Nabumetone (Monograph)
Drug class: Reversible COX-1/COX-2 Inhibitors
Warning
- Cardiovascular Risk
-
Increased risk of serious (sometimes fatal) cardiovascular thrombotic events (e.g., MI, stroke). Risk may occur early in treatment and may increase with duration of use.
-
Contraindicated in the setting of CABG surgery.
- GI Risk
-
Increased risk of serious (sometimes fatal) GI events (e.g., bleeding, ulceration, perforation of the stomach or intestine). Serious GI events can occur at any time and may not be preceded by warning signs and symptoms.
-
Geriatric patients are at greater risk for serious GI events.
Introduction
Prototypical NSAIA; prodrug with little pharmacologic activity until oxidized in the liver to form an active metabolite that is structurally similar to naproxen.
Uses for Nabumetone
Consider potential benefits and risks of nabumetone therapy as well as alternative therapies before initiating therapy with the drug. Use lowest effective dosage and shortest duration of therapy consistent with the patient’s treatment goals.
Inflammatory Diseases
Symptomatic treatment of osteoarthritis and rheumatoid arthritis.
Guidelines on the treatment of rheumatoid arthritis from the American College of Rheumatology (ACR) recommend initiation of a disease-modifying antirheumatic drug (DMARD) for most patients; role of NSAIAs not discussed.
ACR recommends topical/oral NSAIAs for treatment of osteoarthritis, among other interventions. Therapy selection is patient-specific; factors to consider include patients' values and preferences, risk factors for serious adverse GI effects, existing comorbidities (e.g., hypertension, heart failure, other cardiovascular disease, chronic kidney disease), injuries, disease severity, surgical history, and access to and availability of the interventions.
Nabumetone Dosage and Administration
General
Pretreatment Screening
-
Obtain baseline renal function assessment.
-
Obtain baseline hepatic function tests.
-
Obtain baseline CBC and chemistry profiles.
-
Inquire about pregnancy status in female patients.
Patient Monitoring
-
Monitor blood pressure during initiation of nabumetone and throughout therapy.
-
Monitor patients (including those without previous symptoms of cardiovascular disease) for the possible development of cardiovascular events, including cardiac ischemia and signs of worsening heart failure, throughout therapy.
-
Monitor for signs and symptoms of GI bleeding or ulceration.
-
Monitor for signs and symptoms of hepatotoxicity (e.g., nausea, fatigue, lethargy, diarrhea, pruritus, jaundice, right upper quadrant tenderness, flu-like symptoms).
-
Monitor renal function in patients with renal or hepatic impairment, heart failure, dehydration, diuretic use, or hypovolemia.
-
Monitor for changes in asthma signs and symptoms when using nabumetone in patients with preexisting asthma.
-
Perform periodic CBC and chemistry profiles in patients receiving long-term nabumetone therapy.
-
Monitor hemoglobin or hematocrit if signs and/or symptoms of anemia occur during therapy with nabumetone.
-
Monitor for signs and symptoms of serious skin reactions.
-
Inquire about pregnancy status in female patients.
Other General Considerations
-
Use the lowest effective dosage for the shortest duration consistent with individual patient treatment goals.
Administration
Oral Administration
Administer orally. Available as tablets. Administer with or without food.
Dosage
To minimize the potential risk of adverse cardiovascular and/or GI events, use lowest effective dosage and shortest duration of therapy consistent with the patient’s treatment goals. Adjust dosage based on individual requirements and response; attempt to titrate to the lowest effective dosage.
Adults
Inflammatory Diseases
Osteoarthritis
OralInitially, 1 g once daily. May increase dosage to 1.5–2 g daily, given as a single daily dose or 2 divided doses.
Patients weighing <50 kg may be less likely to need dosages >1 g daily.
Rheumatoid Arthritis
OralInitially, 1 g once daily. May increase dosage to 1.5–2 g daily, given as a single daily dose or 2 divided doses.
Patients weighing <50 kg may be less likely to need dosages >1 g daily.
Special Populations
Hepatic Impairment
No recommendations for dosage adjustment in patients with hepatic impairment. Impact of hepatic impairment on the efficacy of nabumetone is unknown.
Renal Impairment
No dosage adjustment is required in patients with mild renal insufficiency (Clcr ≥50 mL/minute). Dosage adjustment is warranted in patients with moderate renal impairment (Clcr 30 to 49 mL/minute). Not recommended for use in patients with severe renal impairment (Clcr <30 ml/minute).
If used in patients with moderate or severe renal insufficiency, do not exceed a starting dose of 750 mg or 500 mg, respectively, once daily. Increase to a higher daily dosage of 1.5 g in patients with moderate renal insufficiency or 1 g in patients with severe renal insufficiency only if close monitoring of renal function is possible.
Geriatric Patients
No recommendation for dosage adjustment in geriatric patients; however, increased monitoring for adverse effects is advised in this population.
Cytochrome P-450 Isoenzyme 2C9 Variants
Clinical Pharmacogenetics Implementation Consortium (CPIC) guidelines state that the pharmacokinetics of nabumetone are not significantly impacted by CYP2C9 genetic variants despite in vitro evidence indicating the role of CYP2C9 in metabolism of nabumetone’s active metabolite, 6-methoxy-2-naphthylacetic acid (6-MNA). The guideline does not make a recommendation to guide clinical practice on modifying the use of nabumetone in patients with CYP2C9 genetic variants.
Cautions for Nabumetone
Contraindications
-
Known hypersensitivity to the drug or any ingredient in the formulation.
-
History of asthma, urticaria, or other sensitivity reactions after taking aspirin or other nonsteroidal anti-inflammatory agents (NSAIAs).
-
Setting of coronary artery bypass graft (CABG) surgery.
Warnings/Precautions
Warnings
Cardiovascular Effects
A boxed warning regarding the increased risk of serious cardiovascular (CV) thrombotic events is included in the prescribing information for nabumetone. This increased risk may occur as early as the first weeks of treatment and has been observed most consistently at higher doses. To minimize the potential risk of adverse CV events in patients receiving NSAIAs, use the lowest effective dosage for the shortest possible duration. Monitor all patients for the possible development of CV events throughout therapy. Inform patients about the signs and symptoms of serious CV events, and instruct them to seek immediate medical attention if such symptoms occur. There is no consistent evidence that concomitant use of low-dose aspirin mitigates the increased risk of serious CV events associated with NSAIAs. Concomitant use of aspirin and an NSAIA, such as nabumetone, increases the risk for serious GI events. The incidence of myocardial infarction (MI) and stroke may be increased following CABG surgery. Do not use NSAIAs in the setting of CABG.
Gastrointestinal Effects
A boxed warning regarding the increased risk of serious GI events is included in the prescribing information for nabumetone. Serious, sometimes fatal, adverse GI effects including inflammation, bleeding, ulceration, and perforation of the stomach, small intestine, or large intestine can occur at any time in patients receiving NSAIAs, and such effects may not be preceded by warning signs or symptoms. Use extreme caution when using NSAIAs in patients with a prior history of ulcer disease or GI bleeding. Other risk factors for GI bleeding in patients treated with NSAIAs include the concomitant use of oral corticosteroids or anticoagulants, longer duration of NSAIA therapy, smoking, alcohol use, older age, and poor general health status. Most spontaneous reports of fatal GI effects have been in geriatric or debilitated patients. To minimize the potential risk of adverse GI effects, use the lowest effective dosage for the shortest possible duration. Closely monitor for signs and symptoms of GI ulceration and bleeding during NSAIA therapy. Promptly initiate additional evaluation and treatment if a serious adverse GI event is suspected and hold NSAIA therapy until a serious adverse GI event is ruled out. For high-risk patients, consider non-NSAIA therapy.
Other Warnings/Precautions
Post-MI Patients
Observational studies conducted in the Danish National Registry have demonstrated that patients who received NSAIAs in the post-MI period were at increased risk of reinfarction, cardiovascular-related death, and all-cause mortality beginning in the first week of treatment.
Avoid use of nabumetone in patients with recent MI unless the benefits of therapy are expected to outweigh the risk of recurrent cardiovascular thrombotic events; if nabumetone is used in such patients, monitor for signs of cardiac ischemia.
Hypertension
Use of NSAIAs, including nabumetone, can result in the onset of new hypertension or worsening of preexisting hypertension. Patients receiving NSAIAs may have an impaired response to thiazide or loop diuretics.
Use NSAIAs, including nabumetone, with caution in patients with hypertension. Monitor blood pressure closely during initiation of an NSAIA and throughout therapy.
Heart Failure and Edema
Use of COX-2 selective and nonselective NSAIAs may increase the risk of hospitalization for heart failure.
Fluid retention and edema may occur with NSAIA use. Use of nabumetone may blunt the CV effects of several therapeutic agents used to treat heart failure, such as diuretics, ACE inhibitors, or angiotensin receptor antagonists.
Avoid use of nabumetone in patients with severe heart failure unless the benefits of therapy are expected to outweigh the risk of worsening heart failure. If nabumetone is used in patients with severe heart failure, monitor for signs of worsening heart failure.
Renal Effects
Renal toxicity due to NSAIA use may occur in patients with impaired renal function, heart failure, hepatic dysfunction, those taking diuretics, and the elderly. Recovery of renal function to pretreatment levels usually occurs following discontinuance of NSAIA therapy.
Since no information from clinical trials is available on use of nabumetone in patients with advanced renal disease, use of nabumetone is not recommended in these patients. If nabumetone is initiated, monitor renal function closely.
Anaphylactoid Reactions
As with other NSAIAs, anaphylactoid reactions may occur in patients without known prior exposure to nabumetone. Do not give nabumetone to patients with the aspirin triad. This symptom complex typically occurs in asthmatic patients who experience rhinitis with or without nasal polyps, or who exhibit severe, potentially fatal bronchospasm after taking aspirin or other NSAIAs. Seek emergency help if an anaphylactoid reaction occurs.
Serious Skin Reactions
NSAIAs, including nabumetone can cause serious skin adverse reactions such as exfoliative dermatitis, Stevens-Johnson syndrome, fixed drug eruption, and toxic epidermal necrolysis, which can be fatal. These events can occur without warning.
Inform patients about the signs and symptoms of serious skin manifestations; use of nabumetone should be discontinued at the first appearance of skin rash or any other sign of hypersensitivity. Nabumetone is contraindicated in patients with previous serious skin reactions to NSAIAs.
Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS)
DRESS, a potentially fatal or life-threatening syndrome, has been reported in patients receiving NSAIAs, such as nabumetone. The typical, though not exclusive, clinical presentation of DRESS is fever, rash, lymphadenopathy, and/or facial swelling. Early manifestations of hypersensitivity (e.g., fever, lymphadenopathy) can present without an evident rash. If DRESS is suspected, discontinue nabumetone and evaluate the patient immediately.
Fetal/Neonatal Morbidity and Mortality
Use of NSAIAs, including nabumetone, during pregnancy at about 30 weeks’ gestation or later can cause premature closure of the fetal ductus arteriosus; use at about 20 weeks’ gestation or later has been associated with fetal renal dysfunction resulting in oligohydramnios and, in some cases, neonatal renal impairment.
Avoid use of NSAIAs, including nabumetone, in pregnant women at about 30 weeks’ gestation or later. If NSAIA therapy is necessary between about 20 and 30 weeks’ gestation, use the lowest effective dosage for the shortest possible duration. Consider ultrasound monitoring of amniotic fluid if nabumetone treatment extends beyond 48 hours. Discontinue nabumetone if oligohydramnios occurs and follow up according to clinical practice.
Hepatic Effects
Elevations in liver function tests and rare cases of severe hepatic reactions, including jaundice and fatal fulminant hepatitis, liver necrosis, and hepatic failure, have been reported. Evaluate patients with symptoms and/or signs suggesting liver dysfunction, or in whom an abnormal liver test has occurred for evidence of the development of a more severe hepatic reaction while taking nabumetone. Discontinue nabumetone if clinical signs and symptoms consistent with liver disease develop or if systemic manifestations, such as eosinophilia or rash, occur.
Hematologic Effects
Anemia, due to fluid retention, occult or gross GI blood loss, or an effect on erythropoiesis, may occur. If patients on long-term treatment with NSAIAs exhibit any signs or symptoms of anemia, check hemoglobin or hematocrit levels.
NSAIAs inhibit platelet aggregation and can prolong bleeding time in some patients. Monitor patients with coagulation disorders or receiving anticoagulants more closely while taking nabumetone.
Preexisting Asthma
Some patients with asthma may have aspirin-sensitive asthma and can experience severe, potentially fatal, bronchospasm if they receive aspirin. Since cross-reactivity, including bronchospasm, between aspirin and other NSAIAs has been reported in such aspirin-sensitive patients, do not administer nabumetone to patients with this form of aspirin sensitivity. Use caution in all patients with preexisting asthma.
Photosensitivity
Nabumetone may be associated with more reactions to sun exposure than might be expected based on skin tanning types.
Masking of Inflammation and Fever
The pharmacologic activity of nabumetone in reducing fever and inflammation may diminish the utility of these diagnostic signs in detecting complications of noninfectious, painful conditions.
Corticosteroid Insufficiency
Nabumetone is not a substitute for corticosteroids nor can it treat corticosteroid insufficiency. Avoid abrupt discontinuation of corticosteroids and manage corticosteroid use according to standard of care guidelines.
Pharmacogenomics
The manufacturer and the Clinical Pharmacogenetics Implementation Consortium Guideline (CPIC) for CYP2C9 and Nonsteroidal Anti-Inflammatory Drugs do not provide information on modification of nabumetone use based on pharmacogenetic testing. According to CPIC guidelines, nabumetone pharmacokinetics not significantly impacted by CYP2C9 genetic variants despite in vitro evidence of CYP2C9 role in 6-MNA metabolism.
Specific Populations
Pregnancy
Use of NSAIAs, including nabumetone, during pregnancy at about 30 weeks’ gestation or later increases the risk of premature closure of the fetal ductus arteriosus. NSAIA use at about 20 weeks’ gestation or later has been associated with fetal renal dysfunction resulting in oligohydramnios and, in some cases, neonatal renal impairment.
Nabumetone should be used in pregnancy only if the potential benefit justifies the potential fetal risk. If used, limit the dose and duration of nabumetone use between 20 and 30 weeks’ gestation. Avoid nabumetone use at about 30 weeks’ gestation and later in pregnancy.
The effects of nabumetone on labor and delivery are unknown.
Lactation
Active metabolite is distributed into milk in rats; not known whether nabumetone or its metabolites are distributed into milk in humans. Discontinue nursing or the drug.
Pediatric Use
Safety and efficacy not established in children.
Geriatric Use
Caution advised. Safety and efficacy profiles similar to those in younger adults.
Hepatic Impairment
Data are limited on the use of nabumetone in patients with severe hepatic impairment. Formation of 6-MNA, the active metabolite, and its metabolism to inactive metabolites may be reduced in patients with severe hepatic impairment.
Renal Impairment
No information is available on use of nabumetone in patients with advanced renal disease; use is not recommended in such patients. In patients with moderate renal impairment (Clcr 30 to 49 mL/minute), a 50% increase in unbound plasma 6-MNA (the active metabolite) occurs. The oxidized and conjugated metabolites of 6-MNA are renally eliminated.
If nabumetone is initiated in patients with moderate or advanced renal impairment, adjust the dose and monitor renal function closely.
Common Adverse Effects
Adverse effects reported in >3% of patients receiving nabumetone in clinical trials include diarrhea, dyspepsia, abdominal pain, constipation, flatulence, nausea, positive stool guaiac, dizziness, headache, pruritus, rash, tinnitus, and edema.
Drug Interactions
Protein-bound Drugs
Active metabolite, 6-MNA, could displace other protein-bound drugs from binding sites, and some drugs (e.g., aspirin) may displace 6-MNA.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
ACE inhibitors |
Reduced BP response to ACE inhibitor Use of nabumetone may blunt CV effects of ACE inhibitors and other drugs used to treat heart failure |
Monitor BP Monitor for signs of worsening heart failure. |
|
Angiotensin II receptor antagonists |
Use of nabumetone may blunt CV effects of angiotensin II receptor blockers (ARBs) and other drugs used to treat heart failure |
Monitor for signs of worsening heart failure. |
|
Antacids (aluminum-containing) |
No effect on 6-MNA bioavailability |
|
|
Aspirin |
Increased risk of GI ulceration and other complications No consistent evidence that low-dose aspirin mitigates the increased risk of serious cardiovascular events associated with NSAIAs When nabumetone tablets are administered with aspirin, its protein binding is reduced, but clearance of free nabumetone is not altered; clinical importance of this interaction unknown |
Manufacturer states that concomitant use not recommended |
|
Diuretics (furosemide, thiazides) |
Reduced natriuretic effects possible Possible deterioration of renal function in individuals with renal impairment Use of nabumetone may blunt CV effects of diuretics and other drugs used to treat heart failure |
Monitor for diuretic efficacy and renal failure Monitor for signs of worsening heart failure |
|
Lithium |
Increased plasma lithium concentrations |
Monitor for lithium toxicity |
|
Methotrexate |
Possible toxicity associated with increased plasma methotrexate concentrations |
Caution advised |
|
Warfarin |
Possibility of bleeding complications; 6-MNA may displace other protein-bound drugs (e.g., warfarin) from their binding site |
Caution advised |
Nabumetone Pharmacokinetics
Absorption
Bioavailability
Well absorbed following oral administration.
Rapidly biotransformed to active metabolite, 6-MNA; mean time to maximum concentration of 6-MNA: 2.5–4 hours.
Unchanged nabumetone is not detected in plasma.
Food
Food increases rate of nabumetone absorption; increases rate but not extent of metabolism to 6-MNA.
Peak plasma 6-MNA concentrations increased by approximately one-third.
Distribution
Extent
Unknown if distributed into human milk.
Plasma Protein Binding
6-MNA: >99%.
Elimination
Metabolism
Approximately 35% of a 1-g dose is metabolized to the active metabolite, 6-MNA.
6-MNA is hepatically metabolized via conjugation and O-demethylation to inactive metabolites; 6-MNA does not appear to undergo enterohepatic recirculation.
Elimination Route
Urine: 75% recovered at 48 hours; 80% recovered at 168 hours
Feces: 9%
Half-life
6-MNA: approximately 24 hours.
Special Populations
In patients with moderate renal impairment (Clcr 30–49 mL/minute) and severe renal impairment (Clcr <30 mL/minute), elimination half-life and plasma levels of 6-MNA increased.
In geriatric patients, steady-state plasma 6-MNA concentrations are higher than in younger individuals.
Stability
Storage
Oral
Tablets
20-25°C ; excursions permitted between 15–30°C for generic tablets.
Actions
-
Inhibits cyclooxygenase-1 (COX-1) and COX-2.
-
Pharmacologic actions similar to those of other prototypical NSAIAs; exhibits anti-inflammatory, analgesic, and antipyretic activity.
Advice to Patients
-
Advise patients to read the FDA-approved patient labeling (Medication Guide).
-
Advise patients to be alert for symptoms of serious cardiovascular thrombotic events. Advise patients to seek immediate medical attention if signs and symptoms of a cardiovascular event (e.g., chest pain, dyspnea, weakness, slurred speech) occur.
-
Advise patients to report symptoms of GI ulcerations and bleeding (e.g., epigastric pain, dyspepsia, melena, hematemesis) to their healthcare provider. Inform patients receiving concomitant low-dose aspirin of the increased risk of GI bleeding.
-
Instruct patients to stop taking nabumetone immediately if they develop any type of rash or fever and to promptly contact their clinician.
-
Advise patients to seek emergency medical attention if signs of an anaphylactic reaction occur (e.g., difficulty breathing, swelling of the face or throat).
-
Inform patients of the signs and symptoms of hepatotoxicity. Advise patients to discontinue therapy and contact their clinician immediately if signs and symptoms of hepatotoxicity (e.g., nausea, fatigue, lethargy, pruritus, jaundice, upper right quadrant tenderness, flu-like symptoms) occur.
-
Inform patients of the risk of heart failure or edema and the importance of reporting dyspnea, unexplained weight gain, or edema.
-
Advise women to inform their clinician if they are or plan to become pregnant or plan to breast-feed. Advise pregnant women to avoid nabumetone and other NSAIAs beginning at 30 weeks’ gestation because of the risk of premature closure of the fetal ductus arteriosus; monitoring for oligohydramnios may be necessary if NSAIA therapy is required for >48 hours’ duration between about 20 and 30 weeks’ gestation.
-
Advise patients to inform their clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary and herbal supplements, as well as any concomitant illnesses.
-
Advise patients that concomitant use of other NSAIAs with nabumetone provides little or no increase in efficacy but increases risk of GI toxicity and is not recommended.
-
Advise patients not to use concomitant low-dose aspirin without consulting their clinician.
-
Alert patients to the presence of NSAIAs in many OTC drugs.
-
Advise patients of other precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
500 mg* |
Nabumetone Tablets |
|
|
750 mg* |
Nabumetone Tablets |
|||
|
1 g* |
Nabumetone Tablets |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions March 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
More about nabumetone
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (93)
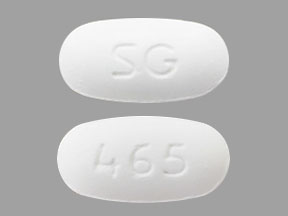
- Drug images
- Latest FDA alerts (4)
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: Nonsteroidal anti-inflammatory drugs
- Breastfeeding
- En español