Mosunetuzumab-axgb (Monograph)
Brand name: Lunsumio
Drug class: Antineoplastic Agents
Warning
- Cytokine Release Syndrome (CRS)
-
Cytokine release syndrome (CRS), including serious or life-threatening reactions, can occur in patients receiving mosunetuzumab-axgb.
-
Initiate treatment with the step-up dosing schedule to reduce risk of CRS.
-
If CRS occurs, withhold mosunetuzumab-axgb until CRS resolves or permanently discontinue based on severity.
Introduction
Antineoplastic agent; bispecific CD20-directed CD3 T-cell engager.
Uses for Mosunetuzumab-axgb
Follicular Lymphoma
Treatment of relapsed or refractory follicular lymphoma in adults who previously received ≥2 lines of systemic therapy (designated an orphan drug by FDA for this use).
Current indication approved under accelerated approval based on response rate; continued FDA approval for this indication may be contingent on verification and description of clinical benefit in a confirmatory trial.
Mosunetuzumab-axgb Dosage and Administration
General
Pretreatment Screening
-
Ensure adequate hydration to reduce risk of cytokine release syndrome (CRS).
-
Rule out active infection prior to initiating therapy; use caution in patients with a history of recurring/chronic infections, underlying conditions that may predispose to infections, or significant prior immunosuppressive treatment.
-
Verify pregnancy status in females of reproductive potential.
Patient Monitoring
-
Monitor for CRS and infusion-related reactions.
-
Monitor for signs and symptoms of neurologic toxicity, including immune effector cell-associated neurotoxicity (ICANS).
-
Monitor for signs and symptoms of infection.
-
Monitor CBC throughout treatment for neutropenia, anemia, and/or thrombocytopenia.
-
Monitor for signs and symptoms of compression or obstruction due to mass effect secondary to tumor flare, particularly in patients with bulky tumors or disease located in close proximity to airways or a vital organ.
Premedication and Prophylaxis
-
Administer prophylactic antimicrobials according to current guidelines.
-
Premedication to reduce risk of CRS and infusion-related reactions recommended (see Premedications under Dosage and Administration).
Administration
IV Administration
Administer via IV infusion.
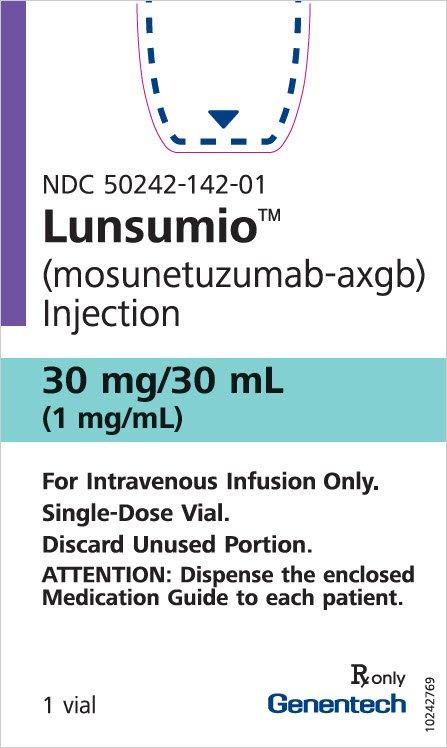
Available in single-dose vials containing mosunetuzumab-axgb 1 mg/mL solution.
Dilution required prior to use.
Administration by a qualified healthcare professional required with appropriate medical support to manage severe reactions such as CRS and neurologic toxicity.
Administer through a dedicated infusion line; do not use an in-line filter. May use drip chamber filters for administration.
Dilution
Determine the dose, total volume of mosunetuzumab-axgb solution required, and the number of vials needed. Obtain infusion bag of 0.9% sodium chloride or 0.45% sodium chloride; withdraw volume of solution equal to the volume of mosunetuzumab-axgb required for the patient’s dose and discard. Only use infusion bags made of polyvinyl chloride (PVC) or polyolefin such as polyethylene and polypropylene.
Withdraw required volume of mosunetuzumab-axgb from vial and dilute into the infusion bag of 0.9% sodium chloride or 0.45% sodium chloride as noted in Table 1. Discard any unused portion.
|
Dose |
Volume of Mosunetuzumab-axgb in 0.9% or 0.45% Sodium Chloride Solution |
Size of Infusion Bag |
|---|---|---|
|
1 mg |
1 mL |
50 mL or 100 mL |
|
2 mg |
2 mL |
50 mL or 100 mL |
|
60 mg |
60 mL |
100 mL or 250 mL |
|
30 mg |
30 mL |
50 mL, 100 mL, or 250 mL |
Gently mix by slow inversion. Do not shake.
Apply peel-off label from package insert to the infusion bag.
Rate of Administration
Administer over a minimum of 4 hours during cycle 1. If infusions during cycle 1 are well-tolerated, may administer infusions in subsequent treatment cycles over 2 hours.
Premedications
Premedication recommended to prevent CRS and infusion-related reactions; specific recommendations for premedication summarized in Table 2.
|
Treatment Cycle |
Patients Requiring Premedication |
Premedication |
Dosage |
Administration |
|---|---|---|---|---|
|
Cycle 1 and Cycle 2 |
All patients |
Corticosteroid |
Dexamethasone 20 mg IV or methylprednisolone 80 mg IV |
Complete at least 1 hour prior to infusion |
|
Cycle 1 and Cycle 2 |
All patients |
Antihistamine |
Diphenhydramine 50–100 mg or equivalent oral or IV antihistamine |
At least 30 minutes prior to infusion |
|
Cycle 1 and Cycle 2 |
All patients |
Antipyretic |
Oral acetaminophen (500–1000 mg) |
At least 30 minutes prior to infusion |
|
Cycles 3+ |
Patients who experienced any grade CRS with the previous dose |
Corticosteroid |
Dexamethasone 20 mg IV or methylprednisolone 80 mg IV |
Complete at least 1 hour prior to infusion |
|
Cycles 3+ |
Patients who experienced any grade CRS with the previous dose |
Antihistamine |
Diphenhydramine 50–100 mg or equivalent oral or IV antihistamine |
At least 30 minutes prior to infusion |
|
Cycles 3+ |
Patients who experienced any grade CRS with the previous dose |
Antipyretic |
Oral acetaminophen (500–1000 mg) |
At least 30 minutes prior to infusion |
Dosage
Adults
Follicular Lymphoma
IV
Recommended dosage based on treatment cycle and day (see Table 3). Usual treatment duration is 8 cycles, unless unacceptable toxicity or disease progression occurs. Administer additional 9 cycles of treatment in patients who achieve partial response or have stable disease after the first 8 cycles, unless unacceptable toxicity or disease progression occurs.
|
Treatment Cycle |
Day of Treatment |
Dose of Mosunetuzumab-axgb |
Rate of Infusion |
|---|---|---|---|
|
Cycle 1 |
Day 1 |
1 mg |
Administer over a minimum of 4 hours |
|
Cycle 1 |
Day 8 |
2 mg |
Administer over a minimum of 4 hours |
|
Cycle 1 |
Day 15 |
60 mg |
Administer over a minimum of 4 hours |
|
Cycle 2 |
Day 1 |
60 mg |
Administer over 2 hours if infusions from Cycle 1 were well tolerated |
|
Cycle 3+ |
Day 1 |
30 mg |
Administer over 2 hours if infusions from Cycle 1 were well tolerated |
Dosage Modification for Toxicity
Patients who experience CRS, neurologic toxicity, or other adverse reactions may require dosage adjustment, dose delay, or treatment discontinuation, depending on severity. Recommendations for management of CRS, neurologic toxicity, and other adverse reactions summarized in Tables 4, 5, and 6, respectively. If restarting mosunetuzumab-axgb after a dose delay, follow dosage recommendations in Table 7.
Identify CRS based on clinical presentation. Evaluate for and treat other causes of fever, hypoxia, and hypotension. If CRS is suspected, hold mosunetuzumab-axgb until CRS resolves and manage according to recommendations in Table 4. Administer supportive therapy for CRS, including intensive care if warranted. If CRS is refractory to management, consider other causes, including hemophagocytic lymphohistiocytosis.
Premedication may mask fever; if clinical presentation is consistent with CRS, follow these management guidelines.
Refer to Table 7 for information on restarting after dose delays.
Low-flow oxygen defined as oxygen delivered at <6 L/min; high-flow oxygen defined as oxygen delivered at ≥6 L/min.
|
Severity |
Presenting Symptoms |
Actions |
|---|---|---|
|
Grade 1 |
Fever ≥38°C |
Withhold infusion and manage per current practice guidelines; if symptoms resolve, restart infusion at the same rate. Ensure CRS symptoms are resolved for at least 72 hours prior to the next dose. Administer premedication prior to next dose and monitor more frequently. |
|
Grade 2 |
Fever ≥38°C with hypotension not requiring vasopressors and/or hypoxia requiring low-flow oxygen by nasal cannula or blow-by |
Withhold infusion and manage per current practice guidelines; if symptoms resolve, restart infusion at 50% rate. Ensure CRS symptoms are resolved for at least 72 hours prior to the next dose. Administer premedication prior to next dose and consider infusing the next dose at 50% rate. For the next dose, monitor more frequently and consider hospitalization. For recurrent Grade 2 CRS, manage as Grade 3 CRS. |
|
Grade 3 |
Fever ≥38°C with hypotension requiring a vasopressor (with or without vasopressin) and/or hypoxia requiring high-flow oxygen by nasal cannula, face mask, non-rebreather mask, or Venturi mask |
Withhold infusion, manage per current practice guidelines, and provide supportive therapy, which may include intensive care. Ensure CRS symptoms are resolved for at least 72 hours prior to the next dose. Administer premedication prior to next dose and infuse the next dose at 50% rate. Hospitalize for the next dose. For recurrent Grade 3 CRS, permanently discontinue. Manage CRS per current practice guidelines and provide supportive therapy, which may include intensive care. |
|
Grade 4 |
Fever ≥38°C with hypotension requiring multiple vasopressors (excluding vasopressin) and/or hypoxia requiring oxygen by positive pressure (e.g., CPAP, BiPAP, intubation and mechanical ventilation) |
Permanently discontinue. Manage CRS per current practice guidelines and provide supportive therapy, which may include intensive care. |
At first sign of neurologic toxicity, including ICANS, hold mosunetuzumab-axgb and consider neurology evaluation. Manage as recommended in Table 5. Rule out other causes of neurologic symptoms. Provide supportive therapy, which may include intensive care.
Refer to Table 7 for information on restarting after dose delays.
|
Severity |
Actions |
|---|---|
|
Grade 2 |
Withhold until neurologic toxicity symptoms improve to Grade 1 or baseline for at least 72 hours. Provide supportive therapy. If ICANS, manage per current practice guidelines. |
|
Grade 3 |
Withhold until neurologic toxicity symptoms improve to Grade 1 or baseline for at least 72 hours. Provide supportive therapy, which may include intensive care, and consider neurology evaluation. If ICANS, manage per current practice guidelines. If recurrence, permanently discontinue. |
|
Grade 4 |
Permanently discontinue. Provide supportive therapy, which may include intensive care, and consider neurology evaluation. If ICANS, manage per current practice guidelines. |
Manage adverse events other than CRS or neurologic toxicity as recommended in Table 6.
Refer to Table 7 for information on restarting after dose delays.
|
Adverse Reaction |
Severity |
Actions |
|---|---|---|
|
Infections |
Grades 1–4 |
Withhold in patients with active infection until the infection resolves. For Grade 4 infection, consider permanent discontinuation. |
|
Neutropenia |
Absolute neutrophil count <500 cells/mm3 |
Withhold until absolute neutrophil count is ≥500 cells/mm3. |
|
Other Adverse Reactions |
Grade 3 or higher |
Withhold until the toxicity resolves to Grade 1 or baseline. |
Table 7 provides recommendations on restarting therapy after dose delay due to toxicity.
For the Day 1, Day 8, and Day 15 doses in the next cycle, administer premedication for all patients.
|
Last Dose Administered |
Time Since Last Dose |
Action for Next Dose |
|---|---|---|
|
1 mg Cycle 1 Day 1 |
1–2 weeks |
Administer 2 mg (Cycle 1 Day 8), then resume the planned treatment schedule |
|
1 mg Cycle 1 Day 1 |
>2 weeks |
Repeat 1 mg (Cycle 1 Day 1), then administer 2 mg (Cycle 1 Day 8) and resume the planned treatment schedule |
|
2 mg Cycle 1 Day 8 |
1–2 weeks |
Administer 60 mg (Cycle 1 Day 15), then resume the planned treatment schedule |
|
2 mg Cycle 1 Day 8 |
>2 weeks and <6 weeks |
Repeat 2 mg (Cycle 1 Day 8), then administer 60 mg (Cycle 1 Day 15) and resume the planned treatment schedule |
|
2 mg Cycle 1 Day 8 |
≥6 weeks |
Repeat 1 mg (Cycle 1 Day 1) and 2 mg (Cycle 1 Day 8), then administer 60 mg (Cycle 1 Day 15) and resume the planned treatment schedule |
|
60 mg Cycle 1 Day 15 |
1 week to <6 weeks |
Administer 60 mg (Cycle 2 Day 1), then resume the planned treatment schedule |
|
60 mg Cycle 1 Day 15 |
≥6 weeks |
Repeat 1 mg (Cycle 2 Day 1) and 2 mg (Cycle 2 Day 8), then administer 60 mg (Cycle 2 Day 15), followed by 30 mg (Cycle 3 Day 1) and resume the planned treatment schedule |
|
60 mg Cycle 2 Day 1 |
3 weeks to <6 weeks |
Administer 30 mg (Cycle 3 Day 1), then resume the planned treatment schedule |
|
60 mg Cycle 2 Day 1 |
≥6 weeks |
Repeat 1 mg (Cycle 3 Day 1) and 2 mg (Cycle 3 Day 8), then administer 30 mg (Cycle 3 Day 15), followed by 30 mg (Cycle 4 Day 1) and resume the planned treatment schedule |
|
30 mg Cycle 3 onwards |
3 weeks to <6 weeks |
Administer 30 mg then resume the planned treatment schedule |
|
30 mg Cycle 3 onwards |
≥6 weeks |
Repeat 1 mg on Day 1 and 2 mg on Day 8 during the next cycle, then administer 30 mg on Day 15, followed by 30 mg on Day 1 of subsequent cycles |
Special Populations
Hepatic Impairment
No dosage recommendations at this time.
Renal Impairment
No dosage recommendations at this time.
Geriatric Patients
No dosage recommendations at this time.
Cautions for Mosunetuzumab-axgb
Contraindications
-
None.
Warnings/Precautions
Warnings
Cytokine Release Syndrome (CRS)
Serious or life-threatening cases of CRS reported (see Boxed Warning). CRS occurs most often during first treatment cycle, but may also occur in subsequent treatment cycles.
Time from start of mosunetuzumab administration to CRS onset ranges from 0.1 hours to 16 days. Median duration of CRS is 3 days.
Signs and symptoms include, but not limited to, fever, chills, hypotension, tachycardia, hypoxia, and headache.
Initiate mosunetuzumab treatment using the recommended step-up dosing schedule to reduce risk of CRS. Administer pretreatment medications, ensure adequate hydration, and monitor patients closely following administration.
At first sign of CRS, immediately evaluate patients for hospitalization, manage per current practice guidelines, and administer supportive care. Withhold mosunetuzumab until CRS resolves or permanently discontinue depending on severity.
Advise patients experiencing CRS or other adverse events that impair consciousness to avoid driving or operating heavy or potentially dangerous machinery until resolution.
Other Warnings/Precautions
Neurologic Toxicity, Including Immune Effector Cell-Associated Neurotoxicity Syndrome
Serious and life-threatening neurologic toxicity, including immune effector cell-associated neurotoxicity syndrome (ICANS), reported.
Coadministration with other products that cause dizziness or mental status changes may increase risk.
Monitor for signs and symptoms. At first sign of neurologic toxicity, including ICANS, immediately evaluate patient, consider neurology evaluation as appropriate, and provide supportive care based on severity. Withhold or permanently discontinue treatment based on severity and follow management recommendations.
Initiate neurology evaluation for patients who experience tremors, dizziness, insomnia, severe neurotoxicity, or any other adverse reactions that impair consciousness.
Advise patients at increased risk to avoid driving and refrain from operating heavy or dangerous machinery until resolution.
Infections
Serious or fatal infections reported.
Monitor for signs and symptoms of infection prior to and during treatment.
Do not administer during active infection. Use caution in patients with a history of recurring or chronic infections (e.g., chronic, active Epstein-Barr Virus), underlying conditions that may predispose to infections, or significant prior immunosuppressive treatment.
Administer prophylactic antimicrobials according to guidelines.
Withhold or consider permanent discontinuation based on infection severity.
Hemophagocytic Lymphohistiocytosis
Fatal or serious hemophagocytic lymphohistiocytosis (HLH) reported. Common manifestations include fever, elevated ferritin, hemophagocytosis, cytopenias, coagulopathy, hepatitis, and splenomegaly.
Monitor patients for clinical signs and symptoms of HLH. Consider HLH diagnosis when CRS presentation is atypical or prolonged, or when there are features of macrophage activation. If HLH suspected, interrupt therapy and evaluate and treat the patient promptly per practice guidelines.
Cytopenias
Serious or severe cytopenias, including neutropenia, anemia, and thrombocytopenia, reported.
Monitor CBC during treatment. Based on severity of cytopenias, temporarily withhold or permanently discontinue mosunetuzumab-axgb.
Consider prophylactic granulocyte colony-stimulating factor administration as applicable.
Tumor Flare
Serious or severe tumor flare reported.
Monitor for signs and symptoms of compression or obstruction due to mass effect secondary to tumor flare, particularly in patients with bulky tumors or disease located in close proximity to airways or a vital organ. If compression or obstruction develops, institute standard treatment.
Fetal/Neonatal Morbidity and Mortality
Based on mechanism of action, may cause fetal harm when administered to a pregnant woman. No human or animal data available; however, immune activation by mosunetuzumab may compromise pregnancy maintenance, and exposure to the drug in utero may cause B-cell lymphocytopenia in infants.
Advise pregnant women of potential risk to the fetus. Verify pregnancy status in females of reproductive potential prior to initiating mosunetuzumab-axgb. Advise females of reproductive potential to use effective contraception during treatment and for 3 months after last dose.
Immunogenicity
No patients developed anti-mosunetuzumab antibodies in up to 12 months of treatment.
Specific Populations
Pregnancy
No available data in pregnant women to evaluate for drug-associated risk.
Based on mechanism of action, may cause fetal harm.
Mosunetuzumab causes T-cell activation and cytokine release; immune activation may compromise pregnancy maintenance. Based on expression of CD20 on B cells and finding of B cell depletion in non-pregnant animals, the drug may also cause B-cell lymphocytopenia in infants exposed in utero. Mosunetuzumab may be transmitted from the mother to the developing fetus.
Advise women of the potential fetal risk. Verify pregnancy status in females of reproductive potential prior to initiating the drug.
Lactation
No available data regarding presence of mosunetuzumab in human milk, effects on the breast-fed infant, or effects on milk production. Because human IgG is present in human milk, and potential exists for drug absorption leading to B-cell depletion, advise women not to breast-feed during treatment and for 3 months after last dose.
Females and Males of Reproductive Potential
Verify pregnancy status in females of reproductive potential prior to initiating mosunetuzumab.
Advise females of reproductive potential to use effective contraception during treatment and for 3 months after the last dose.
Pediatric Use
Safety and effectiveness not established.
Geriatric Use
Insufficient data in patients ≥65 years of age to assess whether there are differences in safety or effectiveness compared to younger adult patients.
Hepatic Impairment
No clinically significant differences in the pharmacokinetics of mosunetuzumab in mild hepatic impairment (total bilirubin ≤ ULN with AST >ULN OR total bilirubin >1 to 1.5 times ULN with any AST level). Pharmacokinetic effects of moderate to severe hepatic impairment (total bilirubin >1.5 times ULN with any AST) unknown.
Renal impairment
No clinically significant differences in pharmacokinetics of mosunetuzumab in mild or moderate renal impairment (Clcr 30–89 mL/minute). Pharmacokinetic effects of severe renal impairment (Clcr 15–29 mL/minute) unknown.
Common Adverse Effects
Most common adverse reactions (≥20%): CRS, fatigue, rash, pyrexia, headache.
Most common Grade 3 to 4 laboratory abnormalities (≥10%): decreased lymphocyte count, decreased phosphate, increased glucose, decreased neutrophil count, increased uric acid, decreased white blood cell count, decreased hemoglobin, decreased platelets.
Drug Interactions
No clinical drug interaction studies conducted.
Drugs Metabolized by Hepatic Microsomal Enzymes
Activity of CYP enzymes may be suppressed, resulting in increased exposure of CYP substrates. Increased exposure more likely to occur after the first dose of mosunetuzumab-axgb on Cycle 1 Day 1, up to 14 days after the second 60 mg dose on Cycle 2 Day 1, and during and after cytokine release syndrome (CRS).
Monitor for toxicity or concentrations of CYP substrates where minimal concentration changes may lead to serious adverse reactions. Consult the concomitant CYP substrate drug’s prescribing information for recommended dosage modification.
Mosunetuzumab-axgb Pharmacokinetics
Absorption
Bioavailability
Pharmacokinetics dose proportional over range of 0.2–60 mg.
Steady state achieved by Cycle 4 (63–84 days).
Special Populations
Pharmacokinetics not impacted by age (19–96 years), sex, race, and ethnicity.
Distribution
Extent
Unknown if distributed into human milk.
Elimination
Half-life
16.1 days.
Stability
Storage
Parenteral
Injection Concentrate, for IV Infusion
Unopened vials: 2–8°C in original carton to protect from light.
Diluted solution: use immediately. If not used immediately, may refrigerate at 2–8°C for up to 24 hours or store at ambient temperature (9–30°C) for up to 16 hours. Bring to room temperature prior to infusion.
Actions
-
T-cell engaging bispecific antibody that binds to the CD3 receptor (expressed on the surface of T cells) and CD20 (expressed on the surface of lymphoma cells and some healthy B-lineage cells).
-
Activates T cells, causes release of proinflammatory cytokines, and induces lysis of B cells.
-
After administration of recommended mosunetuzumab-axgb dosage, peripheral B-cell counts decreased to undetectable levels in 92% of patients by Cycle 2 Day 1; sustained depletion observed at Cycle 4 and Cycle 8.
-
Induces hypogammaglobulinemia in some patients.
-
Transient elevations in plasma cytokine concentrations observed after administration; levels generally returned to baseline prior to next infusion.
Advice to Patients
-
Advise patients to read the FDA-approved patient labeling (Medication Guide).
-
Advise patients to seek immediate medical attention if they develop signs or symptoms associated with cytokine release syndrome (CRS), including fever, chills, hypotension, tachycardia, hypoxia, and headache. Advise patients to avoid driving or operating heavy or dangerous machinery if they experience symptoms that impair consciousness.
-
Advise patients to immediately contact their healthcare provider if they develop signs and symptoms associated with neurologic toxicity, including immune effector cell-associated neurotoxicity syndrome (ICANS), headache, peripheral neuropathy, dizziness, or mental status changes. Advise patients to avoid driving or operating heavy or dangerous machinery if they experience neurologic toxicity that impairs consciousness.
-
Inform patients about the signs and symptoms of hemophagocytic lymphohistiocytosis including fever, coagulopathy, cytopenias, and splenomegaly.
-
Inform patients about signs and symptoms of infection.
-
Inform patients about signs and symptoms of cytopenias, including neutropenia, febrile neutropenia, anemia, and thrombocytopenia.
-
Advise patients to report any signs and symptoms of tumor flare to their healthcare provider.
-
Advise patients to inform their clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as any concomitant illnesses.
-
Advise patients to inform their clinician if they are or plan to become pregnant. Advise pregnant women of the potential fetal risk. Advise females of reproductive potential to use effective contraception during treatment and for 3 months after the last dose.
-
Advise patients to inform their clinician if they plan to breast-feed. Advise patients not to breast-feed during treatment and for 3 months after the last dose.
-
Advise patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Concentrate, for injection, for IV infusion |
1 mg/mL (1 mg and 30 mg) |
Lunsumio (available in single-dose vials) |
Genentech |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions April 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
More about mosunetuzumab
- Check interactions
- Compare alternatives
- Reviews (1)
- Side effects
- Dosage information
- During pregnancy
- Drug class: bispecific T-cell engagers (BiTE)
- Breastfeeding
- En español