concomitant use |
Olaparib Pharmacokinetics
Absorption
Bioavailability
Peak plasma concentrations achieved in median of 1.5 hours.
Systemic exposure increases approximately proportionally over dose range of 25–450 mg; peak plasma concentrations increase slightly less than proportionally over same dose range.
Following repeated doses, AUC mean accumulation ratio is 1.8.
Food
Administration with high-fat, high-calorie meal delays Tmax by 2.5 hours but does not substantially affect extent of absorption (mean AUC increased by approximately 8%).
Special Populations
Mild hepatic impairment (Child-Pugh class A): Mean Cmax and AUC increased by 13 and 15%, respectively.
Moderate hepatic impairment (Child-Pugh class B): Mean Cmax decreased by 13% and AUC increased by 8%.
Severe hepatic impairment (Child-Pugh class C): Not studied.
Mild renal impairment (Clcr 51–80 mL/minute): Mean Cmax and AUC increased by 15 and 24%, respectively.
Moderate renal impairment (Clcr 31–50 mL/minute): Mean Cmax and AUC increased by 26 and 44%, respectively.
Severe renal impairment or end-stage renal disease (Clcr ≤30 mL/minute): Not studied.
Distribution
Extent
Not known whether distributed into human milk.
Plasma Protein Binding
Approximately 82%.
Special Populations
Protein binding not affected by mild to moderate hepatic impairment.
Elimination
Metabolism
Primarily metabolized by CYP3A.
Elimination Route
Eliminated in urine (44%) and feces (42%).
Half-life
14.9 hours.
Stability
Storage
Oral
Tablets
20–25°C (excursions permitted between 15–30°C). Store in original container to protect from moisture.
Actions
-
Inhibits mammalian poly(ADP-ribose) polymerase (PARP) enzymes, including PARP-1, PARP-2, and PARP-3. PARP enzymes are involved in normal cellular homeostasis, including DNA transcription and DNA repair. In prostate cancer models, the PARP-1 enzyme helps regulate androgen receptor activity.
-
Olaparib-induced cytotoxicity may involve inhibition of PARP enzymatic activity and increased formation of PARP-DNA complex, which results in DNA damage and cancer cell death.
-
PARP inhibitors, including olaparib, appear to be selective for tumor cells harboring certain homologous recombination deficiencies (e.g., BRCA1 and BRCA2 mutations). In vitro, olaparib inhibited growth of such select tumor cell lines.
-
Reduces tumor growth of xenograft models of human cancer in mice as a single agent or following platinum-based chemotherapy.
-
Increases cytotoxicity and anti-tumor activity in BRCA-deficient cell lines and mouse tumor models deficient in BRCA1/2, ATM, and other genes involved in homologous recombination repair, and correlates with platinum response.
-
In combination with androgen receptor inhibition, leads to cytotoxicity in vitro and anti-tumor activity in mouse xenograft models.
Advice to Patients
-
Importance of providing a copy of written patient information (medication guide) each time olaparib is dispensed. Advise patients to read the patient information before taking olaparib and each time the prescription is refilled.
-
Advise patients to swallow olaparib tablets whole and not to chew, crush, dissolve, or divide tablets. Inform patients to avoid grapefruit, grapefruit juice, Seville oranges, and Seville orange juice while taking the drug.
-
If a dose is missed, advise patients not to take an extra dose and to take the next normal dose at the regularly scheduled time.
-
Inform patients that olaparib tablets should be stored at room temperature (20–25°C) and that exposure to temperatures greater than 30°C should be avoided. Inform patients that olaparib tablets should be stored in the original container to protect from moisture.
-
Inform patients of the risk of myelodysplatic syndrome (MDS) and acute myeloid leukemia (AML). Advise patients to inform their clinician if fatigue/asthenia, fever, weight loss, frequent infections, bruising, unusual bleeding (including hematuria or bloody stool), or shortness of breath occurs.
-
Inform patients of the importance of hematologic monitoring during olaparib therapy.
-
Inform patients of the risk of pneumonitis. Advise patients to inform their clinician if new or worsening respiratory symptoms, including shortness of breath, fever, cough, or wheezing, occur.
-
Advise patients to immediately report any signs or symptoms of venous thromboembolism, including pain or swelling of the extremities, shortness of breath, chest pain, rapid breathing, and fast heart rate.
-
Advise patients that mild or moderate nausea and/or vomiting commonly occurs with olaparib therapy; patients experiencing these symptoms should contact their clinician for advice on available antiemetic treatment options.
-
Advise patients of the risk of fetal harm and pregnancy loss. Inform females of reproductive potential to avoid pregnancy and to use an effective method of contraception while receiving olaparib and for at least 6 months following discontinuance of therapy. Inform males with female partners of reproductive potential or partners who are pregnant to use an effective method of contraception while receiving olaparib and for 3 months following discontinuance of therapy. Inform males not to donate sperm while receiving olaparib and for 3 months following discontinuance of therapy. Advise women to inform their clinician immediately if they become pregnant during therapy or think they may be pregnant. If pregnancy occurs, advise pregnant women of potential risk to the fetus.
-
Advise women to avoid breast-feeding while receiving olaparib therapy and for at least 1 month following discontinuance of therapy.
-
Advise patients to inform their clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements (e.g., St. John's wort), as well as any concomitant illnesses (e.g., respiratory disorders, liver or kidney damage).
-
Inform patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
Olaparib is obtained through designated specialty pharmacies and specialty distributors. Contact manufacturer or consult the manufacturer website for specific availability information.
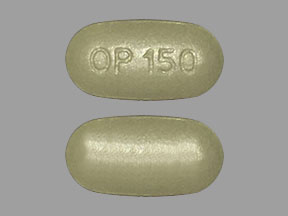
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
100 mg |
Lynparza |
AstraZeneca |
|
150 mg |
Lynparza |
AstraZeneca |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions May 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Frequently asked questions
- How long does it take Lynparza (olaparib) to work?
- How effective is Lynparza (olaparib)?
- Does Lynparza (olaparib) cause hair loss?
More about olaparib
- Check interactions
- Compare alternatives
- Reviews (19)
- Side effects
- Dosage information
- During pregnancy
- Drug class: PARP inhibitors
- Breastfeeding
- En español