Metoclopramide Hydrochloride (Monograph)
Brand names: Gimoti, Reglan
Drug class: Prokinetic Agents
Warning
- Tardive Dyskinesia
-
May result in tardive dyskinesia. Risk increases with increasing duration of therapy and total cumulative dose.
-
Discontinue metoclopramide in patients who develop signs or symptoms of tardive dyskinesia. Symptoms may lessen or resolve in some patients after discontinuance.
-
Avoid treatment durations >12 weeks because of increased risk of developing tardive dyskinesia with longer-term use.
Introduction
Antiemetic; stimulant of upper GI motility (prokinetic agent); dopamine D2-receptor antagonist.
Uses for Metoclopramide Hydrochloride
Diabetic Gastroparesis
Symptomatic treatment of acute and recurrent diabetic gastric stasis (gastroparesis). Therapy should not exceed 12 weeks’ duration because of the risk for developing tardive dyskinesia with longer-term use.
Metoclopramide is the only approved drug therapy for diabetic gastroparesis, but evidence supporting its use is weak; given the potential for serious adverse events (e.g., acute dystonic reactions, drug-induced parkinsonism, akathisia, tardive dyskinesia), the American Diabetes Association recommends reserving use for severe cases of diabetic gastroparesis that are unresponsive to other therapies. The American College of Gastroenterology (ACG) suggests metoclopramide over no treatment for management of refractory gastroparesis symptoms.
Cancer Chemotherapy-induced Nausea and Vomiting
Used parenterally for the prevention of nausea and vomiting associated with emetogenic cancer chemotherapy.
Has been used orally† [off-label] for the prevention of chemotherapy-induced nausea and vomiting.
No longer routinely used for prophylaxis of chemotherapy-induced nausea and vomiting; other drugs with fewer adverse effects now preferred (some experts state that metoclopramide may still be a reasonable prophylactic option in patients receiving low emetic risk chemotherapy).
American Society of Clinical Oncology (ASCO) states metoclopramide may be an option for treatment of breakthrough nausea and vomiting† [off-label] in patients who received prophylactic antiemetic therapy with drugs from a different therapeutic class .
Intubation of the Small Intestine
Used parenterally to facilitate small intestine intubation in adults and pediatric patients when the tube (e.g., endoscope, biopsy tube) does not pass through the pylorus with conventional maneuvers.
Radiographic Examination of the Upper GI Tract
Used parenterally to stimulate gastric emptying and intestinal transit of barium when delayed emptying interferes with radiographic examination of the stomach and/or small intestine.
Gastroesophageal Reflux
Short-term (4–12 weeks) relief of symptomatic, documented gastroesophageal reflux in adults who are unresponsive to conventional therapy.
Use typically reserved for patients with GERD and concomitant gastroparesis. ACG recommends against treatment of GERD with any prokinetic agent (e.g., metoclopramide) unless there is objective evidence of gastroparesis. The American Gastroenterological Association (AGA) recommends against the use of metoclopramide for treatment of GERD, and states that prokinetic agents have not been shown to be useful in GERD (but may be useful for concomitant gastroparesis).
Other Uses
Prevention of postoperative nausea and vomiting when nasogastric suction is considered undesirable (evidence limited, but may be useful if other dopamine antagonists not available).
Has been used for aspiration prophylaxis in patients undergoing anesthesia† [off-label] (routine use not recommended, but may be considered for patients at high risk of aspiration and patients undergoing cesarean delivery or postpartum tubal ligation).
Has been used for the symptomatic treatment of acute and chronic postsurgical gastroparesis† [off-label] following vagotomy and gastric resection or vagotomy and pyloroplasty. Has been used for gastroparesis related to other conditions (nondiabetic gastroparesis† [off-label]).
Has been used for the management of migraine†. Some experts state that IV metoclopramide may be considered for relief of migraine pain.
Has been used for breakthrough nausea and vomiting associated with low or minimal emetic risk radiation therapy† .
Option for the treatment of nausea and vomiting in pregnancy† in patients not responding to first-line antiemetic therapies.
Has been used for nausea and vomiting due to other causes† (evidence limited). Has been used for the management of intractable hiccups† and to promote lactation† .
Metoclopramide Hydrochloride Dosage and Administration
General
Patient Monitoring
-
Monitor patients with hepatic impairment for fluid retention and volume overload while receiving metoclopramide.
-
In patients receiving concomitant drugs with possible diminished GI absorption by metoclopramide, monitor for reduced efficacy.
-
Monitor blood glucose concentrations and adjust insulin as necessary in patients with insulin-controlled diabetes mellitus.
Other General Considerations
-
Avoid use of metoclopramide if patients are receiving other drug therapies that are likely to cause tardive dyskinesia (e.g., antipsychotic agents).
-
Patients with cytochrome-b5 reductase deficiency who receive metoclopramide have an increased risk of methemoglobinemia and/or sulfhemoglobinemia. Patients with glucose-6-phosphate dehydrogenase (G6PD) deficiency who develop metoclopramide-induced methemoglobinemia should not receive methylene blue therapy due to the risk of potentially fatal hemolytic anemia.
-
Some formulations of metoclopramide oral solution may contain the dye tartrazine (FD&C yellow No. 5), which may cause allergic reactions including bronchial asthma in susceptible individuals.
-
Advise patients who must restrict their intake of phenylalanine that the 5- and 10-mg orally disintegrating tablets contain aspartame (metabolized to phenylalanine).
Administration
Administer orally, intranasally, by direct IV injection or IV infusion, or IM.
Metoclopramide therapy, including all dosage forms and routes of administration, should not exceed 12 weeks’ duration because of risk of tardive dyskinesia with longer-term use.
Oral Administration
Oral formulations of metoclopramide are recommended for use in adults only.
Administer orally on an empty stomach (at least 30 minutes before eating) as conventional tablets, oral solution, or orally disintegrating tablets. At least one manufacturer states that dose should not be repeated if inadvertently administered with food.
Orally Disintegrating Tablets
Remove tablet from the blister packaging with dry hands and immediately place it on the tongue. Tablet should disintegrate in approximately one minute (range: 10 seconds to 14 minutes); swallow the granules without water. Discard any tablet that breaks or crumbles during handling.
The 5- and 10-mg orally disintegrating tablets contain aspartame (metabolized to phenylalanine).
Intranasal Administration
Metoclopramide nasal spray is recommended for use in adults only.
Commercially available in a bottle with a metered-dose spray pump attachment for administration by nasal inhalation. For information on administration technique, consult manufacturer's instructions for use.
Prime the pump prior to first use or if not used for ≥2 weeks.
IV Administration
Dilution
For direct IV injection, use without further dilution.
If dose is >10 mg, dilute in 50 mL of a compatible IV solution.
For IV infusion, manufacturer recommends dilution in 50 mL of 5% dextrose, 0.9% sodium chloride, 5% dextrose and 0.45% sodium chloride, Ringer’s, or lactated Ringer’s injection.
Manufacturer states that 0.9% sodium chloride injection is preferred because metoclopramide hydrochloride is most stable in this solution.
Rate of Administration
Direct IV injection: Administer each 10 mg slowly over 1–2 minutes. Rapid IV injection may cause transient but intense feelings of anxiety and restlessness, followed by drowsiness.
IV infusion: Administer slowly over ≥15 minutes.
IM Administration
Inject without further dilution.
Dosage
Available as metoclopramide hydrochloride; dosage expressed in terms of metoclopramide.
Metoclopramide therapy, including all dosage forms and routes of administration, should not exceed 12 weeks’ duration because of risk of tardive dyskinesia with longer-term use.
Nasal spray delivers 15 mg of metoclopramide per 70-µL metered spray. Each bottle contains 9.8 mL of solution, which is sufficient for administration 4 times daily over a period of 4 weeks.
Pediatric Patients
Intubation of the Small Intestine
IV
Children <6 years of age: Usually, one 0.1-mg/kg dose given by direct IV injection.
Pediatric patients 6–14 years of age: Usually, one 2.5- to 5-mg dose given by direct IV injection.
Pediatric patients >14 years of age: Usually, one 10-mg dose given by direct IV injection.
Adults
Diabetic Gastroparesis
Oral
10 mg 4 times daily, given 30 minutes before meals and at bedtime. Maximum recommended dosage is 40 mg daily. Continue for 2–8 weeks, depending on response.
Intranasal
15 mg (one spray in one nostril) administered 30 minutes before meals and at bedtime. Continue for 2–8 weeks, depending on response.
IV, then Oral
If symptoms are severe or oral use is not feasible, 10 mg 4 times daily, given by direct IV injection 30 minutes before meals and at bedtime. Continued use for up to 10 days may be required until symptoms subside enough to allow oral administration; however, thoroughly assess the risks and benefits prior to continuing therapy.
IM, then Oral
If symptoms are severe or oral use is not feasible, 10 mg 4 times daily, given by IM injection 30 minutes before meals and at bedtime. Continued use for up to 10 days may be required until symptoms subside enough to allow oral administration; however, thoroughly assess the risks and benefits prior to continuing therapy.
Cancer Chemotherapy-induced Nausea and Vomiting
Oral
When used for breakthrough nausea and vomiting† in addition to prophylactic antiemetic therapy, metoclopramide dosages of 10–20 mg given every 6 hours as needed have been used.
IV
Manufacturer states that metoclopramide usually is given by IV infusion 30 minutes before administration of chemotherapy, and then repeated every 2 hours for 2 additional doses followed by every 3 hours for 3 additional doses. Manufacturer states that initial 2 doses should be 2 mg/kg if highly emetogenic chemotherapy used; for less emetogenic drugs or regimens, 1 mg/kg dose may be sufficient.
When used for breakthrough nausea and vomiting† in addition to prophylactic antiemetic therapy, IV metoclopramide dosages of 10–20 mg given every 6 hours as needed have been used.
Prevention of Postoperative Nausea and Vomiting
IM
Manufacturer states that usual dose is 10 mg administered near the end of the surgical procedure; 20 mg also may be used.
Intubation of the Small Intestine
IV
Usually, one 10-mg dose given by direct IV injection.
Radiographic Examination of the Upper GI Tract
IV
Usually, one 10-mg dose given by direct IV injection.
Gastroesophageal Reflux Disease
Oral
If continuous dosing is required, 10–15 mg 4 times daily, given 30 minutes before meals and at bedtime for 4–12 weeks; base treatment duration on endoscopic evaluation of response. Maximum recommended dosage is 60 mg daily.
For intermittent symptoms or symptoms at specific times of the day, one 20-mg dose before the provocative situation may be preferred to daily administration of multiple doses.
Special Populations
Hepatic Impairment
Diabetic Gastroparesis
Oral
Moderate or severe hepatic impairment (Child-Pugh class B or C): 5 mg 4 times daily, given 30 minutes before meals and at bedtime (maximum 20 mg daily).
Mild hepatic impairment (Child-Pugh class A): Patient may receive usual recommended dosage.
Intranasal
Moderate or severe hepatic impairment: Not recommended because dosage cannot be adjusted.
Mild hepatic impairment: Patient may receive usual recommended dosage.
Gastroesophageal Reflux Disease
Oral
Moderate or severe hepatic impairment: 5 mg 4 times daily, given 30 minutes before meals and at bedtime, or 10 mg 3 times daily (maximum 30 mg daily).
Mild hepatic impairment: Patient may receive usual recommended dosage.
Renal Impairment
In patients with Clcr <40 mL/minute, manufacturers of metoclopramide injection recommend an initial parenteral dosage of approximately 50% of the usual dosage. Subsequently, increase or decrease dosage according to response and tolerance.
Diabetic Gastroparesis
Oral
Moderate or severe renal impairment (Clcr <60 mL/minute): 5 mg 4 times daily, given 30 minutes before meals and at bedtime (maximum 20 mg daily).
End-stage renal disease, including hemodialysis or continuous ambulatory peritoneal dialysis (CAPD): 5 mg twice daily (maximum 10 mg daily).
Intranasal
Moderate or severe renal impairment (Clcr <60 mL/minute): Not recommended because dosage cannot be adjusted.
Mild renal impairment (Clcr ≥60 mL/minute): Patient may receive usual recommended dosage.
Gastroesophageal Reflux Disease
Oral
Moderate or severe renal impairment (Clcr ≤60 mL/minute): 5 mg 4 times daily, given 30 minutes before meals and at bedtime, or 10 mg 3 times daily (maximum 30 mg daily).
End-stage renal disease, including hemodialysis or CAPD: 5 mg 4 times daily, given 30 minutes before meals and at bedtime, or 10 mg twice daily (maximum 20 mg daily).
Geriatric Patients
Reduce initial dosage. Administer lowest effective dosage.
Diabetic Gastroparesis
Oral: Initially, 5 mg 4 times daily, given 30 minutes before meals and at bedtime. May titrate to 10 mg 4 times daily based on response and tolerability (maximum 40 mg daily).
Intranasal: Metoclopramide nasal spray not recommended as initial therapy in patients ≥65 years of age. May switch from an alternative metoclopramide preparation given at a stable dosage of 10 mg 4 times daily to the nasal formulation given at a dosage of 15 mg (one spray in one nostril) given 30 minutes before meals and at bedtime (maximum 4 times daily); continue for 2–8 weeks, depending on response.
Gastroesophageal Reflux Disease
Oral: Initially, 5 mg 4 times daily, given 30 minutes before meals and at bedtime. May titrate to 10–15 mg 4 times daily based on response and tolerability (maximum 60 mg daily).
Poor CYP2D6 Metabolizers
Metoclopramide elimination may be slower in poor CYP2D6 metabolizers than in intermediate, extensive, or ultra-rapid CYP2D6 metabolizers; poor metabolizers may be at increased risk of dystonic and other adverse reactions. Reduced dosage recommended.
IV or IM: Manufacturers make no specific dosage recommendations.
Diabetic Gastroparesis
Oral: 5 mg 4 times daily, given 30 minutes before meals and at bedtime (maximum 20 mg daily).
Intranasal: Metoclopramide nasal spray not recommended because dosage cannot be adjusted.
Gastroesophageal Reflux Disease
Oral: 5 mg 4 times daily, given 30 minutes before meals and at bedtime, or 10 mg 3 times daily (maximum 30 mg daily).
Cautions for Metoclopramide Hydrochloride
Contraindications
-
Concomitant use of other drugs likely to cause extrapyramidal reactions.
-
History of tardive dyskinesia or dystonic reaction to metoclopramide.
-
Mechanical obstruction or perforation or other situations in which stimulation of GI motility might be dangerous.
-
GI hemorrhage
-
Pheochromocytoma or other catecholamine-releasing paragangliomas (due to potential for hypertensive/pheochromocytoma crisis).
-
History of seizure disorders.
-
Known hypersensitivity to metoclopramide.
Warnings/Precautions
Warnings
Tardive Dyskinesia
May cause tardive dyskinesia, a potentially irreversible disorder manifested by involuntary movements of the tongue or face, and sometimes by involuntary movements of the trunk and/or extremities; movements may be choreoathetotic in appearance (see Boxed Warning). Risk of developing tardive dyskinesia is increased in geriatric patients, especially older women, and patients with diabetes mellitus. Risk of developing tardive dyskinesia and likelihood that it will become irreversible increase with duration of therapy and total cumulative dose. Tardive dyskinesia occurs in about 20% of patients receiving the drug for >12 weeks. Avoid treatment durations >12 weeks, including all dosage forms and routes of administration, and reduce dosage in geriatric patients. Metoclopramide nasal spray not recommended for initial therapy in geriatric patients. Avoid use in patients receiving other drugs that are likely to cause tardive dyskinesia (e.g., antipsychotic agents). Discontinue metoclopramide in patients who develop signs or symptoms of tardive dyskinesia. Tardive dyskinesia may remit, either partially or completely, in some patients within several weeks to months after discontinuance. Metoclopramide may suppress or partially suppress signs of tardive dyskinesia, thereby masking the underlying disease process; effect of this suppression on the long-term course of tardive dyskinesia is unknown. Do not use metoclopramide for symptomatic control of tardive dyskinesia.
Other Warnings and Precautions
Other Extrapyramidal Symptoms
In addition to tardive dyskinesia, potential for other extrapyramidal reactions (e.g., acute dystonic reactions, parkinsonian symptoms, akathisia), especially in pediatric patients and adults <30 years of age or when high doses (e.g., IV doses for prophylaxis of cancer chemotherapy-induced nausea and vomiting) are administered. Advise patients to seek immediate medical attention if such symptoms occur and to discontinue metoclopramide.
Avoid use in patients receiving other drugs that are likely to cause extrapyramidal reactions (e.g., antipsychotic agents).
Commonly manifested as acute dystonic reactions or akathisia; stridor and dyspnea (possibly due to laryngospasm) reported rarely.
Generally occur within 24–48 hours after starting therapy.
Give diphenhydramine hydrochloride 50 mg IM or benztropine 1–2 mg IM to reverse symptoms.
If akathisia resolves, may consider reinitiating metoclopramide at a lower dosage. Discontinue intranasal metoclopramide if symptoms of akathisia occur.
Parkinsonian symptoms (e.g., tremor, cogwheel rigidity, bradykinesia, mask-like facies) have occurred. More common during first 6 months of therapy but occur occasionally after longer periods. Symptoms generally subside within 2–3 months following drug discontinuance.
Some manufacturers state metoclopramide can be used cautiously in patients with Parkinson’s disease, while others recommend avoiding use in patients with parkinsonian syndrome and in patients receiving antiparkinsonian drugs due to the potential exacerbation of symptoms.
Neuroleptic Malignant Syndrome (NMS)
NMS, a potentially fatal symptom complex characterized by hyperpyrexia, muscular rigidity, altered mental status, and autonomic dysfunction, reported with dopamine antagonists. Other symptoms may include elevations in CPK, rhabdomyolysis, and acute renal failure. Evaluate patients with these symptoms immediately.
Has occurred following metoclopramide overdosage in patients receiving concomitant therapy with other drugs associated with NMS.
Avoid use in patients receiving other drugs associated with NMS (e.g., typical or atypical antipsychotic agents).
Important to determine whether untreated or inadequately treated extrapyramidal reactions and serious medical illness (e.g., pneumonia, systemic infection) may coexist. In differential diagnosis, consider the possibility of central anticholinergic toxicity, heat stroke, malignant hyperthermia, drug fever, serotonin syndrome, and primary CNS pathology.
Immediately discontinue metoclopramide and other drugs not considered essential, provide intensive symptomatic treatment, monitor patient, and treat any concomitant serious medical condition for which specific therapies are available.
Depression
Mild to severe depression (including suicidal ideation and suicide) has occurred in patients with or without history of depression who receive metoclopramide.
Some manufacturers recommend avoidance of metoclopramide in patients with a history of depression, while others state it can be given if expected benefits outweigh expected risks.
Hypertension
May increase BP; increase in circulating catecholamines reported in hypertensive patients. Avoid use in patients with hypertension and in those receiving MAO inhibitors.
Hypertensive crisis reported in patients with undiagnosed pheochromocytoma; discontinue metoclopramide in any patient who has a rapid increase in BP.
Fluid Retention
Possible transient increases in plasma aldosterone concentrations and sodium retention; closely monitor patients (e.g., those with hepatic impairment, CHF, or cirrhosis) at risk of developing fluid retention and volume overload.
Monitor patients with hepatic impairment for fluid retention and volume overload. Discontinue metoclopramide if fluid retention or volume overload occurs at any time during therapy.
Hyperprolactinemia
May cause elevations in prolactin levels that persist with long-term administration. Hyperprolactinemia may result in impaired gonadal steroidogenesis and inhibition of reproductive function in both females and males. Galactorrhea, gynecomastia, amenorrhea, and impotence reported.
Hyperprolactinemia may potentially stimulate prolactin-dependent breast cancer. However, some clinical and epidemiologic studies have not shown an association between dopamine D2-receptor antagonists and tumorigenesis in humans.
Effects on the Ability to Drive and Operate Machinery
Drowsiness may occur, particularly at higher dosages.
Performance of activities requiring mental alertness and physical coordination (e.g., operating machinery, driving a motor vehicle) may be impaired. Concomitant use of CNS depressants and drugs that cause extrapyramidal reactions may increase mental and/or physical impairment; avoid such concomitant use.
Phenylketonuria
Each 5- or 10-mg orally disintegrating tablet of metoclopramide contains aspartame, which is metabolized in the GI tract to provide 4.7 mg of phenylalanine per tablet.
Pressure on Suture Lines Following GI Anastomosis or Closure
When deciding whether to use parenteral metoclopramide or NG suction to prevent postoperative nausea and vomiting, consider the possibility that metoclopramide theoretically could produce increased pressure on suture lines following GI anastomosis or closure.
Specific Populations
Pregnancy
Published studies, including retrospective cohort studies, national registry studies, and meta-analyses, have not revealed an increased risk of adverse pregnancy-related outcomes with metoclopramide use during pregnancy.
No adverse developmental effects observed in animal studies.
Crosses the placenta and may cause extrapyramidal reactions and methemoglobinemia in neonates whose mothers received the drug during delivery; monitor for extrapyramidal effects.
Lactation
Distributed into milk. Estimated dose received by breast-fed infants is <10% of the maternal weight-adjusted oral dose. In one study, estimated dose from breast milk was 6–24 mcg/kg daily at 3–9 days postpartum and 1–13 mcg/kg daily at 8–12 weeks postpartum. Exposure expected to be similar following maternal doses of 10 mg administered orally or 15 mg administered intranasally.
Adverse GI effects (e.g., intestinal discomfort, increased intestinal gas formation) reported in breast-fed infants exposed to metoclopramide.
Although metoclopramide increases prolactin concentrations, data are inadequate to support drug-related effects on milk production.
Consider developmental and health benefits of breast-feeding along with the mother's clinical need for metoclopramide and any potential adverse effects on the breast-fed child from the drug or underlying maternal condition.
Monitor nursing neonates for extrapyramidal effects (dystonias) and methemoglobinemia.
Females and Males of Reproductive Potential
Animal reproductive studies using metoclopramide dosages of up to approximately 3 times the maximum recommended human dose (MRHD) have not revealed impaired fertility or altered reproductive performance. Menstrual disturbances and impotence have been reported with metoclopramide.
Pediatric Use
Safety profile in adults cannot be extrapolated to pediatric patients. Dystonias and other extrapyramidal reactions are more common in pediatric patients than in adults.
Safety and efficacy of oral and intranasal metoclopramide not established in pediatric patients; these formulations are not recommended for use in pediatric patients because of risk of tardive dyskinesia and other extrapyramidal reactions, as well as risk of methemoglobinemia in neonates.
Safety and efficacy of metoclopramide injection in pediatric patients is established only for use to facilitate intubation of the small intestine. Use metoclopramide injection with caution; incidence of extrapyramidal reactions is increased in pediatric patients.
Use metoclopramide injection with caution in neonates. Neonatal susceptibility to methemoglobinemia is increased due to prolonged clearance (may cause excessive serum concentrations) in combination with decreased neonatal levels of cytochrome-b5 reductase.
Geriatric Use
Geriatric patients are more likely to have decreased renal function and may be more sensitive to therapeutic or adverse effects of metoclopramide. Geriatric patients, especially older women, are at increased risk for tardive dyskinesia.
Risk of adverse parkinsonian effects increases with increasing dosage; administer lowest effective dosage in geriatric patients. If parkinsonian symptoms develop, generally should discontinue metoclopramide before initiating specific antiparkinsonian therapy.
Confusion and oversedation may occur.
Substantially eliminated by the kidneys; risk of adverse reactions, including tardive dyskinesia, may be greater in patients with impaired renal function.
Consider reduced dosage. Select dosage with caution, usually initiating therapy at the low end of the dosage range, because of age-related decreases in renal function and concomitant disease and drug therapy.
Hepatic Impairment
Clearance reduced by approximately 50% in patients with severe hepatic impairment (Child-Pugh class C), resulting in increased exposure. Possible increased risk of adverse effects. Pharmacokinetic data lacking in patients with moderate hepatic impairment (Child-Pugh class B). Reduced dosage recommended in patients with moderate to severe hepatic impairment. Avoid intranasal metoclopramide in patients with moderate to severe hepatic impairment.
Possible increased risk of fluid retention in patients with hepatic impairment. Monitor for fluid retention and volume overload in patients with hepatic impairment.
Renal Impairment
Systemic exposure increased approximately 2-fold in patients with moderate or severe renal impairment (Clcr <60 mL/minute) following oral administration. In patients with ESRD requiring dialysis, systemic exposure increased approximately 3.5-fold. Reduce dosages in patients with moderate to severe renal impairment, including those undergoing hemodialysis or continuous ambulatory peritoneal dialysis.
Avoid intranasal metoclopramide in patients with moderate to severe renal impairment, including those undergoing hemodialysis or peritoneal dialysis. Initial parenteral dosage reductions recommended in patients with Clcr<40 mL/minute; subsequently, increase or decrease dosage according to response and tolerance..
Common Adverse Effects
Oral metoclopramide (>10% of patients): Restlessness, drowsiness, fatigue, lassitude.
Parenteral metoclopramide: restlessness, sleepiness, tiredness, dizziness, exhaustion, headache, confusion, difficulty sleeping.
Intranasal metoclopramide (≥5% of patients): Dysgeusia, headache, and fatigue.
Drug Interactions
Metabolized by CYP2D6; also conjugated with glucuronic acid and sulfuric acid.
Orally Administered Drugs
Possible decreased absorption of certain drugs that disintegrate, dissolve, and/or are absorbed mainly in the stomach.
Possible enhanced rate and extent of absorption of drugs mainly absorbed in the small intestine.
Drugs that Impair GI Motility
Possible reduced oral absorption of metoclopramide; monitor for reduced metoclopramide efficacy.
Drugs Affecting Hepatic Microsomal Enzymes
Potent CYP2D6 inhibitors: Possible increased systemic exposure to metoclopramide and exacerbation of extrapyramidal symptoms. Reduce metoclopramide dosage (see Table 1). Examples of potent CYP2D6 inhibitors include, but are not limited to, bupropion, fluoxetine, paroxetine, and quinidine.
|
Metoclopramide Route of Administration |
Adult Dosage Recommendation |
|---|---|
|
Oral |
Diabetic gastroparesis: 5 mg given 4 times daily (maximum 20 mg daily) Gastroesophageal reflux: 5 mg given 4 times daily or 10 mg given 3 times daily (maximum 30 mg daily) |
|
Parenteral |
Manufacturers make no specific recommendations |
|
Intranasal |
Not recommended; dosage cannot be adjusted to reduce exposure |
Drugs Metabolized by Hepatic Microsomal Enzymes
CYP2D6 substrates: In vitro studies suggest metoclopramide can inhibit CYP2D6, but interactions considered unlikely in vivo at clinically relevant concentrations.
Drugs with Similar Adverse Effect Profiles
Drugs that are likely to cause extrapyramidal reactions or are known to cause tardive dyskinesia or neuroleptic malignant syndrome (NMS): Possible additive effects; avoid concomitant use.
Dopaminergic Agents
Possible reduced efficacy of metoclopramide and possible exacerbation of parkinsonian symptoms due to opposing effects on dopamine. Avoid concomitant use; if concomitant use is required, monitor therapeutic effects.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Acetaminophen |
Possible enhanced rate and extent of acetaminophen absorption |
|
|
Anticholinergic agents (e.g., atropine) |
Antagonism of GI motility effects of metoclopramide Impairment of GI motility by anticholinergic agent may reduce oral absorption of metoclopramide |
Monitor for reduced metoclopramide efficacy |
|
Antidiarrheal agents, antiperistaltic |
Impairment of GI motility by antiperistaltic agent may reduce oral absorption of metoclopramide |
Monitor for reduced metoclopramide efficacy |
|
Antipsychotic agents (e.g., butyrophenones, phenothiazines) |
Possible additive adverse effects, including increased frequency and severity of tardive dyskinesia, parkinsonian or other extrapyramidal symptoms, and NMS |
Avoid concomitant use |
|
Atovaquone |
Possible decreased atovaquone absorption |
Monitor for reduced atovaquone efficacy |
|
CNS depressants (alcohol, opiates or other analgesics, sedatives or hypnotics, anxiolytic agents, anesthetics) |
Increased CNS depressant effects; possible enhanced rate and extent of alcohol absorption |
Avoid concomitant use |
|
Cyclosporine |
Possible enhanced rate and extent of cyclosporine absorption |
Monitor cyclosporine concentrations and adjust cyclosporine dosage as needed |
|
Digoxin |
Possible decreased digoxin absorption |
Monitor digoxin concentrations and adjust digoxin dosage as needed |
|
Dopamine agonists (e.g., apomorphine, bromocriptine, cabergoline, pramipexole, ropinirole, rotigotine) |
Possible reduced efficacy of metoclopramide and possible exacerbation of parkinsonian symptoms due to opposing effects on dopamine |
Avoid concomitant use; if concomitant use required, monitor therapeutic effects |
|
Fluoxetine |
Increased peak concentration and AUC of metoclopramide by 40 and 90%, respectively; possible exacerbation of extrapyramidal symptoms |
Reduce metoclopramide dosage (see Table 1) |
|
Fosfomycin |
Possible decreased fosfomycin absorption |
Monitor for reduced fosfomycin efficacy |
|
Insulin |
Possible alteration of glycemic control secondary to metoclopramide-related changes in the delivery of food to and the rate of absorption in the intestine |
Monitor blood glucose; adjustment of insulin dose or timing may be necessary |
|
Levodopa |
Possible enhanced rate and extent of levodopa absorption Possible reduced efficacy of metoclopramide and possible exacerbation of parkinsonian symptoms due to opposing effects on dopamine |
Avoid concomitant use; if concomitant use required, monitor therapeutic effects |
|
MAO inhibitors |
Possible hypertensive reaction due to metoclopramide-induced release of catecholamines |
Avoid concomitant use |
|
Neuromuscular blocking agents |
Enhanced neuromuscular blockade due to metoclopramide inhibition of plasma cholinesterase |
Monitor for prolonged neuromuscular blockade |
|
Opiate analgesics |
Antagonism of GI motility effects of metoclopramide Impairment of GI motility by opiate may reduce oral absorption of metoclopramide |
Monitor for reduced metoclopramide efficacy |
|
Posaconazole |
Posaconazole oral suspension: Possible decreased posaconazole absorption Posaconazole delayed-release tablets: Absorption not affected |
Posaconazole oral suspension: Monitor for reduced posaconazole efficacy |
|
Sirolimus |
Possible enhanced sirolimus absorption |
Monitor sirolimus concentrations and adjust sirolimus dosage as needed |
|
Tacrolimus |
Possible enhanced tacrolimus absorption |
Monitor tacrolimus concentrations and adjust tacrolimus dosage as needed |
|
Tetracycline |
Possible enhanced rate and extent of tetracycline absorption |
Metoclopramide Hydrochloride Pharmacokinetics
Absorption
Bioavailability
Following oral administration, rapidly and almost completely absorbed. Relative to a 20 mg IV dose, absolute bioavailability of oral metoclopramide is about 80%. Peak plasma concentration usually attained at 1–2 hours.
Orally disintegrating tablets are bioequivalent to metoclopramide conventional tablets when administered under fasting conditions in adults. Time to peak plasma concentration is delayed from 1.8 to 3 hours and peak concentration is decreased by 17% when orally disintegrating tablets are administered with a high-fat meal compared to the fasted state, although overall absorption is not significantly affected. Clinical relevance of a lower peak plasma concentration is not known.
Following intranasal administration, absolute bioavailability is 47% compared with IV administration. Absorption is reduced following intranasal versus oral administration; peak concentration, AUC, and time to reach peak concentration are similar following a 15-mg intranasal dose or a 10-mg oral dose.
Over an intranasal dose range of 10–80 mg, systemic exposure is proportional to dose.
Onset
Following oral administration, 30–60 minutes for effects on GI tract.
Following IM administration, 10–15 minutes for effects on GI tract.
Following IV administration, 1–3 minutes for effects on GI tract.
Food
Administration of the orally disintegrating tablets immediately after a high-fat meal did not affect extent of absorption, but decreased peak blood concentration by 17% and increased time to peak concentration to 3 hours (compared with 1.8 hours under fasting conditions). Clinical importance of decreased peak concentration is unknown.
Special Populations
Moderate or severe renal impairment: AUC following oral administration is approximately 2-fold that observed in individuals with normal renal function; in end-stage renal disease requiring dialysis, AUC is approximately 3.5-fold that observed in individuals with normal renal function.
Females: AUC and peak concentration following intranasal administration are increased by 34 and 42%, respectively, compared with males. Clinical relevance unknown.
Body weight: Following intranasal administration, lower systemic exposure expected in individuals with higher lean body weight (within range of 34–94 kg). Clinical relevance unknown.
Pediatric patients: Pharmacodynamics are highly variable; relationship between drug plasma concentrations and pharmacodynamic effects not established.
Infants: Metoclopramide may accumulate in plasma after multiple doses; mean peak plasma concentration was 2-fold higher after tenth dose compared with that after first dose in infants (3.5 weeks–5.4 months of age) with gastroesophageal reflux receiving metoclopramide oral solution.
Distribution
Extent
Distributed into milk in humans.
Plasma Protein Binding
30% bound.
Elimination
Metabolism
Undergoes enzymatic metabolism via oxidation as well as conjugation with glucuronic acid and sulfuric acid in the liver. Monodeethylmetoclopramide, a major oxidative metabolite, is formed mainly by CYP2D6, which is subject to genetic variability.
Elimination Route
Excreted in urine (85%) within 72 hours following an oral dose; approximately 50% of dose excreted as free or conjugated metoclopramide. About 18 and 22% of a 10 mg and 20 mg oral dose, respectively, excreted in urine as unchanged drug within 36 hours.
Minimally removed by hemodialysis or peritoneal dialysis.
Half-life
In adults with normal renal function, 5–6 hours. Half-life of 8.1 hours reported following intranasal administration.
In pediatric patients, elimination half-life is about 4.1–4.5 hours.
Special Populations
Renal impairment: Half-life may be prolonged and clearance decreased.
Severe hepatic impairment (Child-Pugh class C): Average clearance following oral administration is reduced by approximately 50% compared with individuals with normal hepatic function.
Data insufficient to determine whether pharmacokinetics of the drug in pediatric patients are similar to those in adults.
Neonates: Reduced clearance, possibly associated with immature renal and hepatic functions present at birth.
Stability
Storage
Nasal
Solution
20–25°C (may be exposed to 15–30°C). Discard 4 weeks after opening.
Oral
Tablets
Tight, light-resistant containers at 20–25°C.
Tablets, Orally Disintegrating
20–25°C. Do not remove from blister pack until immediately before administration.
Solution
Tight, light-resistant containers at 20–25°C. Protect from freezing.
Parenteral
Injection
20–25°C. Protect from light.
Following dilution with 5% dextrose, 0.9% sodium chloride, 5% dextrose and 0.45% sodium chloride, Ringer’s, or lactated Ringer’s injection, store for up to 48 hours (without freezing) when protected from light or for up to 24 hours under normal light conditions (i.e., unprotected from light).
May be stored frozen for up to 4 weeks following dilution with 0.9% sodium chloride injection.
Degradation occurs if metoclopramide is diluted in 5% dextrose injection and frozen.
Actions
-
A dopamine D2-receptor antagonist, an antiemetic, and a stimulant of upper GI motility (prokinetic agent).
-
Mechanism of action in GI disorders not fully elucidated; principal effects involve the GI tract and CNS. Appears to sensitize tissue to the actions of acetylcholine, resulting in stimulation of the upper GI tract, without causing stimulation of gastric, biliary, or pancreatic secretions.
-
Increases gastric contraction tone and amplitude, relaxes the pyloric sphincter and duodenal bulb, and increases peristalsis of the duodenum and jejunum to accelerate gastric emptying and intestinal transit.
-
Antiemetic effects likely due to blockade of central and peripheral dopamine receptors, which decreases stimulation of the chemoreceptor trigger zone.
Advice to Patients
-
Provide the patient or caregiver with a copy of the manufacturer’s medication guide. Instruct patient or caregiver to read and understand the contents of the medication guide before initiating therapy and each time the prescription is refilled.
-
Inform patients that oral and intranasal formulations of metoclopramide are recommended for use in adults only.
-
Instruct patients receiving intranasal metoclopramide therapy on appropriate use of the metered-dose inhaler and provide them with a copy of the manufacturer's instructions for use.
-
Inform patients of the risk of tardive dyskinesia. Stress importance of contacting clinician immediately if new, abnormal, involuntary, or uncontrollable muscle movements occur (e.g., lip smacking, chewing, puckering mouth, frowning, scowling, tongue protrusion, blinking, eye movements, arm and leg shaking). Stress importance of not taking metoclopramide for >12 weeks.
-
Inform patients of the risk of neuroleptic malignant syndrome (NMS). Stress importance of contacting clinician immediately if signs or symptoms of NMS (e.g., high fever, stiff muscles, difficulty thinking, fast or uneven heartbeat, increased sweating) occur.
-
Inform patients of the risk of dystonic reactions, parkinsonian symptoms, or akathisia. Stress importance of contacting clinician immediately if such reactions occur.
-
Inform patients of the risk of depression and/or suicidality. Stress importance of contacting clinician immediately if depression or suicidality occurs.
-
Inform patients of the potential for drowsiness or dizziness.
-
Inform patients of the potential for metoclopramide to impair mental alertness or physical coordination; avoid driving or operating machinery until effects on the individual are known. Advise patients that alcohol, opiate analgesics, sedatives or hypnotics, anxiolytic agents, other CNS depressants, and other drugs that cause extrapyramidal symptoms may enhance such impairment.
-
For patients receiving metoclopramide nasal solution, stress importance of not repeating a dose if uncertain whether the spray entered the nostril and of not administering an extra dose or a double dose to make up for a missed dose; instead, administer the next dose at the regularly scheduled time.
-
Inform patients with phenylketonuria that metoclopramide orally disintegrating tablets contain aspartame.
-
Stress importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses. Advise patients that concomitant use of metoclopramide with many other drugs may precipitate or worsen tardive dyskinesia, extrapyramidal symptoms, NMS, and CNS depression. Explain that the prescriber of any other medication must be made aware that the patient is taking metoclopramide.
-
Stress importance of patients informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Inform patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Nasal |
Solution |
15 mg (of metoclopramide) per metered spray |
Gimoti |
Evoke |
|
Oral |
Solution |
5 mg (of metoclopramide) per 5 mL* |
Metoclopramide Hydrochloride Oral Solution |
|
|
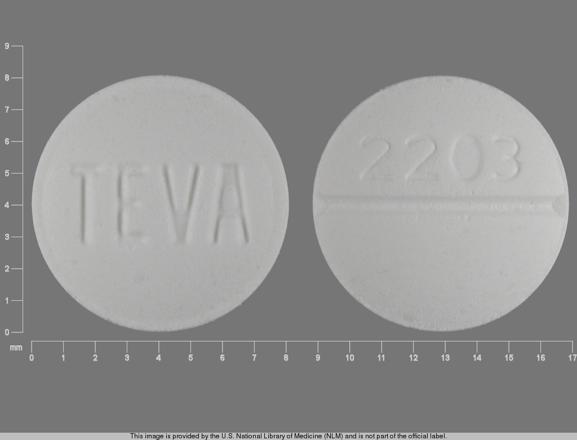
Tablets |
5 mg (of metoclopramide)* |
Metoclopramide Hydrochloride Tablets |
||
|
Reglan |
ANI |
|||
|
10 mg (of metoclopramide)* |
Metoclopramide Hydrochloride Tablets |
|||
|
Reglan (scored) |
ANI |
|||
|
Tablets, orally disintegrating |
5 mg (of metoclopramide)* |
Metoclopramide Hydrochloride Orally Disintegrating Tablets |
||
|
10 mg (of metoclopramide)* |
Metoclopramide Hydrochloride Orally Disintegrating Tablets |
|||
|
Parenteral |
Injection |
5 mg (of metoclopramide) per mL* |
Metoclopramide Hydrochloride Injection |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions February 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
More about metoclopramide
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (518)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Drug class: GI stimulants
- Breastfeeding
Patient resources
Professional resources
- Metoclopramide Injection prescribing information
- Metoclopramide Oral Solution (FDA)
- Metoclopramide Orally DisintegratingTablets (FDA)
- Metoclopramide Tablets (FDA)