niCARdipine Hydrochloride (Monograph)
Brand name: Cardene
Drug class: Dihydropyridines
Introduction
Calcium-channel blocking agent; dihydropyridine derivative.1
Uses for niCARdipine Hydrochloride
Hypertension
Oral management of hypertension (alone or in combination with other classes of antihypertensive agents).1 2 3 1200
Therapy with extended-release capsules generally is preferred because of less frequent dosing, potentially smoother BP control,500 1200 and concerns raised by experience with short-acting (conventional, immediate-release) nifedipine.35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 61 72 73
Calcium-channel blockers are recommended as one of several preferred agents for the initial management of hypertension according to current evidence-based hypertension guidelines; other preferred options include ACE inhibitors, angiotensin II receptor antagonists, and thiazide diuretics.501 502 503 504 1200 While there may be individual differences with respect to recommendations for initial drug selection and use in specific patient populations, current evidence indicates that these antihypertensive drug classes all generally produce comparable effects on overall mortality and cardiovascular, cerebrovascular, and renal outcomes.501 502 503 504 1200 1213
Individualize choice of therapy; consider patient characteristics (e.g., age, ethnicity/race, comorbidities, cardiovascular risk) as well as drug-related factors (e.g., ease of administration, availability, adverse effects, cost).501 502 503 504 515 1200 1201
A 2017 ACC/AHA multidisciplinary hypertension guideline classifies BP in adults into 4 categories: normal, elevated, stage 1 hypertension, and stage 2 hypertension.1200 (See Table 1.)
Source: Whelton PK, Carey RM, Aronow WS et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13-115.
Individuals with SBP and DBP in 2 different categories (e.g., elevated SBP and normal DBP) should be designated as being in the higher BP category (i.e., elevated BP).
|
Category |
SBP (mm Hg) |
DBP (mm Hg) |
|
|---|---|---|---|
|
Normal |
<120 |
and |
<80 |
|
Elevated |
120–129 |
and |
<80 |
|
Hypertension, Stage 1 |
130–139 |
or |
80–89 |
|
Hypertension, Stage 2 |
≥140 |
or |
≥90 |
The goal of hypertension management and prevention is to achieve and maintain optimal control of BP.1200 However, the BP thresholds used to define hypertension, the optimum BP threshold at which to initiate antihypertensive drug therapy, and the ideal target BP values remain controversial.501 503 504 505 506 507 508 515 523 526 530 1200 1201 1207 1209 1222 1223 1229
The 2017 ACC/AHA hypertension guideline generally recommends a target BP goal (i.e., BP to achieve with drug therapy and/or nonpharmacologic intervention) of <130/80 mm Hg in all adults regardless of comorbidities or level of atherosclerotic cardiovascular disease (ASCVD) risk.1200 In addition, an SBP goal of <130 mm Hg is recommended for noninstitutionalized ambulatory patients ≥65 years of age with an average SBP of ≥130 mm Hg.1200 These BP goals are based upon clinical studies demonstrating continuing reduction of cardiovascular risk at progressively lower levels of SBP.1200 1202 1210
Other hypertension guidelines generally based target BP goals on age and comorbidities.501 504 536 Guidelines such as those issued by the JNC 8 expert panel generally have targeted a BP goal of <140/90 mm Hg regardless of cardiovascular risk and have used higher BP thresholds and target BPs in elderly patients501 504 536 compared with those recommended by the 2017 ACC/AHA hypertension guideline.1200
Some clinicians continue to support previous target BPs recommended by JNC 8 due to concerns about the lack of generalizability of data from some clinical trials (e.g., SPRINT study) used to support the 2017 ACC/AHA hypertension guideline and potential harms (e.g., adverse drug effects, costs of therapy) versus benefits of BP lowering in patients at lower risk of cardiovascular disease.1222 1223 1224 1229
Consider potential benefits of hypertension management and drug cost, adverse effects, and risks associated with the use of multiple antihypertensive drugs when deciding a patient's BP treatment goal.1200 1220 1229
For decisions regarding when to initiate drug therapy (BP threshold), the 2017 ACC/AHA hypertension guideline incorporates underlying cardiovascular risk factors.1200 1207 ASCVD risk assessment is recommended by ACC/AHA for all adults with hypertension.1200
ACC/AHA currently recommend initiation of antihypertensive drug therapy in addition to lifestyle/behavioral modifications at an SBP ≥140 mm Hg or DBP ≥90 mm Hg in adults who have no history of cardiovascular disease (i.e., primary prevention) and a low ASCVD risk (10-year risk <10%).1200
For secondary prevention in adults with known cardiovascular disease or for primary prevention in those at higher risk for ASCVD (10-year risk ≥10%), ACC/AHA recommend initiation of antihypertensive drug therapy at an average SBP ≥130 mm Hg or an average DBP ≥80 mm Hg.1200
Adults with hypertension and diabetes mellitus, chronic kidney disease (CKD), or age ≥65 years are assumed to be at high risk for cardiovascular disease; ACC/AHA state that such patients should have antihypertensive drug therapy initiated at a BP ≥130/80 mm Hg.1200 Individualize drug therapy in patients with hypertension and underlying cardiovascular or other risk factors.502 1200
In stage 1 hypertension, experts state that it is reasonable to initiate drug therapy using the stepped-care approach in which one drug is initiated and titrated and other drugs are added sequentially to achieve the target BP.1200 Initiation of antihypertensive therapy with 2 first-line agents from different pharmacologic classes recommended in adults with stage 2 hypertension and average BP >20/10 mm Hg above BP goal.1200
Calcium-channel blockers may be beneficial in hypertensive patients with certain coexisting conditions (e.g., ischemic heart disease)523 and in geriatric patients, including those with isolated systolic hypertension.502 510 1200
Calcium-channel blockers may be particularly useful in black patients with hypertension;100 101 501 504 1250 1251 1252 1253 1254 1255 such patients generally respond better to monotherapy with calcium-channel blockers or thiazide diuretics than to other antihypertensive drug classes (e.g., ACE inhibitors, angiotensin II receptor antagonists).501 504 1200 However, the combination of an ACE inhibitor or an angiotensin II receptor antagonist with a calcium-channel blocker or thiazide diuretic produces similar BP lowering in black patients as in other racial groups.1200
IV, short-term management of hypertension when oral therapy is not feasible or desirable.18
IV management of hypertensive crises (e.g., emergencies) in adults.18 1200
IV, rapid reduction of BP in the management of acute severe hypertension and life-threatening symptoms in children and adolescents† [off-label].1150
Angina
Management of chronic stable angina pectoris (alone or in combination with other antianginal agents).1 3 25
niCARdipine Hydrochloride Dosage and Administration
General
BP Monitoring and Treatment Goals
-
Monitor BP regularly (i.e., monthly) during therapy and adjust dosage of the antihypertensive drug until BP controlled.1200
-
If unacceptable adverse effects occur, discontinue drug and initiate another antihypertensive agent from a different pharmacologic class.1200 1216
-
If adequate BP response not achieved with a single antihypertensive agent, either increase dosage of single drug or add a second drug with demonstrated benefit and preferably a complementary mechanism of action (e.g., ACE inhibitor, angiotensin II receptor antagonist, thiazide diuretic).1200 1216 Many patients will require ≥2 drugs from different pharmacologic classes to achieve BP goal; if goal BP still not achieved with 2 antihypertensive agents, add a third drug.1200 1216 1220
Severe Hypertension and Hypertensive Emergency
-
Adults with a compelling indication—severe preeclampsia or eclampsia or pheochromocytoma crisis: Reduce SBP to <140 mm Hg during the first hour.1200
-
Adults with a compelling indication—acute aortic dissection: Reduce SBP to <120 mm Hg within the first 20 minutes.1200
-
Initial goal of IV therapy in adults with a hypertensive emergency without a compelling indication is to reduce SBP by ≤25% within the first hour, followed by further BP reduction if stable to 160/110 or 160/100 mm Hg within the next 2–6 hours, avoiding excessive declines in BP that could precipitate renal, cerebral, or coronary ischemia.1200 If this BP is well tolerated and the patient is clinically stable, may implement further gradual reductions toward normal BP in the next 24–48 hours.1200
-
Children and adolescents: Reduce BP by ≤25% of the planned reduction over the first 8 hours.1150
Administration
Administer orally1 2 5 or by IV infusion.18 22 23
Oral Administration
Conventional Capsules
Administer orally 3 times daily.1
Extended-release Capsules
Administer orally twice daily.2
IV Administration
Administer by slow, continuous IV infusion.18 22 23
Some experts state drug may be administered by direct IV (“bolus”) injection in children and adolescents with acute severe hypertension and life-threatening symptoms.1150
Must dilute commercially available injection concentrate containing 2.5 mg/mL with a compatible IV infusion solution prior to administration.18
Alternatively, administer as premixed solution (0.1 mg/mL in either 4.8% dextrose or 0.86% sodium chloride injection, 0.2 mg/mL in either 5% dextrose or 0.83% sodium chloride injection).600 601
If administered via a peripheral vein, change infusion site every 12 hours to minimize risk of venous irritation.18
Monitor BP closely during and after completion of IV administration; avoid rapid or excessive reduction in systolic or diastolic BP.18
Dilution
Injection concentrate: Dilute each 25-mg ampul containing 2.5 mg/mL with 240 mL of a compatible IV solution to provide a solution containing 0.1 mg/mL.18 c
Standardize 4 Safety
Standardized concentrations for nicardipine have been established through Standardize 4 Safety (S4S), a national patient safety initiative to reduce medication errors, especially during transitions of care.249 250 Multidisciplinary expert panels were convened to determine recommended standard concentrations.249 250 Because recommendations from the S4S panels may differ from the manufacturer’s prescribing information, caution is advised when using concentrations that differ from labeling, particularly when using rate information from the label.249 250 For additional information on S4S (including updates that may be available), see [Web].249 250
dosing units differ from concentration units
|
Patient Population |
Concentration Standards |
Dosing Units |
|---|---|---|
|
Adults |
0.1 mg/mL |
mg/hour |
|
0.2 mg/mL |
||
|
Pediatric patients (<50 kg) |
0.1 mg/mL |
mcg/kg/min |
|
0.2 mg/mL |
||
|
0.5 mg/mL |
Dosage
Available as nicardipine hydrochloride; dosage is expressed in terms of the salt.a b c
Pediatric Patients
Acute Severe Hypertension† [off-label]
Rapid Reduction of BP† [off-label]
IVDirect IV (“bolus”) injection: 30 mcg/kg (up to 2 mg) per dose.1150
IV infusion: 0.5–4 mcg/kg per minute.1150
Adults
Hypertension
Conventional Capsules
OralInitially, 20 mg 3 times daily.1 5
Adjust dosage according to patient’s peak (approximately 1–2 hours after dosing, particularly during initiation of therapy) and trough (8 hours after dosing) BP responses, but generally no more frequently than at 3-day intervals.1
Usual dosage is 20–40 mg 3 times daily.1
Extended-Release Capsules
OralInitially, 30 mg twice daily.2
Adjust dosage according to BP response 2–4 hours after dosing as well as just prior to next dose.2
Usual dosage range is 30–60 mg twice daily.2 1200
Switching to Extended-Release Capsules
OralTotal daily dose of conventional tablets not a useful guide to judging effective dose of extended-release capsules.2 c However, may administer the currently effective total daily dose of conventional capsules and adjust dosage according to BP response.2 c
Short-term Management with IV Therapy
IVInitially, 5 mg/hour.18
If target BP is not achieved, increase rate by 2.5 mg/hour every 15 minutes, up to 15 mg/hour.18
For more rapid reduction, initially, 5 mg/hour. If the target BP is not achieved, increase rate by 2.5 mg/hour every 5 minutes, up to 15 mg/hour.18
Following achievement of desired BP response, decrease rate to 3 mg/hour;18 adjust rate as necessary to maintain desired BP response.18
Conversion From Oral to IV Therapy
IV|
Oral Dosage (as Conventional Capsules) |
Equivalent IV Infusion Rates |
|---|---|
|
20 mg every 8 hours |
0.5 mg/hour |
|
30 mg every 8 hours |
1.2 mg/hour |
|
40 mg every 8 hours |
2.2 mg/hour |
Hypertensive Emergency
IV5–15 mg/hour; adjust according to BP response and tolerance.1200
Angina
Conventional Capsules
OralInitially, 20 mg 3 times daily.1 5 Adjust dosage according to patient tolerance and response at ≥3-day intervals.1
Usual dosage range is 20–40 mg 3 times daily.1
Prescribing Limits
Adults
Hypertension
IV
15 mg/hour.18
Special Populations
Hepatic Impairment
Conventional capsules: Initially, 20 mg twice daily in patients with severe hepatic impairment.1 Individualize dosage, but maintain a twice-daily dosing schedule.1
IV infusion: Consider dosage reduction.18 Use with caution in patients with portal hypertension.18
Renal Impairment
Conventional capsules: Initially, 20 mg 3 times daily.1 5 Titrate dosage carefully.1
Extended-release capsules: Initially, 30 mg twice daily.2 Titrate dosage carefully.2
IV infusion: Titrate dosage carefully.18
Geriatric Patients
Cautious dosing recommended.a b For conventional and extended-release capsules, initiate therapy at low end of dosage range.20 68
Cautions for niCARdipine Hydrochloride
Contraindications
-
Known hypersensitivity to nicardipine or any ingredient in the formulation.1 2 18
-
Advanced aortic stenosis, since reduction in diastolic pressure may worsen myocardial oxygen balance.1 2 18
Warnings/Precautions
Warnings
Increased Angina
Increased frequency, duration, and severity of angina upon initiation or dosage increase of calcium channel blockers.1 2 18
Heart Failure
Use with caution in patients with heart failure or substantial left ventricular dysfunction, especially in those receiving concomitant β-adrenergic blocking agents.1 2 18
β-Blocker Withdrawal
Taper dosage of β-adrenergic blocking agent, preferably over 8–10 days before initiation of nicardipine.1 2 18 Nicardipine is not a β-adrenergic blocking agent and offers no protection against abrupt withdrawal of these agents.1 2 18
General Precautions
Hypotension
Possible symptomatic hypotension from decreased peripheral resistance.1 2 18 Use with caution in patients with acute cerebral infarction or hemorrhage; avoid systemic hypotension in these patients.1 2 18
Monitor BP carefully, especially during initiation of therapy or upward adjustment of dosage.1
Pheochromocytoma
Limited clinical experience in patients with hypertension associated with pheochromocytoma.18 Use with caution.18
Specific Populations
Pregnancy
Lactation
Distributed into milk in high concentrations in rats.1 2 18 Use not recommended.1 2 18
Pediatric Use
Safety and efficacy not established in children <18 years of age.1 2 18
Some experts recommend use in children and adolescents† [off-label] for acute severe hypertension with life-threatening symptoms.1150
Use with caution for rapid reduction of BP in children and adolescents† [off-label] ; may cause reflex tachycardia.1150
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether geriatric patients respond differently than younger adults.a b Select dosage with caution; initiate dosage at lower end of recommended range.a b
Hepatic Impairment
Use with caution in patients with hepatic impairment or reduced hepatic blood flow; dosage adjustments recommended.1 2 18 24 (See Hepatic Impairment under Dosage and Administration.)
Use of extended-release capsules has not been studied in patients with severe hepatic impairment.2
Renal Impairment
Use with caution; careful dosage titration recommended.1 2 18 (See Renal Impairment under Dosage and Administration.)
Common Adverse Effects
With oral therapy, pedal edema, dizziness, headache, asthenia, flushing, increased angina, vasodilation, palpitation.a b
With IV therapy, headache, hypotension, nausea/vomiting, tachycardia.c
Drug Interactions
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Antacids (magnesium hydroxide) |
||
|
β-Adrenergic blockers (e.g., propranolol) |
Pharmacokinetic interaction (e.g., effect on plasma protein binding of nicardipine) unlikely1 2 18 |
|
|
Cimetidine |
||
|
Cyclosporine |
Monitor plasma cyclosporine concentrations closely and adjust dosage accordingly1 2 18 |
|
|
Digoxin |
||
|
Dipyridamole |
||
|
Fentanyl |
Potential for severe hypotension with concomitant use of a β-adrenergic blocker and a calcium channel blocker1 2 18 |
Increase circulating fluid volume if hypotension occurs1 2 18 |
|
Furosemide |
||
|
Naproxen |
||
|
Quinidine |
||
|
Warfarin |
niCARdipine Hydrochloride Pharmacokinetics
Absorption
Bioavailability
Completely absorbed from the GI tract following oral administration; peak plasma concentrations of conventional and extended-release capsules are attained within 0.5–2 and 1–4 hours, respectively.1 2
Minimum plasma levels of equivalent doses of conventional and extended-release capsules are similar.2
Bioavailability of conventional capsules is about 35%;1 2 extended-release capsules have a slightly lower bioavailability, except at the highest doses.2
Food
High-fat meal decreases bioavailability of conventional and extended-release capsules.1 2
Special Populations
In patients with severe hepatic impairment, peak plasma concentrations and AUC increased by 1.8 and 4-fold, respectively, and terminal half-life prolonged to 19 hours.1 2
In patients with moderate renal impairment, peak plasma concentrations and AUC increased by 2- to 3-fold following administration of conventional or extended-release capsules.1 2
Distribution
Extent
Distributed into milk in rats.1 2
Plasma Protein Binding
Elimination
Metabolism
Extensively metabolized in the liver.1 2 18
Elimination Route
Excreted in urine (49–60%) and feces (35–43%).1 2 18
Half-life
Multi-phasic; terminal elimination half-life is 8.6 and 14.4 hours following oral and IV administration, respectively.1 2 18
Stability
Storage
Oral
Conventional Capsules and Extended-release Capsules
Light resistant containers at 15–30°C.a b
Parenteral
Injection Concentrate
20–25°C; protect from light.c Avoid exposure to increased temperatures.c
Premixed Injection for Infusion
20–25°C; protect from light, freezing, and excessive heat.600 601
Actions
-
Inhibits transmembrane influx of extracellular calcium ions across the membranes of myocardial cells and vascular smooth muscle cells, without changing serum calcium concentrations.a b c
-
Peripheral arterial vasodilator; acts directly on vascular smooth muscle causing reduction in peripheral vascular resistance (afterload) and BP.a b c
Advice to Patients
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.1 2 18
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.1 2 18
-
Importance of informing patients of other important precautionary information.1 2 18 (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
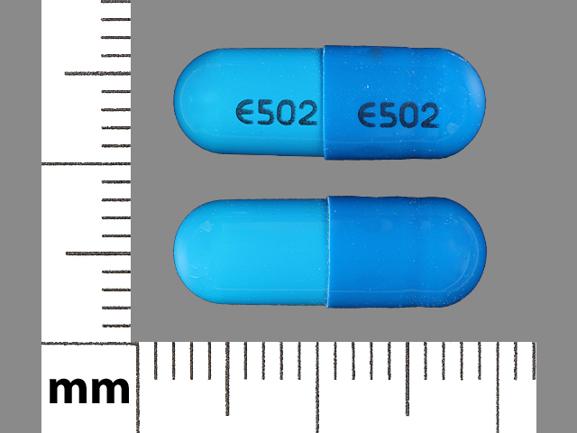
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules |
20 mg* |
Nicardipine Hydrochloride Capsules |
|
|
30 mg* |
Nicardipine Hydrochloride Capsules |
|||
|
Capsules, extended-release |
30 mg |
Cardene SR |
Chiesi |
|
|
60 mg |
Cardene SR |
Chiesi |
||
|
Parenteral |
For injection, concentrate, for IV infusion |
2.5 mg/mL* |
Cardene I.V. |
Chiesi |
|
Nicardipine Hydrochloride Injection |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Injection, for IV infusion |
0.1 mg/mL (20 mg) in 4.8% Dextrose |
Cardene I.V. |
Chiesi |
|
0.2 mg/mL (40 mg) in 5% Dextrose |
Cardene I.V. |
Chiesi |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Injection, for IV infusion |
0.1 mg/mL (20 mg) in 0.86% Sodium Chloride |
Cardene I.V. |
Chiesi |
|
0.2 mg/mL (40 mg) in 0.83% Sodium Chloride |
Cardene I.V. |
Chiesi |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
1. Syntex Laboratories, Inc. Cardene (nicardipine hydrochloride) capsules prescribing information. Palo Alto CA; 1992 Jul.
2. Syntex Laboratories, Inc. Cardene SR (nicardipine hydrochloride) sustained release capsules prescribing information. Palo Alto CA; 1992 Jan.
3. Freedman DD, Waters DD. Second generation dihydropyridine calcium antagonists. Greater vascular selectivity and some unique applications. Drugs. 1987; 34:578-98. https://pubmed.ncbi.nlm.nih.gov/3319491
4. Murdoch D, Heel RC. Amlodipine : a review of its pharmacodynamic and pharmacokinetic properties and therapeutic use in cardiovascular disease. Drugs. 1991; 41:478-505. https://pubmed.ncbi.nlm.nih.gov/1711448
5. Sorkin EM, Clissold SP. Nicardipine. A review of its pharmacodynamic and pharmacokinetic properties, and therapeutic efficacy, in the treatment of angina pectoris, hypertension and related cardiovascular disorders. Drugs. 1987; 33:296-345. https://pubmed.ncbi.nlm.nih.gov/3297616
8. Syntex Laboratories, Inc, Palo Alto, CA: (personal observations).
9. Sandoz Pharmaceuticals Corp. DynaCirc (isradipine) capsules prescribing information. East Hanover, NJ; 1992 Jun.
10. Lopez LM, Santiago TM. Isradipine—another calcium-channel blocker for the treatment of hypertension and angina. Ann Pharmacother. 1992; 26:789-99. https://pubmed.ncbi.nlm.nih.gov/1535246
11. Fitton A, Benfield P. Isradipine: a review of its pharmacodynamic and pharmacokinetic properties, and therapeutic use in cardiovascular disease. Drugs. 1990; 40:31-74. https://pubmed.ncbi.nlm.nih.gov/2143980
12. Walton T, Symes LR. Felodipine and isradipine: new calcium-channel blocking agents for the treatment of hypertension. Clin Pharm. 1993; 12:261-75. https://pubmed.ncbi.nlm.nih.gov/8458178
14. Prisant LM, Carr AA, Nelson EB et al. Isradipine vs propranolol in hydrochlorothiazide-treated hypertensives: a multicenter evaluation. Arch Intern Med. 1989; 149:2453-7. https://pubmed.ncbi.nlm.nih.gov/2530945
15. Anon. Isradipine for hypertension. Med Lett Drugs Ther. 1991; 33:51-4. https://pubmed.ncbi.nlm.nih.gov/1827655
16. Alderman MH. Which antihypertensive drugs first—and why! JAMA. 1992; 267:2786-7. Editorial.
17. Weber MA, Laragh JH. Hypertension: steps forward and steps backward: the Joint National Committee fifth report. Arch Intern Med. 1993; 153:149-52. https://pubmed.ncbi.nlm.nih.gov/8422205
18. PDL Biopharma. Cardene I.V. (nicardipine hydrochloride) prescribing information. Philadelphia PA; 2006 Jan.
19. Fagan TC, Tyler ED, Reitman MA et al. Sustained-release nicardipine in mild-to-moderate hypertension. Chest. 1993; 104:427-33. https://pubmed.ncbi.nlm.nih.gov/8339631
20. Frampton JE, Faulds D. Nicardipine. A review of its pharmacology and therapeutic efficacy in older patients. Drugs Aging. 1993; 3:165-87. https://pubmed.ncbi.nlm.nih.gov/8477149
21. Bosch X, Sobrino J, Lopez-Soto A et al. Parotitis due to nicardipine. BMJ. 1992; 304:882. https://pubmed.ncbi.nlm.nih.gov/1392752
22. IV Nicardipine Study Group. Efficacy and safety of intravenous nicardipine in the control of postoperative hypertension. Chest. 1991; 99:393-8. https://pubmed.ncbi.nlm.nih.gov/1989801
23. Wallin JD, Fletcher E, Ram VS et al. Intravenous nicardipine for the treatment of severe hypertension. A double-blind, placebo-controlled multicenter trial. Arch Intern Med. 1989; 149:2662-9. https://pubmed.ncbi.nlm.nih.gov/2688586
24. Razak TA, McNeil JJ, Sewel RB et al. The effect of hepatic cirrhosis on the pharmacokinetics and blood pressure response to nicardipine. Clin Pharmacol Ther. 1990; 47:463-9. https://pubmed.ncbi.nlm.nih.gov/2328554
25. Sklar J, Dennish GW III, Glode J et al. Usefulness of nicardipine as monotherapy for chronic, stable angina. Am J Cardiol. 1989; 63:1203-7. https://pubmed.ncbi.nlm.nih.gov/2711990
26. Eicher JC, Chalopin JM, Tanter Y et al. Nicardipine and urinary retention. JAMA. 1987; 258:3388. https://pubmed.ncbi.nlm.nih.gov/3682133
27. Dubois C, Blanchard D. Efficacy and safety of nicardipine in 29,104 patients with hypertension. Clin Ther. 1989; 11:452-60. https://pubmed.ncbi.nlm.nih.gov/2673515
28. Nami R, Caruso D, Dormi A et al. Efficacy and tolerability of nicardipine slow release and enalapril in elderly hypertensive patients: results of a multicenter study. Curr Ther Res. 1993; 54:221-31.
29. Kubota K, Pearce GL, Inman WHW. Vasodilation-related adverse events in diltiazem and dihydropyridine calcium antagonists studied by prescription-event monitoring. Eur J Clin Pharmacol. 1995; 48:1-7. https://pubmed.ncbi.nlm.nih.gov/7621840
30. Jannet D, Carbonne B, Sebban E et al. Nicardipine versus metoprolol in the treatment of hypertension during pregnancy: a randomized comparative trial. Obstet Gynecol. 1994; 84:354-9. https://pubmed.ncbi.nlm.nih.gov/8058230
31. Carbonne B, Jannet D, Touboul C et al. Nicardipine treatment of hypertension during pregnancy. Obstet Gynecol. 1993; 81:908-14. https://pubmed.ncbi.nlm.nih.gov/8497354
32. Narváez M, Figueras A, Capellá D et al. Tinnitus with calcium-channel blockers. Lancet. 1994; 343:1229-30.
33. Agre K. An overview of the safety and efficacy of nicardipine in clinical trials. Am J Cardiol. 1987; 59:31J-5J. https://pubmed.ncbi.nlm.nih.gov/3300239
34. Ahmad S. Nicardipine-induced hyperglycemia. Am Fam Physician. 1992; 45:449,452. https://pubmed.ncbi.nlm.nih.gov/1739035
35. Glasser SP, Clark PI, Lipicky RJ et al. Exposing patients with chronic, stable, exertional angina to placebo periods in drug trials. JAMA. 1991; 265:1550- 4. https://pubmed.ncbi.nlm.nih.gov/1671885
36. National Heart, Lung, and Blood Institute. NHLBI panel reviews safety of calcium channel blockers. Rockville, MD; 1995 Aug 31. Press release.
37. National Heart, Lung, and Blood Institute. New analysis regarding the safety of calcium-channel blockers: a statement for health professionals from the National Heart, Lung, and Blood Institute. Rockville, MD; 1995 Sep 1.
38. Anon. NHLBI panel stands by JNC V in response to Circulation CCB article; AIM report supports use of beta blockers for prevention of sudden cardiac death. F-D-C Rep. 1995; 57(Sep 4):3-4.
39. American Heart Association. Public advisory statement on calcium channel blocker drugs. Dallas, TX; 1995 Aug 28.
40. Psaty BM, Heckbert SR, Koepsell TD et al. The risk of myocardial infarction associated with antihypertensive drug therapies. JAMA. 1995; 274:620-5. https://pubmed.ncbi.nlm.nih.gov/7637142
41. Psaty BM, Heckbert SR, Koepsell TD et al. The risk of incident myocardial infarction associated with anti- hypertensive drug therapies. Circulation. 1995; 91:925.
42. Buring JE, Glynn RJ, Hennekens CH. Calcium channel blockers and myocardial infarction: a hypothesis formulated but not yet tested. JAMA. 1995; 274:654-5. https://pubmed.ncbi.nlm.nih.gov/7637148
43. Furberg CD, Psaty BM, Meyer JV. Nifedipine: dose-related increase in mortality in patients with coronary heart disease. Circulation. 1995; 92:1326-31. https://pubmed.ncbi.nlm.nih.gov/7648682
44. Opie LH, Messerli FH. Nifedipine and mortality: grave defects in the dossier. Circulation. 1995; 92:1068-73. https://pubmed.ncbi.nlm.nih.gov/7648646
45. Kloner RA. Nifedipine in ischemic heart disease. Circulation. 1995; 92:1074-8. https://pubmed.ncbi.nlm.nih.gov/7648647
46. Yusuf S. Calcium antagonists in coronary artery disease and hypertension: time for reevaluation? Circulation. 1995; 92:1079-82. Editorial.
47. Lenfant C. The calcium channel blocker scare: lessons for the future. Circulation. 1995; 91:2855-6. https://pubmed.ncbi.nlm.nih.gov/7796490
48. Habib GB. Are calcium antagonists harmful in hypertensive patients? Distinguishing hype from reality. Chest. 1995; 108:3-5. https://pubmed.ncbi.nlm.nih.gov/7606987
49. Horton R. Spinning the risks and benefits of calcium antagonists. Lancet. 1995; 346:586-7. https://pubmed.ncbi.nlm.nih.gov/7650997
50. Yusuf S, Held P, Furberg C. Update of effects of calcium antagonists in myocardial infarction or angina in light of the Second Danish Verapamil Infarction Trial (DAVIT-II) and other recent studies. Am J Cardiol. 1991; 67:1295-7. https://pubmed.ncbi.nlm.nih.gov/2035457
51. Egstrup K, Andersen PE Jr. Transient myocardial ischemia during nifedipine therapy in stable angina pectoris, and its relation to coronary collateral flow and comparison with metoprolol. Am J Cardiol. 1993; 71:177-83. https://pubmed.ncbi.nlm.nih.gov/8421980
52. Wagenknecht LE, Furberg CD, Hammon JW et al. Surgical bleeding: unexpected effect of a calcium antagonist. BMJ. 1995; 310:776-7. https://pubmed.ncbi.nlm.nih.gov/7711582
53. Miles Inc. American Heart Association, Dr. Psalty and Miles Inc. release statements qualifying possible risks of calcium channel blockers. West Haven, CT; 1995 Mar 15. Press release.
54. Dear healthcare professional letter regarding calcium-channel blockers and increased risk of heart attack. Chicago:Searle. 1995 Mar 17.
55. McClellan K. Unexpected results from MIDAS in atherosclerosis. Inpharma Wkly. 1994; Apr 9:4.
56. Anon. Groups act to dispel concerns about calcium-channel blockers. Am J Health- Syst Pharm. 1995; 52:1154,1158. https://pubmed.ncbi.nlm.nih.gov/7656105
57. Waters D. Proischemic complications of dihydropyridine calcium channel blockers. Circulation. 1991; 84:2598-600. https://pubmed.ncbi.nlm.nih.gov/1959210
58. Messerli FH. Case-control study, meta-analysis, and bouillabaisse: putting the calcium antagonist scare into context. Ann Intern Med. 1995; 123:888-9. https://pubmed.ncbi.nlm.nih.gov/7486476
59. Reviewers’ comments (personal observations).
60. Pratt Pharmacueticals. Procardia (nifedipine) capsules prescribing information (dated 1993 Feb). In: Physicians’ desk reference. 49th ed. Montvale, NJ: Medical Economics Company Inc; 1995:1906-7.
61. Held PH, Yusuf S, Furberg CD. Calcium channel blockers in acute myocardial infarction and unstable angina: an overview. BMJ. 1989; 299:1187-92. https://pubmed.ncbi.nlm.nih.gov/2513047
62. Kitler ME. The changing face of hypertension and antihypertensive agents. Drugs Aging. 1996; 8:5-11. https://pubmed.ncbi.nlm.nih.gov/8785469
63. Parker BM, Cusack BJ, Vestal RE. Pharmacokinetic optimisation of drug therapy in elderly patients. Drugs Aging. 1995; 7:10-8. https://pubmed.ncbi.nlm.nih.gov/7579777
64. Kvasnicka J, Flack JM, Grimm RH. Treatment of hypertension in the presence of coexisting medical conditions. Drugs Aging. 1994; 4:304-12. https://pubmed.ncbi.nlm.nih.gov/8019053
65. Kelly JG, O’Malley K. Calcium antagonists in the elderly. Drugs Aging. 1993; 3:400-7. https://pubmed.ncbi.nlm.nih.gov/8241605
66. Burris JF. Practical considerations in treating the elderly hypertensive patient. Am J Med. 1991; 90(Suppl 4B):28-31S.
67. O’Malley K, Cox JP, O’Brien E. Choice of drug treatment for elderly hypertensive patients. Am J Med. 1991; 90(Suppl 3A):27-33S.
68. Food and Drug Administration. Specific requirements on content and format of labeling for human prescrption drugs; proposed addition of ”geriatric use“ subsection in the labeling; proposed rule (Docket No. 89N-0474). Fed Regist. 1990; 55:46134-7.
69. Bailey DG, Arnold JMO, Spence JD. Grapefruit juice and drugs: how significant in the interaction? Clin Pharmcokinet. 1994; 26:91-8.
71. Kaplan NM. Choice of initial therapy for hypertension. JAMA. 1996; 275:1577-80. https://pubmed.ncbi.nlm.nih.gov/8622249
72. Psaty BM, Smith NL, Siscovich DS et al. Health outcomes associated with antihypertensive therapies used as first-line agents: a systematic review and meta-analysis. JAMA. 1997; 277:739-45. https://pubmed.ncbi.nlm.nih.gov/9042847
73. American College of Cardiology and American Heart Association. ACC/AHA guidelines for the management of patients with acute myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction). J Am Coll Cardiol. 1996; 28:1328-428. https://pubmed.ncbi.nlm.nih.gov/8890834
75. Velussi M, Brocco E, Frigato F et al. Effects of cilazapril and amlodipine on kidney function in hypertensive NIDDM patients. Diabetes. 1996; 45:216-22. https://pubmed.ncbi.nlm.nih.gov/8549868
76. Estacio RO, Jeffers BW, Hiatt WR et al. The effect of nisoldipine as compared with enalapril on cardiovascular outcomes in patients with non-insulin-dependent diabetes and hypertension. N Engl J Med. 1998; 338:645-52. https://pubmed.ncbi.nlm.nih.gov/9486993
77. Pahor M, Psaty BM, Furberg CD. Treatment of hypertensive patients with diabetes. Lancet. 1998; 351:689-90. https://pubmed.ncbi.nlm.nih.gov/9504510
78. Tatti P, Pahor M, Byington RP et al. Outcome results of the Fosinopril versus Amlodipine Cardiovascular Events randomized Trial (FACET) in patients
79. Byington RP, Craven TE, Furberg CD et al. Isradipine, raised glycosylated haemoglobin, and risk of cardiovascular events. Lancet. 1997; 350:1075-6. https://pubmed.ncbi.nlm.nih.gov/10213554
80. Alderman M, Madhavan S, Cohen H. Calcium antagonists and cardiovascular events in patients with hypertension and diabetes. Lancet. 1998; 351:216-7. https://pubmed.ncbi.nlm.nih.gov/9449897
81. Josefson D. Infarction risk found with calcium channel blocker. BMJ. 1998; 316:797.
82. Cutler JA. Calcium-channel blockers for hypertension—uncertainty continues. N Engl J Med. 1998; 338:679-81. https://pubmed.ncbi.nlm.nih.gov/9486999
83. Bayer, West Haven, CT: Personal communication.
84. Bakris GL, Copley JB, Vicknair N et al. Calcium channel blockers versus other antihypertensive therapies on progression of NIDDM associated nephropathy. Kidney Int. 1996; 50:1641-50. https://pubmed.ncbi.nlm.nih.gov/8914031
85. Ameer B, Weintraub RA. Drug interactions with grapefruit juice. Clin Phramacokinet. 1997; 33:103-21.
86. Roller L. Drugs and grapefruit juice. Clin Pharmacol Ther. 1998; 63:87. https://pubmed.ncbi.nlm.nih.gov/9465845
87. Spence JD. Drugs and grapefruit juice. Clin Pharmacol Ther. 1998; 63:87-8. https://pubmed.ncbi.nlm.nih.gov/9465845
88. Izzo JL, Levy D, Black HR. Importance of systolic blood pressure in older Americans. Hypertension. 2000; 35:1021-4. https://pubmed.ncbi.nlm.nih.gov/10818056
89. Frohlich ED. Recognition of systolic hypertension for hypertension. Hypertension. 2000; 35:1019-20. https://pubmed.ncbi.nlm.nih.gov/10818055
90. Bakris GL, Williams M, Dworkin L et al. Preserving renal function in adults with hypertension and diabetes: a consensus approach. Am J Kidney Dis. 2000; 36:646-61. https://pubmed.ncbi.nlm.nih.gov/10977801
91. Associated Press (American Diabetes Association). Diabetics urged: drop blood pressure. Chicago, IL; 2000 Aug 29. Press Release from web site. http://www.diabetes.org/newsroom/
92. Appel LJ. The verdict from ALLHAT—thiazide diuretics are the preferred initial therapy for hypertension. JAMA. 2002; 288:3039-60. https://pubmed.ncbi.nlm.nih.gov/12479770
93. The ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high-riskhypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA. 2002; 288:2981-97. https://pubmed.ncbi.nlm.nih.gov/12479763
96. Kaplan NM. The meaning of ALLHAT. J Hypertens. 2003; 21:233-4. https://pubmed.ncbi.nlm.nih.gov/12569243
100. Wright JT, Dunn JK, Cutler JA et al. Outcomes in hypertensive black and nonblack patients treated with chlorthalidone, amlodipine, and lisinopril. JAMA. 2005; 293:1595-607. https://pubmed.ncbi.nlm.nih.gov/15811979
101. Neaton JD, Kuller LH. Diuretics are color blind. JAMA. 2005; 293:1663-6. https://pubmed.ncbi.nlm.nih.gov/15811986
102. Leenen FHH, Nwachuku CE, Black HR et al. Clinical events in high-risk hypertensive patients randomly assigned to calcium-channel blocker versus angiotensin-converting enzyme inhibitor in the Antihypertensive and Lipid-Lowering treatment to prevent Heart Attack Trial. Hypertension. 2006; 48:374-84. https://pubmed.ncbi.nlm.nih.gov/16864749
103. Messerli FH, Staessen JA. Amlodipine better than lisinopril: how one randomized clinical trial ended fallacies from observational studies? Hypertension. 2006; 48:359-61. Editorial.
249. ASHP. Standardize 4 Safety: pediatric continuous infusion standard. Updated 2024 Mar. From ASHP website. Updates may be available at ASHP website. https://www.ashp.org/standardize4safety
250. ASHP. Standardize 4 Safety: adult continuous infusion standard. Updated 2024 Mar. From ASHP website. Updates may be available at ASHP website. https://www.ashp.org/standardize4safety
500. National Heart, Lung, and Blood Institute National High Blood Pressure Education Program. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7). Bethesda, MD: National Institutes of Health; 2004 Aug. (NIH publication No. 04-5230.)
501. James PA, Oparil S, Carter BL et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014; 311:507-20. https://pubmed.ncbi.nlm.nih.gov/24352797
502. Mancia G, Fagard R, Narkiewicz K et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013; 31:1281-357. https://pubmed.ncbi.nlm.nih.gov/23817082
503. Go AS, Bauman MA, Coleman King SM et al. An effective approach to high blood pressure control: a science advisory from the American Heart Association, the American College of Cardiology, and the Centers for Disease Control and Prevention. Hypertension. 2014; 63:878-85. https://pubmed.ncbi.nlm.nih.gov/24243703
504. Weber MA, Schiffrin EL, White WB et al. Clinical practice guidelines for the management of hypertension in the community: a statement by the American Society of Hypertension and the International Society of Hypertension. J Clin Hypertens (Greenwich). 2014; 16:14-26. https://pubmed.ncbi.nlm.nih.gov/24341872
505. Wright JT, Fine LJ, Lackland DT et al. Evidence supporting a systolic blood pressure goal of less than 150 mm Hg in patients aged 60 years or older: the minority view. Ann Intern Med. 2014; 160:499-503. https://pubmed.ncbi.nlm.nih.gov/24424788
506. Mitka M. Groups spar over new hypertension guidelines. JAMA. 2014; 311:663-4. https://pubmed.ncbi.nlm.nih.gov/24549531
507. Peterson ED, Gaziano JM, Greenland P. Recommendations for treating hypertension: what are the right goals and purposes?. JAMA. 2014; 311:474-6. https://pubmed.ncbi.nlm.nih.gov/24352710
508. Bauchner H, Fontanarosa PB, Golub RM. Updated guidelines for management of high blood pressure: recommendations, review, and responsibility. JAMA. 2014; 311:477-8. https://pubmed.ncbi.nlm.nih.gov/24352759
510. Staessen JA, Fagard R, Thijs L et al. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. The Systolic Hypertension in Europe (Syst-Eur) Trial Investigators. Lancet. 1997; 350:757-64. https://pubmed.ncbi.nlm.nih.gov/9297994
511. JATOS Study Group. Principal results of the Japanese trial to assess optimal systolic blood pressure in elderly hypertensive patients (JATOS). Hypertens Res. 2008; 31:2115-27. https://pubmed.ncbi.nlm.nih.gov/19139601
515. Thomas G, Shishehbor M, Brill D et al. New hypertension guidelines: one size fits most?. Cleve Clin J Med. 2014; 81:178-88. https://pubmed.ncbi.nlm.nih.gov/24591473
516. Wright JT, Bakris G, Greene T et al. Effect of blood pressure lowering and antihypertensive drug class on progression of hypertensive kidney disease: results from the AASK trial. JAMA. 2002; 288:2421-31. https://pubmed.ncbi.nlm.nih.gov/12435255
522. Patel A, ADVANCE Collaborative Group, MacMahon S et al. Effects of a fixed combination of perindopril and indapamide on macrovascular and microvascular outcomes in patients with type 2 diabetes mellitus (the ADVANCE trial): a randomised controlled trial. Lancet. 2007; 370:829-40. https://pubmed.ncbi.nlm.nih.gov/17765963
523. Fihn SD, Gardin JM, Abrams J et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation. 2012; 126:e354-471.
524. WRITING COMMITTEE MEMBERS, Yancy CW, Jessup M et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013; 128:e240-327.
525. Smith SC, Benjamin EJ, Bonow RO et al. AHA/ACCF Secondary Prevention and Risk Reduction Therapy for Patients with Coronary and other Atherosclerotic Vascular Disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. Circulation. 2011; 124:2458-73. https://pubmed.ncbi.nlm.nih.gov/22052934
526. Kernan WN, Ovbiagele B, Black HR et al. Guidelines for the Prevention of Stroke in Patients With Stroke and Transient Ischemic Attack: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2014; :. https://pubmed.ncbi.nlm.nih.gov/24788967
527. O'Gara PT, Kushner FG, Ascheim DD et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013; 127:e362-425.
530. Myers MG, Tobe SW. A Canadian perspective on the Eighth Joint National Committee (JNC 8) hypertension guidelines. J Clin Hypertens (Greenwich). 2014; 16:246-8. https://pubmed.ncbi.nlm.nih.gov/24641124
535. Taler SJ, Agarwal R, Bakris GL et al. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for management of blood pressure in CKD. Am J Kidney Dis. 2013; 62:201-13. https://pubmed.ncbi.nlm.nih.gov/23684145
536. Kidney Disease: Improving Global Outcomes (KDIGO) Blood Pressure Work Group. KDIGO clinical practice guideline for the management of blood pressure in chronic kidney disease. Kidney Int Suppl. 2012: 2: 337-414.
541. Perk J, De Backer G, Gohlke H et al. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts). Eur Heart J. 2012; 33:1635-701. https://pubmed.ncbi.nlm.nih.gov/22555213
542. Marik PE, Varon J. Hypertensive crises: challenges and management. Chest. 2007; 131:1949-62. https://pubmed.ncbi.nlm.nih.gov/17565029
600. Baxter. Cardene IV Premixed injection (0.1 mg/mL) in either 4.8% dextrose or 0.86% sodium chloride prescribing information. Deerfield, IL; 2013 Jan.
601. Baxter. Cardene IV Premixed injection (0.2 mg/mL) in either 5% dextrose or 0.83% sodium chloride prescribing information. Deerfield, IL; 2013 Jan.
1150. Flynn JT, Kaelber DC, Baker-Smith CM et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017; 140 https://pubmed.ncbi.nlm.nih.gov/28827377
1200. Whelton PK, Carey RM, Aronow WS et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018; 71:el13-e115. https://pubmed.ncbi.nlm.nih.gov/29133356
1201. Bakris G, Sorrentino M. Redefining hypertension - assessing the new blood-pressure guidelines. N Engl J Med. 2018; 378:497-499. https://pubmed.ncbi.nlm.nih.gov/29341841
1202. Carey RM, Whelton PK, 2017 ACC/AHA Hypertension Guideline Writing Committee. Prevention, detection, evaluation, and management of high blood pressure in adults: synopsis of the 2017 American College of Cardiology/American Heart Association hypertension guideline. Ann Intern Med. 2018; 168:351-358. https://pubmed.ncbi.nlm.nih.gov/29357392
1207. Burnier M, Oparil S, Narkiewicz K et al. New 2017 American Heart Association and American College of Cardiology guideline for hypertension in the adults: major paradigm shifts, but will they help to fight against the hypertension disease burden?. Blood Press. 2018; 27:62-65. https://pubmed.ncbi.nlm.nih.gov/29447001
1209. Qaseem A, Wilt TJ, Rich R et al. Pharmacologic treatment of hypertension in adults aged 60 years or older to higher versus lower blood pressure targets: a clinical practice guideline from the American College of Physicians and the American Academy of Family Physicians. Ann Intern Med. 2017; 166:430-437. https://pubmed.ncbi.nlm.nih.gov/28135725
1210. SPRINT Research Group, Wright JT, Williamson JD et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015; 373:2103-16. https://pubmed.ncbi.nlm.nih.gov/26551272
1213. Reboussin DM, Allen NB, Griswold ME et al. Systematic review for the 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2017; https://pubmed.ncbi.nlm.nih.gov/29146534
1216. Taler SJ. Initial treatment of hypertension. N Engl J Med. 2018; 378:636-644. https://pubmed.ncbi.nlm.nih.gov/29443671
1220. Cifu AS, Davis AM. Prevention, detection, evaluation, and management of high blood pressure in adults. JAMA. 2017; 318:2132-2134. https://pubmed.ncbi.nlm.nih.gov/29159416
1222. Bell KJL, Doust J, Glasziou P. Incremental benefits and harms of the 2017 American College of Cardiology/American Heart Association high blood pressure guideline. JAMA Intern Med. 2018; 178:755-7. https://pubmed.ncbi.nlm.nih.gov/29710197
1223. LeFevre M. ACC/AHA hypertension guideline: what is new? what do we do?. Am Fam Physician. 2018; 97(6):372-3. https://pubmed.ncbi.nlm.nih.gov/29671534
1224. Brett AS. New hypertension guideline is released. From NEJM Journal Watch website. Accessed 2018 Jun 18. https://www.jwatch.org/na45778/2017/12/28/nejm-journal-watch-general-medicine-year-review-2017
1229. Ioannidis JPA. Diagnosis and treatment of hypertension in the 2017 ACC/AHA guidelines and in the real world. JAMA. 2018; 319(2):115-6. https://pubmed.ncbi.nlm.nih.gov/29242891
1250. Weir MR, Josselson J, Giard MJ et al. Sustained-release diltiazem compared with atenolol monotherapy for mild to moderate systemic hypertension. Am J Cardiol. 1987; 60:36-41I. https://pubmed.ncbi.nlm.nih.gov/3604943
1251. Muller FB, Bolli P, Erne P et al. Use of calcium antagonists as monotherapy in the management of hypertension. Am J Med. 1984; 77(Suppl 2B):11-5. https://pubmed.ncbi.nlm.nih.gov/6385691
1252. Kiowski W, Bühler FR, Fadayomi MO et al. Age, race, blood pressure and renin: predictors for antihypertensive treatment with calcium antagonists. Am J Cardiol. 1985; 56:81-5H.
1253. Frishman WH, Charlap S, Michelson EL. Calcium channel blockers in systemic hypertension. Am J Cardiol. 1986; 58:157-60. https://pubmed.ncbi.nlm.nih.gov/3524178
1254. Halperin AK, Cubeddu LX. The role of calcium channel blockers in the treatment of hypertension. Am Heart J. 1986; 111:363-82. https://pubmed.ncbi.nlm.nih.gov/3511651
1255. Laragh JH. Issues, goals, and guidelines in selecting first-line drug therapy for hypertension. In: The National Heart, Lung, and Blood Institute workshop on antihypertensive drug treatment. Bethesda, MD; June 11–12, 1987. Hypertension. 1989; 13(Suppl I):I-103-12. https://pubmed.ncbi.nlm.nih.gov/2490815
a. Roche Pharmaceuticals. Cardene (nicardipine hydrochloride) capsules prescribing information. Nutley, NJ; 1999 Sep.
b. Roche Pharmaceuticals. Cardene SR (nicardipine hydrochloride) sustained release capsules prescribing information. Nutley, NJ; 2000 Aug.
c. ESP Pharma. Cardene I.V. (nicardipine hydrochloride) prescribing information. Edison, NJ; 2002 Dec.
HID. Trissel LA. Handbook on injectable drugs. 17th ed. Bethesda, MD: American Society of Health-System Pharmacists; 2013:849-53.
Related/similar drugs
More about nicardipine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: calcium channel blockers
- Breastfeeding
- En español