Flecainide Acetate (Monograph)
Drug class: Class Ic Antiarrhythmics
Warning
- Mortality
-
In the Cardiac Arrhythmia Suppression Trial (CAST), excessive mortality and nonfatal cardiac arrest reported in patients with asymptomatic non-life-threatening ventricular arrhythmias (e.g., premature ventricular contractions [PVCs]) and recent MI (>6 days, but <2 years previously) who were receiving flecainide (5.1%) compared with placebo (2.3%).1 190 302 (See Mortality under Cautions.)
-
Although not known whether these findings can be extrapolated to other patient populations (e.g., patients without recent MI), it is prudent to consider the risks of class Ic antiarrhythmic agents in addition to the lack of evidence of improved survival generally unacceptable in patients without life-threatening ventricular arrhythmias, even in patients experiencing unpleasant, but non-life-threatening symptoms.1
- Proarrhythmic Effects in Patients with Atrial Fibrillation/Flutter
-
Do not use in patients with chronic atrial fibrillation because of risk of ventricular proarrhythmia (e.g., PVCs, VT, VF, death).1 (See Patients with Chronic Atrial Fibrillation under Cautions.)
-
Some patients with atrial flutter may develop 1:1 AV conduction.1 Paradoxically, an increase in ventricular rate also may occur in patients with atrial fibrillation; concomitant use of drugs with negative chronotropic effects (e.g., digoxin, β-adrenergic blocking agents) may reduce this risk.1
Introduction
Local anesthetic-type class Ic antiarrhythmic agent.1 3 4 5 6 7 146 147
Uses for Flecainide Acetate
Ventricular Arrhythmias
Suppression and prevention of recurrent ventricular arrhythmias (e.g., sustained VT) that, in the clinician’s judgment, are considered life-threatening.1 3 4 5 24 52 53 77 89 90 91 92 110 125 161 162 166 175 176 177 178 179 (See Boxed Warning.)
Because of arrhythmogenic potential and associated risk of death, use of flecainide for less severe arrhythmias (e.g., PVCs) not recommended.1 162 163 164 166 170 173 174 175 176 177 178 179 186 190 211 302
No evidence that use is associated with beneficial effect on mortality or sudden death.1 91 92 109 163 164 167 170 171
Supraventricular Tachyarrhythmias
Prevention of paroxysmal supraventricular tachycardia (PSVT), including AV nodal reentrant tachycardia and AV reentrant tachycardia (e.g., Wolff-Parkinson-White syndrome); other symptomatic, disabling, supraventricular tachycardias of unspecified mechanisms; and symptomatic, disabling paroxysmal atrial fibrillation/flutter (PAF) in patients without structural heart disease.1 35 110 115 140 192 193 194 197 198 199 200 201 206 300
One of several drugs that may be used for ongoing management of PSVT in patients without structural or ischemic heart disease; however, because of adverse effects, use generally reserved for patients in whom other therapies (e.g., catheter ablation, β-adrenergic blocking agents, diltiazem, verapamil) are ineffective or contraindicated.300
Considered a drug of choice for pharmacologic cardioversion of atrial fibrillation or flutter† [off-label].300 301
May be used for ongoing management of other supraventricular tachycardias (e.g., focal atrial tachycardia† [off-label], junctional tachycardia† [off-label]).113 120 149 300
Because of risk of proarrhythmia, do not use in patients with structural heart disease or ischemic heart disease.1 300
Flecainide Acetate Dosage and Administration
General
-
Monitor plasma flecainide concentrations when feasible; monitoring is required in patients with severe hepatic or renal impairment,1 and recommended in other patients in whom elimination of the drug may be impaired (e.g., those with moderate renal impairment or CHF, or receiving concomitant amiodarone).1 43 Maintain trough plasma flecainide concentrations at <0.7–1 mcg/mL since concentrations above this range associated with higher rate of adverse cardiac effects.1 59 70 78 104 (See Plasma Concentrations under Pharmacokinetics.)
-
Clinical and ECG monitoring of cardiac function is recommended during therapy.1 89
-
In patients with sustained VT, initiate therapy in hospital setting with ECG monitoring regardless of cardiac status.1 89 151 Some clinicians recommend that withdrawal of therapy also should occur in a hospital setting under continuous ECG monitoring.164 172 182
-
If used in pediatric patients, administer under direct supervision of experienced cardiologist.1 (See Pediatric Use under Cautions.)
Transferring from Other Antiarrhythmic Agents
-
A transition period is suggested in patients transferring from therapy with another antiarrhythmic agent to flecainide.1 Allow ≥2–4 half-lives of the previous antiarrhythmic to elapse prior to initiating flecainide.1
-
Consider hospitalization for transition if discontinuance of the current antiarrhythmic drug is likely to produce life-threatening arrhythmias.1
Administration
Oral Administration
Administer orally in 2 equally divided doses daily at 12-hour intervals.1
If arrhythmias are not adequately controlled or drug is not well tolerated with twice-daily dosing, may administer at 8-hour intervals.1 59 89 146 150
Extemporaneously Compounded Oral Solution
Extemporaneously compounded oral solutions of flecainide acetate have been prepared.247
Standardize 4 Safety
Standardized concentrations for an extemporaneously compounded oral solution of flecainide have been established through Standardize 4 Safety (S4S), a national patient safety initiative to reduce medication errors, especially during transitions of care.252 Because recommendations from the S4S panels may differ from the manufacturer’s prescribing information, caution is advised when using concentrations that differ from labeling, particularly when using rate information from the label.252 For additional information on S4S (including updates that may be available), see [Web].252
|
Concentration Standards |
|---|
|
10 mg/mL |
Dosage
Available as flecainide acetate; dosage expressed in terms of the salt.1
Adjust dosage carefully according to individual patient response and tolerance.1 3 89
To minimize effects on cardiac conduction, use lowest possible effective dosage.1 (See Effects on Cardiac Conduction under Cautions.)
Steady-state plasma concentrations and optimum therapeutic effect may not be attained for 3–5 days (or longer in some patients); do not increase dosage more frequently than once every 4 days.1 76
Oral loading doses generally not used since arrhythmogenicity and congestive heart failure may occur.1 However, single oral loading doses (e.g., 200–300 mg) have been used for conversion of recent-onset atrial fibrillation to normal sinus rhythm† [off-label] (“pill-in-the-pocket” approach) in individuals with mild or no structural heart disease.224 228 233 235 236 240 241 242 243 244 301
Pediatric Patients
Supraventricular and Ventricular Arrhythmias
Oral
Consult specialized references.1 (See Pediatric Use under Cautions.)
Infants <6 months of age: Initial dosage approximately 50 mg/m2 daily, divided into 2 or 3 equally spaced doses.1
Children ≥6 months of age: Initial dosage may be increased to 100 mg/m2 daily.1
Obtain plasma trough (<1 hour before dosing) flecainide concentrations and ECG at steady state (after at least 5 doses) after initiation of therapy or after any change in dosing.1 Plasma drug concentrations may be labile in patients receiving higher dosages.1 Small changes in dosage may lead to disproportionate increases in plasma drug concentrations.1
During first year of therapy, manufacturer suggests that a 12-lead ECG and plasma trough flecainide concentration be obtained whenever the patient is seen for clinical follow-up.1 Usual therapeutic concentration in children is 200–500 ng/mL, although concentrations up to 800 ng/mL may be required.1
Adults
Ventricular Arrhythmias
Oral
Sustained VT: Initially, 100 mg every 12 hours.1 May increase dosage in increments of 50 mg twice daily every 4 days until optimum response is obtained; maximum recommended dosage is 400 mg daily.1
Higher initial dosages and more rapid dosage increases associated with increased incidence of proarrhythmic events and congestive heart failure, particularly during first few days of therapy.1
Dosages >300 mg daily generally not required.1
Supraventricular Tachyarrhythmias
Oral
PSVT or PAF: Initially, 50 mg every 12 hours.1 192 193 200 May increase dosage in increments of 50 mg twice daily every 4 days until optimum response is obtained; maximum recommended dosage is 300 mg daily.1
Self-administration for Conversion of PAF† [off-label]
OralPatients ≥70 kg: 300 mg as a single oral loading dose 5 minutes after onset of palpitations.224 242
Patients <70 kg: 200 mg as a single oral loading dose 5 minutes after onset of palpitations.224 242
Remain in sitting or supine position until resolution of palpitations or for ≥4 hours after dose.224 242 Seek medical advice if palpitations do not resolve within 6–8 hours, if previously unexperienced symptoms (e.g., dyspnea, presyncope, syncope) occur, or if marked increase in heart rate occurs.224
Do not take more than one dose during a 24-hour period.224
Prescribing Limits
Pediatric Patients
Supraventricular and Ventricular Arrhythmias
Oral
Maximum 200 mg/m2 daily.1
Adults
Ventricular Arrhythmias
Oral
Maximum 400 mg daily.1
Supraventricular Tachyarrhythmias
Oral
Maximum 300 mg daily for treatment of paroxysmal supraventricular arrhythmias.1
Self-administration for Conversion of Paroxysmal Atrial Fibrillation†
OralMaximum 300 mg as single oral dose in 24-hour period for adults ≥70 kg.224 242 224
Maximum 200 mg as single oral dose in 24-hour period for adults <70 kg.224 242
Special Populations
Hepatic Impairment
Monitor plasma concentrations closely to guide dosage adjustments.1 3 (See Hepatic Impairment under Cautions.)
Increase dosage with caution and at intervals of >4 days.1
Renal Impairment
In patients with severe renal impairment (Clcr ≤35 mL/minute), initial dosage of 100 mg once daily or 50 mg twice daily recommended.1 (See Renal Impairment under Cautions.)
In patients with moderate renal impairment, initial dosage of 100 mg every 12 hours recommended.1
Monitor plasma concentrations closely to guide dosage adjustments.1
Increase dosage with caution and at intervals of >4 days; closely monitor for adverse cardiac effects or other toxicity.1
Cautions for Flecainide Acetate
Contraindications
-
Preexisting 2nd or 3rd degree AV block or bifascicular block (right bundle branch block associated with left hemiblock) unless pacemaker is in place.1
-
Cardiogenic shock.1
-
Known hypersensitivity to flecainide.1
Warnings/Precautions
Warnings
Mortality
Increased risk of mortality or nonfatal cardiac arrest reported in post-MI patients with non-life-threatening ventricular arrhythmias.1 161 163 174 175 176 177 181 182 190 191 302 (See Boxed Warning.)
Limit use of flecainide in patients with ventricular arrhythmias to those with life-threatening arrhythmias;1 161 163 170 176 177 178 181 use in patients with less severe ventricular arrhythmias, even when symptomatic, is not recommended.1 161 163 170 176 177 178
Do not use in patients with recent or prior MI.1 302
Patients with Chronic Atrial Fibrillation
Manufacturer states not adequately studied and not recommended in patients with chronic atrial fibrillation; possible VT or VF or paradoxical increase in ventricular rate.1 207 208 209 (See Boxed Warning.)
Arrhythmogenic Effects
Potential for new and/or more severe or potentially fatal arrhythmias (principally ventricular tachyarrhythmias but also increased PVCs or supraventricular arrhythmias).1 27 43 44 45 46 47 48 49 50 51 52 151 159 Risk appears to be related to dosage and underlying cardiac disease.1 27 151
Clinical and ECG evaluations are essential prior to and during therapy.1 89 Follow recommended dosage schedule closely.1 27 Monitor plasma drug concentrations and avoid concentrations >1 mcg/mL.1 27 If possible, avoid concomitant use of other antiarrhythmic agents.27 43 44 (See Antiarrhythmic Agents under Interactions.)
Heart Failure
Potential for new or worsened CHF, particularly in patients with cardiomyopathy, preexisting severe CHF (NYHA class III or IV), or ejection fraction <30%.1
If CHF or myocardial dysfunction develops, dosage reduction, discontinuance of therapy, or modification of other drug therapy (e.g., digoxin, diuretics) may be necessary.1
Use with caution in patients with a history of CHF or myocardial dysfunction,1 89 146 151 154 particularly those with advanced failure or dysfunction.19 27 62 63 89 91 146 Carefully monitor such patients; do not exceed recommended initial dosage.1 Monitor plasma flecainide concentrations and adjust dosage to maintain trough concentrations <0.7–1 mcg/mL.1
Effects on Cardiac Conduction
To minimize effects on cardiac conduction, use lowest possible effective dosage.1
Consider dosage reduction if PR interval increases to ≥300 ms,1 QRS duration increases to ≥180 ms,1 or QTc interval increases substantially.46 50 89
If 2nd or 3rd degree AV block or bifascicular block occurs, discontinue flecainide unless a temporary or implanted artificial ventricular pacemaker is in place to ensure adequate ventricular rate.1 89
Torsades de pointes-type arrhythmia reported rarely.1
Patients with Sinus Node Dysfunction
Potential for sinus bradycardia, pause, or arrest in patients with sick sinus syndrome (including bradycardia-tachycardia syndrome); use with extreme caution, if at all,136 in such patients.1 90 151
Changes in Endocardial Pacing Threshold
Potential for increased endocardial pacing threshold and suppression of ventricular escape rhythms.1 32 38 39
Use with caution in patients with permanent artificial pacemakers or temporary pacing electrodes;1 32 38 39 do not administer to patients with existing poor thresholds or nonprogrammable artificial pacemakers unless suitable pacing rescue is available.1
In patients with pacemakers, determine pacing threshold before and 1 week after initiating therapy and at regular intervals thereafter.1
Potassium Imbalance
Correct any preexisting potassium imbalance before initiating flecainide.1
Specific Populations
Pregnancy
Category C.1
Lactation
Distributed into milk.1
Pediatric Use
Safety and efficacy not established in randomized controlled studies.1 Limited data suggest that flecainide may be useful for management of refractory supraventricular tachycardias in pediatric patients.127 300
Possible proarrhythmic effects.1 Has been associated with cardiac arrest and sudden death in pediatric patients with structural heart disease.1 Because of these risks, flecainide generally not a preferred antiarrhythmic drug in pediatric patients.300
Use should be supervised directly by a cardiologist experienced in the treatment of arrhythmias in children.1 Initiate therapy in hospital setting equipped with ECG monitoring.1
Hepatic Impairment
Elimination may be markedly prolonged; use in patients with substantial hepatic impairment only if benefits clearly outweigh risks.1 Monitor plasma concentrations.1 3 (See Hepatic Impairment under Dosage and Administration.)
Renal Impairment
Elimination may be impaired; use with caution.1 70 Monitor plasma concentrations.1 (See Renal Impairment under Dosage and Administration.)
Common Adverse Effects
Dizziness,1 visual disturbances,1 3 4 5 30 58 59 76 77 78 94 95 96 97 98 101 102 103 104 124 150 dyspnea,1 headache,1 30 94 95 97 98 102 103 104 nausea,1 94 95 97 fatigue,1 124 palpitation,1 chest pain.1
Drug Interactions
Metabolized by CYP2D6.1
Antiarrhythmic Agents
Potential for increased risk of arrhythmogenic effects;27 43 91 126 additive, synergistic, or antagonistic cardiac effects; or additive adverse effects.108 112 131 136
Avoid concomitant use with other antiarrhythmic agents if possible;1 27 43 44 reserve such concomitant therapy for carefully selected patients with severe refractory arrhythmias.77 92 108 110 111 112 122 (See Transferring from Other Antiarrhythmic Agents under Dosage and Administration.)
Diuretics
No apparent interaction when used concomitantly with diuretics.1
Drugs Affecting Hepatic Microsomal Enzymes
CYP2D6 inhibitors: Possible increase in plasma flecainide concentrations, particularly in extensive metabolizers.1
Protein-bound Drugs
Pharmacokinetic interaction unlikely.1
Specific Drugs and Foods
|
Drug or Food |
Interaction |
Comments |
|---|---|---|
|
Acidifying agents (e.g., ammonium chloride) |
Urinary excretion of flecainide increased and elimination half-life decreased in presence of very acidic urine 80 85 |
Flecainide dosage adjustment may be necessary70 |
|
Alkalinizing agents (e.g., high-dose antacids, carbonic anhydrase inhibitors, sodium bicarbonate) |
Urinary excretion of flecainide decreased and elimination half-life increased in presence of very alkaline urine 80 85 |
Flecainide dosage adjustment may be necessary70 |
|
Amiodarone |
Increased plasma flecainide concentrations by twofold1 |
Reduce flecainide dosage by 30–50%1 131 142 156 157 and monitor patient closely;1 142 monitor plasma flecainide concentrations and adjust dosage as necessary1 142 |
|
Antacids |
||
|
β-adrenergic blocking agents (e.g., propranolol) |
Potential for additive negative inotropic effects;1 effects on PR interval were less than additive1 Increased plasma concentrations of flecainide and propranolol by 20 and 30%, respectively1 133 |
|
|
Carbamazepine |
Increased rate of flecainide elimination1 |
|
|
Cimetidine |
Possible reduction in nonrenal and renal clearance of flecainide135 Increased elimination half-life and plasma concentrations of flecainide by 10 and 30%, respectively1 |
Possible flecainide dosage reduction; further study needed135 |
|
Clozapine |
Possible increased plasma flecainide concentrations246 |
Use with caution and monitor closely, especially patients with extensive-metabolizer phenotype246 Adjust flecainide and/or clozapine dosage as necessary246 |
|
Digoxin |
Possible increased plasma digoxin concentrations1 132 133 134 |
|
|
Diltiazem |
Experience is too limited to recommend concomitant use1 |
|
|
Disopyramide |
Potential for negative inotropic effects1 |
Use concomitantly only if potential benefits outweigh risk1 |
|
Milk |
Possible reduction of flecainide absorption in infants1 |
Consider reducing flecainide dosage when milk is removed from infant’s diet1 |
|
Nifedipine |
Experience is too limited to recommend concomitant use1 |
|
|
Phenytoin |
Possible increased rate of flecainide elimination1 |
|
|
Phenobarbital |
Possible increased rate of flecainide elimination1 |
|
|
Quinidine |
Possible increased plasma flecainide concentrations1 |
|
|
Verapamil |
Potential for additive negative inotropic effects1 |
Use concomitantly only if potential benefits outweigh risk1 |
Flecainide Acetate Pharmacokinetics
Absorption
Bioavailability
Rapidly and almost completely absorbed following oral administration,1 70 71 72 73 with peak plasma concentrations generally reached within approximately 3 hours (range: 1–6 hours).1 56 70 71 72 73 Absolute bioavailability is approximately 85–90%.70
No substantial first-pass metabolism.1 70 71
Food
Food may slightly decrease rate70 but does not affect extent of absorption.1 70 72
Milk may inhibit absorption in infants.1
Plasma Concentrations
Trough plasma concentrations are 0.2–1 mcg/mL in most patients successfully treated with flecainide.1 59 77 92 189
In children, usual therapeutic concentration is 0.2–0.5 mcg/mL, although concentrations up to 0.8 mcg/mL may be required.1
Increased risk of adverse cardiac effects (e.g., conduction defects, bradycardia) at plasma concentrations >0.7–1 mcg/mL, particularly when concentrations >1 mcg/mL.1 27 45 50 78
Distribution
Extent
Distributed into milk.1
Plasma Protein Binding
Elimination
Metabolism
Extensively metabolized, probably in the liver, to 2 major metabolites and at least 3 unidentified minor metabolites;1 70 73 unlikely that major metabolites contribute substantially to therapeutic or toxic effects.70 86
CYP2D6 involved in metabolism.1
Elimination Route
Excreted almost completely in urine; only small amounts of drug and/or metabolites excreted in feces.1 70 73
Plasma clearance is decreased when urine pH ≥8.1
Half-life
Biphasic; elimination half-life is about 11.5–16 hours following single or multiple doses in healthy adults.56 70 72 80 Elimination half-life following multiple doses in patients with PVCs slightly longer, averaging 19–22 hours (range: 12–30 hours).1 30 58 59 75 76
Special Populations
In patients with PVCs,1 30 58 59 70 75 76 CHF,1 56 70 or renal1 70 or hepatic impairment, elimination half-life is prolonged.1
In children, elimination half-life tends to decrease with age (around 29 hours at birth, 11–12 hours by 3 months of age, 6–8 hours by 1–12 years of age, and 11–12 hours by 12–15 years of age).1
Stability
Storage
Oral
Tablets
Tight, light-resistant containers at 20–25°C.1
Actions
-
Membrane-stabilizing antiarrhythmic agent; exhibits local anesthetic effects.1 3 4 5 6 12 13 14
-
Principal effect on cardiac tissue appears to be concentration-dependent inhibition of transmembrane influx of extracellular sodium ions via fast sodium channels.6 11 12 13 14 15 16 17
-
Combines with fast sodium channels within the myocardium and inhibits rapid sodium influx, which decreases the maximal rate of depolarization of phase 0 of the action potential.6 11 12 13 14 15 16 17
-
Combines with fast sodium channels in their inactive state12 13 17 and inhibits recovery after repolarization in a time- and voltage-dependent manner, which is associated with subsequent dissociation of the drug from the sodium channels.12 13 17
-
Exhibits electrophysiologic effects characteristic of class Ic antiarrhythmic agents, which slowly attach to and dissociate from transmembrane sodium channels.1 3 4 5 12 13 14 20
-
Produces dose-related decrease in intracardiac conduction throughout the heart, with the most marked effect on conduction within the His-Purkinje system.1 3 4 5 22 24
-
Produces dose-related increases in PR, QRS, and, to a lesser degree, QT intervals.1 3 22 23 24 25 27 30 52 53 58 59 76 89 94 102 104
-
May increase atrial effective refractory period (ERP) 22 23 24 26 31 36 77 145 and ventricular ERP.23 24 25 36 52 53 77 92
-
Exhibits a mild to moderate negative inotropic effect.1 10 18 19 60 61 62 63 64 65 66 67 68
Advice to Patients
-
Importance of not altering therapy without first consulting clinician.162 164 172
-
Advise patients who self-administer loading dose for conversion of paroxysmal atrial fibrillation to remain in a supine or sitting position until resolution of palpitations or for a period of at least 4 hours following the dose.224 242 Importance of informing clinician if palpitations do not resolve within 6–8 hours, previously unexperienced symptoms (e.g., dyspnea, presyncope, syncope) occur, or a marked increase in heart rate develops.224
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.1
-
Importance of women informing clinicians if they are or plan to become pregnant or to breast-feed.1
-
Importance of advising patients of other important precautionary information.1 (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
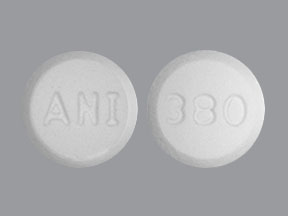
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
50 mg* |
Flecainide Acetate Tablets |
|
|
100 mg* |
Flecainide Acetate Tablets |
|||
|
150 mg* |
Flecainide Acetate Tablets |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
1. West-Ward Pharmaceuticals. Flecainide acetate tablets prescribing information. Eatontown, NJ; 2016 Mar.
3. Holmes B, Heel RC. Flecainide: a preliminary review of its pharmacodynamic properties and therapeutic efficacy. Drugs. 1985; 29:1-33. https://pubmed.ncbi.nlm.nih.gov/3882390
4. Nappi JM, Anderson JL. Flecainide: a new prototype antiarrhythmic agent. Pharmacotherapy. 1985; 5:209-21. https://pubmed.ncbi.nlm.nih.gov/3898035
5. Smith GH. Flecainide: a new class Ic antidysrhythmic. Drug Intell Clin Pharm. 1985; 19:703-7. https://pubmed.ncbi.nlm.nih.gov/3902429
6. Cowan JC, Vaughan Williams EM. Characterization of a new oral antiarrhythmic drug, flecainide (R818). Eur J Pharmacol. 1981; 73:333-42.
7. Hudak JM, Banitt EH, Schmid JR. Discovery and development of flecainide. Am J Cardiol. 1984; 53:17-20B.
8. Banitt EH, Coyne WE, Schmid JR et al. Antiarrhythmics. N-(aminoalkylene) trifluoroethoxybenzamides and N-(aminoalkylene) trifluoroethoxynaphthamides. J Med Chem. 1975; 18:1130-4. https://pubmed.ncbi.nlm.nih.gov/1177259
9. Banitt EH, Bronn WR, Coyne WE et al. Antiarrhythmics. 2. Synthesis and antiarrhythmic activity of N-(piperidylalkyl) trifluoroethoxybenzamides. J Med Chem. 1977; 20:821-6. https://pubmed.ncbi.nlm.nih.gov/874956
10. Verdouw PD, Deckers JW, Gordon JC. Antiarrhythmic and hemodynamic actions of flecainide acetate (R-818) in the ischemic porcine heart. J Cardiovasc Pharmacol. 1979; 1:473-86. https://pubmed.ncbi.nlm.nih.gov/94625
11. Kvam DC, Banitt EH, Schmid JR. Antiarrhythmic and electrophysiologic actions of flecainide in animal models. Am J Cardiol. 1984; 53:22-5B.
12. Vaughan Williams EM. A classification of antiarrhythmic actions reassessed after a decade of new drugs. J Clin Pharmacol. 1984; 24:129-47. https://pubmed.ncbi.nlm.nih.gov/6144698
13. Harrison DC. Antiarrhythmic drug classification: new science and practical applications. Am J Cardiol. 1985; 56:185-7. https://pubmed.ncbi.nlm.nih.gov/2409789
14. Harrison DC. Current classification of antiarrhythmic drugs as a guide to their rational clinical use. Drugs. 1986; 31:93-5. https://pubmed.ncbi.nlm.nih.gov/3948737
15. Singh BN, Nademanee K, Josephson MA et al. The electrophysiology and pharmacology of verapamil, flecainide, and amiodarone: correlations with clinical effects and antiarrhythmic actions. Ann NY Acad Sci. 1984; 432:210-35. https://pubmed.ncbi.nlm.nih.gov/6395762
16. Borchard U, Boisten M. Effect of flecainide on action potentials and alternating current-induced arrhythmias in mammalian myocardium. J Cardiovasc Pharmacol. 1982; 4:205-12. https://pubmed.ncbi.nlm.nih.gov/6175802
17. Campbell TJ. Kinetics of onset of rate-dependent effects of class I antiarrhythmic drugs are important in determining their effects on refractoriness in guinea-pig ventricle, and provide a theoretical basis for their subclassification. Cardiovasc Res. 1983; 17:344-52. https://pubmed.ncbi.nlm.nih.gov/6883410
18. Schulze JJ, Knops J. Effects of flecainide on contractile force and electrophysiological parameters in cardiac muscle. Arzneimittelforschung. 1982; 32:1025-9. https://pubmed.ncbi.nlm.nih.gov/6890819
19. Josephson MA, Ikeda N, Singh BN. Effects of flecainide on ventricular function: clinical and experimental correlations. Am J Cardiol. 1984; 53:95-100B.
20. Milne JR, Hellestrand KJ, Bexton RS et al. Class 1 antiarrhythmic agents—characteristic electrocardiographic differences when assessed by atrial and ventricular pacing. Eur Heart J. 1984; 5:99-107. https://pubmed.ncbi.nlm.nih.gov/6723689
21. Ikeda N, Singh BN, Davis LD et al. Effects of flecainide on the electrophysiologic properties of isolated canine and rabbit myocardial fibers. J Am Coll Cardiol. 1985; 5(2 Part 1):303-10. https://pubmed.ncbi.nlm.nih.gov/3968315
22. Estes NAM III, Garan H, Ruskin JN. Electrophysiologic properties of flecainide acetate. Am J Cardiol. 1984; 53:26-9B.
23. Hellestrand KJ, Bexton RS, Nathan AW et al. Acute electrophysiological effects of flecainide acetate on cardiac conduction and refractoriness in man. Br Heart J. 1982; 48:140-8. https://pubmed.ncbi.nlm.nih.gov/7093083
24. Anderson JL, Lutz JR, Allison SB. Electrophysiologic and antiarrhythmic effects of oral flecainide in patients with inducible ventricular tachycardia. J Am Coll Cardiol. 1983; 2:105-14. https://pubmed.ncbi.nlm.nih.gov/6853905
25. Olsson SB, Edvardsson N. Clinical electrophysiologic study of antiarrhythmic properties of flecainide: acute intraventricular delayed conduction and prolonged repolarization in regular paced and premature beats using intracardiac monophasic action potentials with programmed stimulation. Am Heart J. 1981; 102:864-71. https://pubmed.ncbi.nlm.nih.gov/7304394
26. Seipel L, Abendroth RR, Breithardt G. Electrophysiological effects of flecainide (R818) in man. Circulation. 1981; 62(4 Part II):III-153.
27. Morganroth J, Horowitz LN. Flecainide: its proarrhythmic effect and expected changes on the surface electrocardiogram. Am J Cardiol. 1984; 53:89-94B.
28. Abitbol H, Califano JE, Abate C et al. Use of flecainide acetate in the treatment of premature ventricular contractions. Am Heart J. 1983; 105:227-30. https://pubmed.ncbi.nlm.nih.gov/6823803
29. Somani P. Antiarrhythmic effects of flecainide. Clin Pharmacol Ther. 1980; 27:464-70. https://pubmed.ncbi.nlm.nih.gov/7357804
30. Anderson JL, Stewart JR, Perry BA et al. Oral flecainide acetate for the treatment of ventricular arrhythmias. N Engl J Med. 1981; 305:473-7. https://pubmed.ncbi.nlm.nih.gov/7019711
31. Vik-Mo H, Ohm OJ, Lund-Johansen P. Electrophysiologic effects of flecainide acetate in patients with sinus nodal dysfunction. Am J Cardiol. 1982; 50:1090-4. https://pubmed.ncbi.nlm.nih.gov/7137036
32. Hellestrand KJ, Nathan AW, Bexton RS et al. Electrophysiologic effects of flecainide acetate on sinus node function, anomalous atrioventricular connections, and pacemaker thresholds. Am J Cardiol. 1984; 53:30-8B.
33. Hellestrand KJ, Nathan AW, Bexton RS et al. Response of an abnormal sinus node to intravenous flecainide acetate. PACE. 1984; 7(3 Part 1):436-9. https://pubmed.ncbi.nlm.nih.gov/6204297
34. Hellestrand KJ, Nathan AW, Bexton RS et al. Cardiac electrophysiologic effects of flecainide acetate for paroxysmal reentrant junctional tachycardias. Am J Cardiol. 1983; 51:770-6. https://pubmed.ncbi.nlm.nih.gov/6829436
35. Neuss H, Buss J, Schlepper M et al. Effects of flecainide on electrophysiological properties of accessory pathways in the Wolff-Parkinson-White syndrome. Eur Heart J. 1983; 4:347-53. https://pubmed.ncbi.nlm.nih.gov/6617681
36. Bexton RS, Hellestrand KJ, Nathan AW et al. A comparison of the antiarrhythmic effects on AV junctional re-entrant tachycardia of oral and intravenous flecainide acetate. Eur Heart J. 1983; 4:92-102. https://pubmed.ncbi.nlm.nih.gov/6852073
37. Bexton RS, Hellestrand KJ, Nathan AW et al. Retrograde gap in fast pathway conduction accentuated by the class I antiarrhythmic agent, flecainide. PACE. 1983; 6:1273-7. https://pubmed.ncbi.nlm.nih.gov/6196737
38. Hellestrand KJ, Burnett PJ, Milne JR et al. Effect of the antiarrhythmic agent flecainide acetate on acute and chronic pacing thresholds. PACE. 1983; 6(5 Part 1):892-9. https://pubmed.ncbi.nlm.nih.gov/6195608
39. Walker PR, Papouchado M, James MA et al. Pacing failure due to flecainide acetate. PACE. 1985; 8:900-2. https://pubmed.ncbi.nlm.nih.gov/2415944
40. Velebit V, Podrid P, Lown B et al. Aggravation and provocation of ventricular arrhythmias by antiarrhythmic drugs. Circulation. 1982; 65:886-94. https://pubmed.ncbi.nlm.nih.gov/6176355
41. Torres V, Flowers D, Somberg JC. The arrhythmogenicity of antiarrhythmic agents. Am Heart J. 1985; 109(5 Part 1):1090-7. https://pubmed.ncbi.nlm.nih.gov/3993517
42. Rae AP, Greenspan AM, Spielman SR et al. Antiarrhythmic drug efficacy for ventricular tachyarrhythmias associated with coronary artery disease as assessed by electrophysiologic studies. Am J Cardiol. 1985; 55:1494-9. https://pubmed.ncbi.nlm.nih.gov/3890509
43. Nathan AW, Hellestrand KJ, Bexton RS et al. Proarrhythmic effects of the new antiarrhythmic agent flecainide acetate. Am Heart J. 1984; 107:222-8. https://pubmed.ncbi.nlm.nih.gov/6695656
44. Nathan AW, Hellestrand KJ, Bexton RS et al. The proarrhythmic effects of flecainide. Drugs. 1985; 29(Suppl 4):45-53. https://pubmed.ncbi.nlm.nih.gov/4006779
45. Spivack C, Gottlieb S, Miura DS et al. Flecainide toxicity. Am J Cardiol. 1984; 53:329-30. https://pubmed.ncbi.nlm.nih.gov/6695731
46. Wehr M, Noll B, Krappe J. Flecainide-induced aggravation of ventricular arrhythmias. Am J Cardiol. 1985; 55:1643-4. https://pubmed.ncbi.nlm.nih.gov/4003313
47. Sellers TD, DiMarco JP. Sinusoidal ventricular tachycardia associated with flecainide acetate. Chest. 1984; 85:647-9. https://pubmed.ncbi.nlm.nih.gov/6201323
48. Hohnloser S, Zeiher A, Hust MH et al. Flecainide-induced aggravation of ventricular tachycardia. Clin Cardiol. 1983; 6:130-5. https://pubmed.ncbi.nlm.nih.gov/6851274
49. Muhiddin K, Nathan AW, Hellestrand KJ et al. Ventricular tachycardia associated with flecainide. Lancet. 1982; 2:1220-1. https://pubmed.ncbi.nlm.nih.gov/6128526
50. Lui HK, Lee G, Dietrich P et al. Flecainide-induced QT prolongation and ventricular tachycardia. Am Heart J. 1982; 103(4 Part 1):567-9. https://pubmed.ncbi.nlm.nih.gov/7064795
51. Podrid PJ. Aggravation of ventricular arrhythmia: a drug-induced complication. Drugs. 1985; 29(Suppl 4):33-44. https://pubmed.ncbi.nlm.nih.gov/3924550
52. Platia EV, Estes NAM, Heine DL et al. Flecainide: electrophysiologic and antiarrhythmic properties in refractory ventricular tachycardia. Am J Cardiol. 1985; 55:956-62. https://pubmed.ncbi.nlm.nih.gov/3984883
53. Oetgen WJ, Tibbits PA, Abt MEO et al. Clinical and electrophysiologic assessment of oral flecainide acetate for recurrent ventricular tachycardia: evidence for exacerbation of electrical instability. Am J Cardiol. 1983; 52:746-50. https://pubmed.ncbi.nlm.nih.gov/6624666
54. Hodges M, Hoback J, Graham E et al. Cardiac function after oral dosing with flecainide acetate. Clin Pharmacol Ther. 1981; 29:251.
55. Tanenbaum R, Wilen M, Franciosa JA. Effects of flecainide on hemodynamics and functional capacity in heart failure. Circulation. 1982; 66(4 Part II):II-68.
56. Franciosa JA, Wilen M, Weeks CE et al. Pharmacokinetics and hemodynamic effects of flecainide in patients with chronic low output heart failure. J Am Coll Cardiol. 1983; 1:699.
57. Lui HK, Lee G, Stobbe D et al. Effect of flecainide on left ventricular function. Clin Res. 1983; 31:13A.
58. Hodges M, Haugland JM, Granrud G et al. Suppression of ventricular ectopic depolarizations by flecainide acetate, a new antiarrhythmic agent. Circulation. 1982; 65:879-85. https://pubmed.ncbi.nlm.nih.gov/7074749
59. Duff HJ, Roden DM, Maffucci RJ et al. Suppression of resistant ventricular arrhythmias by twice daily dosing with flecainide. Am J Cardiol. 1981; 48:1133-40. https://pubmed.ncbi.nlm.nih.gov/7304461
60. Muhiddin KA, Shaw E, Blackett A et al. The effect of a new antiarrhythmic agent, flecainide acetate, on systolic time intervals. Eur J Clin Pharmacol. 1983; 25:13-8. https://pubmed.ncbi.nlm.nih.gov/6617715
61. Muhiddin KA, Turner P, Blackett A. Effect of flecainide on cardiac output. Clin Pharmacol Ther. 1985; 37:260-3. https://pubmed.ncbi.nlm.nih.gov/3971650
62. Legrand V, Vandormael M, Collignon P et al. Hemodynamic effects of a new antiarrhythmic agent flecainide (R-818), in coronary heart disease. Am J Cardiol. 1983; 51:422-6. https://pubmed.ncbi.nlm.nih.gov/6823856
63. Josephson MA, Kaul S, Hopkins J et al. Hemodynamic effects on intravenous flecainide relative to the level of ventricular function in patients with coronary artery disease. Am Heart J. 1985; 109:41-5. https://pubmed.ncbi.nlm.nih.gov/3966331
64. Serruys PW, Vanhaleweyk G, Van den Brand M et al. The haemodynamic effect of intravenous flecainide acetate in patients with coronary artery disease. Br J Clin Pharmacol. 1983; 16:51-9. https://pubmed.ncbi.nlm.nih.gov/6882622
65. Legrand V, Materne P, Vandormael M et al. Comparative haemodynamic effects of intravenous flecainide in patients with and without heart failure and with and without beta-blocker therapy. Eur Heart J. 1985; 6:664-71. https://pubmed.ncbi.nlm.nih.gov/4054136
66. Jackson N, Verma SP, Frais MA et al. Hemodynamic dose-response effects of flecainide in acute myocardial infarction with and without left ventricular decompensation. Clin Pharmacol Ther. 1985; 37:619-24. https://pubmed.ncbi.nlm.nih.gov/3891187
67. Cohen AA, Daru V, Covelli G et al. Hemodynamic effects of intravenous flecainide in acute noncomplicated myocardial infarction. Am Heart J. 1985; 110:1193-6. https://pubmed.ncbi.nlm.nih.gov/4072876
68. Dunselman PHJM, Kingma JH, van Wijk LM et al. Haemodynamic and antiarrhythmic effects of intravenous flecainide acetate in chronic congestive heart failure. Drugs. 1985; 29(Suppl 4):58-64. https://pubmed.ncbi.nlm.nih.gov/4006780
69. von Philipsborn G, Gries J, Hofmann HP et al. Pharmacological studies on propafenone and its main metabolite 5-hydroxypropafenone. Arzneimittelforschung. 1984; 34:1489-97. https://pubmed.ncbi.nlm.nih.gov/6543124
70. Conard GJ, Ober RE. Metabolism of flecainide. Am J Cardiol. 1984; 53:41-51B.
71. Conard GJ, Carlson GL, Frost JW et al. Human plasma pharmacokinetics of flecainide acetate (R-818), a new antiarrhythmic, following oral and intravenous doses. Clin Pharmacol Ther. 1979; 25:218.
72. Tjandramaga TB, Verbesselt R, Van Hecken A et al. I.V. and oral-flecainide kinetics: absolute bio-availability, effects of food, antacid (aluminum hydroxide) and multiple oral doses. Eur Heart J. 1984; 5(Suppl B):135. https://pubmed.ncbi.nlm.nih.gov/6373273
73. McQuinn RL, Quarfoth GJ, Johnson JD et al. Biotransformation and elimination of14C-flecainide acetate in humans. Drug Metab Dispos. 1984; 12:414-20. https://pubmed.ncbi.nlm.nih.gov/6148206
74. Chang SF, Welscher TM, Miller AM et al. High-performance liquid chromatographic method for the quantitation of a meta-O-dealkylated metabolite of flecainide acetate, a new antiarrhythmic. J Chromatogr. 1985; 343:119-27. https://pubmed.ncbi.nlm.nih.gov/4066846
75. Conard GJ, Cronheim GE, Klempt HW. Relationship between plasma concentrations and suppression of ventricular extrasystoles by flecainide acetate (R-818), a new antiarrhythmic, in patients. Arzneimittelforschung. 1982; 32:155-9. https://pubmed.ncbi.nlm.nih.gov/7199921
76. Woosley RL, Siddoway LA, Duff HJ et al. Flecainide dose-response relations in stable ventricular arrhythmias. Am J Cardiol. 1984; 53:59-65B.
77. Anderson JL. Experience with electrophysiologically guided therapy of ventricular tachycardia with flecainide: summary of long-term follow-up. Am J Cardiol. 1984; 53:79-86B.
78. Salerno DM, Granrud G, Sharkey P et al. Pharmacodynamics and side effects of flecainide acetate. Clin Pharmacol Ther. 1986; 40:101-7. https://pubmed.ncbi.nlm.nih.gov/3720173
79. Conard GJ, Carlson GL, Frost JW et al. Plasma concentrations of flecainide acetate, a new antiarrhythmic agent, in humans. Clin Ther. 1984; 6:643-52. https://pubmed.ncbi.nlm.nih.gov/6478470
80. Johnston A, Warrington S, Turner P. Flecainide pharmacokinetics in healthy volunteers: the influence of urinary pH. Br J Clin Pharmacol. 1985; 20:333-8. https://pubmed.ncbi.nlm.nih.gov/4074602
81. Johnston A, Muhiddin KA, Hamer J. Serum protein binding of flecainide. Br J Clin Pharmacol. 1982; 13:606P.
82. Johnston A, Caplin JL, Hamer J et al. The serum protein binding of disopyramide and flecainide following acute myocardial infarction. Br J Clin Pharmacol. 1983; 15:601P.
83. Caplin JL, Johnston A, Hamer J et al. The acute changes in serum binding of disopyramide and flecainide after myocardial infarction. Eur J Clin Pharmacol. 1985; 28:253-5. https://pubmed.ncbi.nlm.nih.gov/4007029
84. Wang T, Siddoway LA, Bergstrand RH et al. Treatment of ventricular arrhythmia with individualized intravenous flecainide dosing regimens. Circulation. 1983; 68(4 Part II):III-416.
85. Muhiddin KA, Johnston A, Turner P. The influence of urinary pH on flecainide excretion and its serum pharmacokinetics. Br J Clin Pharmacol. 1984; 17:447-51. https://pubmed.ncbi.nlm.nih.gov/6326790
86. Guehler J, Gornick CC, Tobler HG et al. Electrophysiologic effects of flecainide acetate and its major metabolites in the canine heart. Am J Cardiol. 1985; 55:807-12. https://pubmed.ncbi.nlm.nih.gov/3919554
87. Mottonen LR, Holtzman JL, Harrison LI et al. Effects of smoking on the clearance of flecainide acetate. Clin Pharmacol Ther. 1984; 35:260.
88. Fach WA, Mai BV, Preusler W et al. Flecainid-intoxikation. (German; with English abstract; translation provided by Riker Laboratories.) Inn Med Aktuel. 1984; 11:27-31.
89. Anderson JL, Stewart JR, Crevey BJ. A proposal for the clinical use of flecainide. Am J Cardiol. 1984; 53:112-9B.
90. Flowers D, O’Gallagher D, Torres V et al. Flecainide: long-term treatment using a reduced dosing schedule. Am J Cardiol. 1985; 55:79-83. https://pubmed.ncbi.nlm.nih.gov/3966401
91. Reid PR, Griffith LSC, Platia EV et al. Evaluation of flecainide acetate in the management of patients at high risk of sudden cardiac death. Am J Cardiol. 1984; 53:108-11B.
92. Lal R, Chapman PD, Naccarrelli GV et al. Short- and long-term experience with flecainide acetate in the management of refractory life-threatening ventricular arrhythmias. J Am Coll Cardiol. 1985; 6:772-9. https://pubmed.ncbi.nlm.nih.gov/3928725
93. Granrud G, Salerno D, Hodges M et al. Long term flecainide is effective and well tolerated. Circulation. 1982; 66(4 Part II):II-69. https://pubmed.ncbi.nlm.nih.gov/7116593
94. Duran D, Platia EV, Griffith LSC et al. Suppression of complex ventricular arrhythmias by oral flecainide. Clin Pharmacol Ther. 1982; 32:554-61. https://pubmed.ncbi.nlm.nih.gov/7127996
95. Vanhaleweyk G, Balakumaran K, Lubsen J et al. Oral flecainide for suppression of ventricular arrhythmias. Cardiology. 1984; 71:30-9. https://pubmed.ncbi.nlm.nih.gov/6722846
96. Muhiddin KA, Turner P, Hellestrand K et al. Evaluation of the efficacy of flecainide acetate in the treatment of ventricular premature contractions. Postgrad Med J. 1985; 61:489-96. https://pubmed.ncbi.nlm.nih.gov/2409543
97. Vanhaleweyk G, Balakumaran K, Lubsen J et al. Flecainide: one-year efficacy in patients with chronic ventricular arrhythmias. Eur Heart J. 1984; 5:814-23. https://pubmed.ncbi.nlm.nih.gov/6499854
98. Meinertz T, Zehender MK, Geibel A et al. Long-term antiarrhythmic therapy with flecainide. Am J Cardiol. 1984; 54:91-6. https://pubmed.ncbi.nlm.nih.gov/6741844
99. Webb CR, Morganroth J, Spielman SR et al. Use of flecainide for ventricular tachycardia in patients with left ventricular dysfunction. J Am Coll Cardiol. 1985; 5:482.
100. Lee G, Lui HK, Stobbe D et al. Efficacy of flecainide in patients with serious ventricular dysrhythmias unresponsive to conventional oral antiarrhythmic agents. Clin Res. 1983; 31:199A.
101. Salerno DM, Hodges M, Granrud G et al. Comparison of flecainide with quinidine for suppression of chronic stable ventricular ectopic depolarizations: a double-blind randomized study in ambulatory outpatients. Ann Intern Med. 1983; 98:455-60. https://pubmed.ncbi.nlm.nih.gov/6340575
102. Flecainide-Quinidine Research Group. Flecainide versus quinidine for treatment of chronic ventricular arrhythmias: a multicenter clinical trial. Circulation. 1983; 67:1117-23. https://pubmed.ncbi.nlm.nih.gov/6339110
103. Hodges M, Salerno DM, Granrud G et al. Flecainide versus quinidine: results of a multicenter trial. Am J Cardiol. 1984; 53:66-71B.
104. Kjekshus J, Bathen J, Orning OM et al. A double-blind, crossover comparison of flecainide acetate and disopyramide phosphate in the treatment of ventricular premature complexes. Am J Cardiol. 1984; 53:72-8B.
105. Klempt HW, Nayebagha A, Fabry E. Antiarrhythmic efficacy of mexiletine, propafenone and flecainide in ventricular premature beats: a comparative study in patients after myocardial infarction. (German; with English abstract.) Z Kardiol. 1982; 71:340-9.
106. Dubner SJ, Elencwajg BD, Palma S et al. Efficacy of flecainide in the management of ventricular arrhythmias: comparative study with amiodarone. Am Heart J. 1985; 109:523-8. https://pubmed.ncbi.nlm.nih.gov/3883728
107. Anon. Flecainide: a new antiarrhythmic drug. Med Lett Drugs Ther. 1986; 28:19-20. https://pubmed.ncbi.nlm.nih.gov/3951388
108. Zipes DP. A consideration of antiarrhythmic therapy. Circulation. 1985; 72:949-56. https://pubmed.ncbi.nlm.nih.gov/3930087
109. Stroobandt R, Andries E, van Mieghiem W et al. Efficacy and tolerance of intravenous flecainide in patients with chronic high frequency ventricular arrhythmias. Eur Heart J. 1984; 5:876-82. https://pubmed.ncbi.nlm.nih.gov/6397356
110. Slama R, LeClerq JF. The clinical use of oral flecainide. Drugs. 1985; 29(Suppl 4):28-9. https://pubmed.ncbi.nlm.nih.gov/4006778
111. Stern H, Scheininger M, Theisen F et al. Antiarrhythmic therapy with flecainide in combination and comparison with propranolol. Drugs. 1985; 29(Suppl 4):77-85. https://pubmed.ncbi.nlm.nih.gov/4006784
112. Coumel P, Chouty F, Slama R. Logic and empiricism in the selection of antiarrhythmic agents: the role of drug combinations. Drugs. 1985; 29(Suppl 4):68-76. https://pubmed.ncbi.nlm.nih.gov/4006782
113. Orning OM. The use of tocainide, encainide, lorcainide and flecainide for supraventricular arrhythmias. Eur Heart J. 1984; 5(Suppl B):81-6. https://pubmed.ncbi.nlm.nih.gov/6437821
114. Camm AJ, Hellestrand KJ, Nathan AW et al. Clinical usefulness of flecainide acetate in the treatment of paroxysmal supraventricular arrhythmias. Drugs. 1985; 29(Suppl 4):7-13. https://pubmed.ncbi.nlm.nih.gov/4006783
115. Neuss H. Long term use of flecainide in patients with supraventricular tachycardia. Drugs. 1985; 29(Suppl 4):21-5. https://pubmed.ncbi.nlm.nih.gov/4006776
116. Kappenberger LJ, Fromer MA, Shenasa M et al. Evaluation of flecainide acetate in rapid atrial fibrillation complicating Wolff-Parkinson-White syndrome. Clin Cardiol. 1985; 8:321-6. https://pubmed.ncbi.nlm.nih.gov/4006340
117. Goy JJ, Grbic M, Hurni M et al. Conversion of supraventricular arrhythmias to sinus rhythm using flecainide. Eur Heart J. 1985; 6:518-24. https://pubmed.ncbi.nlm.nih.gov/4043101
118. Goy JJ, Maendly R, Grbic M et al. Cardioversion with flecainide in patients with atrial fibrillation of recent onset. Eur J Clin Pharmacol. 1985; 27:737-8. https://pubmed.ncbi.nlm.nih.gov/3987780
119. Rae BG, Ilsley CDJ, Ablett MB. Flecainide acetate in resistant atrial fibrillation. N Z Med J. 1985; 98:402. https://pubmed.ncbi.nlm.nih.gov/3857526
120. Creamer JE, Nathan AW, Camm AJ. Successful treatment of atrial tachycardias with flecainide acetate. Br Heart J. 1985; 53:164-6. https://pubmed.ncbi.nlm.nih.gov/3966957
121. Frais MA, Silke B, Verma SP et al. Comparative effects of intravenous disopyramide and flecainide in acute myocardial infarction. Br J Clin Pharmacol. 1985; 20:522P.
122. Frank R, Fontaine G, Tonet JL et al. Treatment of severe chronic ventricular arrhythmias by flecainide combined with amiodarone. Eur Heart J. 1984; 5(Suppl 1):181. https://pubmed.ncbi.nlm.nih.gov/6241892
123. Agarwal AK, Lochan RG, Beard D et al. Efficacy of flecainide in the control of ventricular response during exercise in established atrial fibrillation in digitalised patients: its comparison with beta blockade. Br Heart J. 1985; 54:611.
124. Gentzkow GD, Sullivan JY. Extracardiac adverse effects of flecainide. Am J Cardiol. 1984; 53:101-5B.
125. Livelli FD Jr, Ferrick KJ, Bigger JT Jr et al. Mixed response to flecainide acetate. J Am Coll Cardiol. 1984; 3:583.
126. Griffith L, Platia E, Ord S et al. Persistent ventricular tachycardia/fibrillation: a possible adverse interaction between flecainide and class I anti-arrhythmic drugs. J Am Coll Cardiol. 1984; 3:583.
127. Ward DE, Jones S, Shinebourne EA. Use of flecainide acetate for refractory junctional tachycardias in children with the Wolff-Parkinson-White syndrome. Am J Cardiol. 1986; 57:787-90. https://pubmed.ncbi.nlm.nih.gov/3962866
128. Case MT, Sibinski LJ, Steffen GR. Chronic oral toxicity and oncogenicity studies of flecainide, an antiarrhythmic, in rats and mice. Toxicol Appl Pharmacol. 1984; 73:232-42. https://pubmed.ncbi.nlm.nih.gov/6710523
129. Penhall RK, Hong CY, Muhiddin KA. The effect of flecainide on human sperm motility. Br J Clin Pharmacol. 1982; 14:147P.
130. Gosselin RE, Smith RP, Hodge HC. Clinical toxicology of commercial products. 5th ed. Baltimore: The Williams & Wilkins Co; 1984:I10.
131. Wyeth Laboratories Inc. Cordarone (amiodarone HCl) prescribing information. Philadelphia, PA; 1987 Jan.
132. Tjandramaga TB, Verbesselt R, Van Hecken A et al. Oral digoxin pharmacokinetics during multiple-dose flecainide treatment. Arch Int Pharmacodyn Ther. 1982; 260:302-3. https://pubmed.ncbi.nlm.nih.gov/7165437
133. Lewis GP, Holtzman JL. Interaction of flecainide with digoxin and propranolol. Am J Cardiol. 1984; 53:52-7B.
134. Weeks CE, Conard GJ, Kvam DC et al. The effect of flecainide acetate, a new antiarrhythmic, on plasma digoxin levels. J Clin Pharmacol. 1986; 26:27-31. https://pubmed.ncbi.nlm.nih.gov/3950050
135. Tjandramaga TB, Verbesselt R, Van Hecken A et al. Oral flecainide elimination kinetics: effects of cimetidine. Circulation. 1983; 68(4 Part II):III-416.
136. Reviewers’ comments (personal observations).
137. McQuinn RL, Weeks CE, Kvam DC et al. Pharmacokinetics of flecainide in elderly subjects. Clin Pharmacol Ther. 1986; 39:210.
138. Crozier I, Ikram H. Flecainide acetate in atrial fibrillation. N Z Med J. 1985; 98:506. https://pubmed.ncbi.nlm.nih.gov/3859778
139. Zweber MB (Riker Laboratories, Inc; St. Paul, MN): Personal communication.
140. Kim SS, Lal R, Ruffy R. Treatment of paroxysmal reentrant supraventricular tachycardia with flecainide acetate. Am J Cardiol. 1986; 58:80-5. https://pubmed.ncbi.nlm.nih.gov/3728336
141. Ruffy R, Sears M. Wolff-Parkinson-White syndrome. JAMA. 1985; 145:533-6.
142. Shea P, Lal R, Kim SS et al. Flecainide and amiodarone interaction. J Am Coll Cardiol. 1986; 7:1127-30. https://pubmed.ncbi.nlm.nih.gov/3958371
143. Anderson JL. Proarrhythmic effects of antiarrhythmic drug therapy. In: Smith WM, ed. Forum on the management of arrhythmias: the role of flecainide. Auckland, New Zealand: ADIS Press Limited; 1985:41-50.
144. Riker Laboratories Australia Pty Ltd. Tambocor tablets and injection prescribing information. Thornleigh, Australia; 1985 Oct.
145. Webb CR, Morganroth J, Senior S et al. Flecainide: steady state electrophysiologic effects in patients with remote myocardial infarction and inducible sustained ventricular arrhythmia. J Am Coll Cardiol. 1986; 8:214-20. https://pubmed.ncbi.nlm.nih.gov/3711519
146. Roden DM, Woosley RL. Flecainide. N Engl J Med. 1986; 315:36-41. https://pubmed.ncbi.nlm.nih.gov/3520324
147. Somberg JC, Tepper D. Flecainide: a new antiarrhythmic agent. Am Heart J. 1986; 112:808-13. https://pubmed.ncbi.nlm.nih.gov/3094352
148. Borgeat A, Goy JJ, Maendly R et al. Flecainide versus quinidine for conversion of atrial fibrillation to sinus rhythm. Am J Cardiol. 1986; 58:496-8. https://pubmed.ncbi.nlm.nih.gov/3529911
149. Kunze KP, Kuck KH, Schluter M et al. Effect of encainide and flecainide on chronic ectopic atrial tachycardia. J Am Coll Cardiol. 1986; 7:1121-6. https://pubmed.ncbi.nlm.nih.gov/3082957
150. Lal R, Chapman PD, Naccarelli GV et al. Flecainide in the treatment of nonsustained ventricular tachycardia. Ann Intern Med. 1986; 105:493-8. https://pubmed.ncbi.nlm.nih.gov/3752754
151. Morganroth J, Anderson JL, Gentzkow GD. Classification by type of ventricular arrhythmia predicts frequency of adverse cardiac events from flecainide. J Am Coll Cardiol. 1986; 8:607-15. https://pubmed.ncbi.nlm.nih.gov/3745706
152. Nitsch J, Kohler U, Neyses L et al. Inhibition of flecainide absorption by activated charcoal. Am J Cardiol. 1987; 60:753. https://pubmed.ncbi.nlm.nih.gov/3116835
153. Samlowski WE, Frame RN, Logue GL. Flecainide-induced immune neutropenia: documentation of a hapten-mediated mechanism of cell destruction. Arch Intern Med. 1987; 147:383-4. https://pubmed.ncbi.nlm.nih.gov/2434046
154. de Paola AAV, Horowitz LN, Morganroth J et al. Influence of left ventricular dysfunction on flecainide therapy. J Am Coll Cardiol. 1987; 9:163-8. https://pubmed.ncbi.nlm.nih.gov/3098817
155. Winkelmann BR, Leinberger H. Life-threatening flecainide toxicity: a pharmacodynamic approach. Ann Intern Med. 1987; 106:807-14. https://pubmed.ncbi.nlm.nih.gov/3107447
156. Fontaine G, Frank R, Tonet JL. Association amiodarone-flécainide dans le traitement des troubles du rythme ventriculaires graves. Arch Mal Coeur. 1984; 77:1421. https://pubmed.ncbi.nlm.nih.gov/6439167
157. Leclercq JF, Coumel P. Association amiodarone-flécainide dans le traitement des troubles du rythme ventriculaires graves. Arch Mal Coeur. 1984; 77:1421-2. https://pubmed.ncbi.nlm.nih.gov/6439167
158. Crijns HJGM, Kingma JH, Viersma JW et al. Transient giant inverted T waves during flecainide intoxication. Am Heart J. 1987; 113:214-5. https://pubmed.ncbi.nlm.nih.gov/3099561
159. Anastasiou-Nana MI, Anderson JL, Stewart JR et al. Occurrence of exercise-induced and spontaneous wide complex tachycardia during therapy with flecainide for complex ventricular arrhythmias, a probable proarrhythmic effect. Am Heart J. 1987; 113:1071-7. https://pubmed.ncbi.nlm.nih.gov/3107362
160. Leclercq JF, Coumel P. La flécainide: un nouvel antiarythmique. Arch Mal Coeur. 1983; 76:1218-29. https://pubmed.ncbi.nlm.nih.gov/6418100
161. Food and Drug Administration. Enkaid and Tambocor use in non-life-threatening arrhythmias halted. FDA Talk Paper. 1989 Apr 25.
162. Department of Health and Human Services. Background statement regarding encainide, flecainide, and moricizine. Bethesda, MD: National Institutes of Health, National Heart, Lung, and Blood Institute; 1989 Apr.
163. The Cardiac Arrhythmia Suppression Trial (CAST) investigators. Preliminary report: effect of encainide and flecainide on mortality in a randomized trial of arrhythmia suppression after myocardial infarction. N Engl J Med. 1989; 321:406-12. https://pubmed.ncbi.nlm.nih.gov/2473403
164. Ruskin JN. The Cardiac Arrhythmia Suppression Trial (CAST). N Engl J Med. 1989; 321:386-8. https://pubmed.ncbi.nlm.nih.gov/2501683
166. Food and Drug Administration. FDA Cardio-renal Advisory Committee will review CAST study. FDC Rep. 1989(Aug 14):3-4.
167. Greene HL, Richardson DW, Barker AH et al. Classification of deaths after myocardial infarction as arrhythmic or nonarrhythmic (the Cardiac Arrhythmia Pilot Study). Am J Cardiol. 1989; 63:1-6. https://pubmed.ncbi.nlm.nih.gov/2462341
168. Greene HL, Richardson DW, Hallstrom AP et al. Congestive heart failure after acute myocardial infarction in patients receiving antiarrhythmic agents for ventricular premature complexes (Cardiac Arrhythmia Pilot Study). Am J Cardiol. 1989; 63:393-8. https://pubmed.ncbi.nlm.nih.gov/2464919
169. Vlay SC. Lessons from the past and reflections on the Cardiac Arrhythmia Suppression trial. Am J Cardiol. 1990; 65:112-3. https://pubmed.ncbi.nlm.nih.gov/1688480
170. Pratt CM, Brater DC, Harrell FE Jr et al. Clinical and regulatory implications of the Cardiac Arrhythmia Suppression Trial. Am J Cardiol. 1990; 65:103-5. https://pubmed.ncbi.nlm.nih.gov/1688479
171. Morganroth J, Bigger JT Jr, Anderson JL. Treatment of ventricular arrhythmias by United States cardiologists: a survey before the Cardiac Arrhythmia Suppression Trial results were available. Am J Cardiol. 1990; 65:40-8. https://pubmed.ncbi.nlm.nih.gov/1688481
172. Thomas GS. Death following withdrawal of encainide. N Engl J Med. 1989; 321:393-4. https://pubmed.ncbi.nlm.nih.gov/2501684
173. Garratt C, Ward DE, Camm AJ. Lessons from the cardiac arrhythmia suppression trial. BMJ. 1989; 299:805-6. https://pubmed.ncbi.nlm.nih.gov/2510839
174. Coyle JD, Schaal SF. An interim perspective on the removal of encainide and flecainide from the Cardiac Arrhythmia Suppression Trial. DICP. 1989; 23:478-9. https://pubmed.ncbi.nlm.nih.gov/2500783
175. Anon. Drugs for cardiac arrhythmias: new warning. Med Lett Drugs Ther. 1989; 31:48. https://pubmed.ncbi.nlm.nih.gov/2497313
176. Nightingale SL. Flecainide and encainide not to be used in non-life-threatening arrhythmias. JAMA. 1989; 261:3368. https://pubmed.ncbi.nlm.nih.gov/2498536
177. Anon. Restrictions on use of flecainide, encainide. FDA Drug Bull. 1989; 16.
178. Eagleton G. Dear doctor letter regarding appropriate uses of Tambocor. St. Paul, MN: 3M Riker; 1989 May.
179. Anon. Dear pharmacist letter regarding appropriate uses of Tambocor. St. Paul, MN: 3M Riker; 1989 May.
180. The Cardiac Arrhythmia Pilot Study (CAPS) Investigators. Effects of encainide, flecainide, imipramine and moricizine on ventricular arrhythmias during the year after acute myocardial infarction: the CAPS. Am J Cardiol. 1988; 61:501-9. https://pubmed.ncbi.nlm.nih.gov/2894169
181. Anon. Flecainide and CAST. Lancet. 1989; 2:481-2. https://pubmed.ncbi.nlm.nih.gov/2570188
182. Reviewers’ comments (personal observations); 1990 Jan.
183. Ward D, Garratt C, Camm AJ. Cardiac arrhythmia suppression trial and flecainide. Lancet. 1989; 1:1267-8. https://pubmed.ncbi.nlm.nih.gov/2566810
184. Pratt CM, Podrid P, Greatrix B et al. Efficacy and safety of moricizine in patients with congestive heart failure: a summary of the experience in the United States. Am Heart J. 1990; 119:1-7. https://pubmed.ncbi.nlm.nih.gov/1688682
185. Falk RH. Flecainide-induced ventricular tachycardia and fibrillation in patients treated for atrial fibrillation. Ann Intern Med. 1989; 111:107-11. https://pubmed.ncbi.nlm.nih.gov/2500880
186. Jones K, Wood SM. Indications for flecainide. Lancet. 1989; 1:1383. https://pubmed.ncbi.nlm.nih.gov/2567388
187. Robson RH. Indications for flecainide. Lancet. 1989; 2:113.
188. Bigger JT Jr. Indications for flecainide. Lancet. 1989; 2:113-4.
189. Ray J. Flecainide: what are we measuring? Ther Drug Monit. 1990; 12:416. Letter.
190. Echt DS, Liebson PR, Mitchell LB et al. Mortality and morbidity in patients receiving encainide, flecainide, or placebo: the Cardiac Arrhythmia Suppression Trial. N Engl J Med. 1991; 324:781-8. https://pubmed.ncbi.nlm.nih.gov/1900101
191. Anon. CAST deaths revealed. Lancet. 1991; 337:969.
192. Tambocor (flecainide acetate): its role in the treatment of supraventricular arrhythmias. St. Paul, MN: 1991.
193. Henthorn RW, Waldo AL, Anderson JL et al. Flecainide acetate prevents recurrence of symptomatic paroxysmal supraventricular tachycardia. Circulation. 1991; 83:119-25. https://pubmed.ncbi.nlm.nih.gov/1898640
194. Anderson JL, Gilbert EM, Alpert BL et al. Prevention of symptomatic recurrences of paroxysmal atrial fibrillation in patients initially tolerating antiarrythmic therapy: a multicenter, double-blind, crossover study of flecainide and placebo with transtelephonic monitoring. Circulation. 1989; 80:1557-70. https://pubmed.ncbi.nlm.nih.gov/2513143
195. Pritchett ELC, Wilkinson WE. Mortality in patients treated with flecainide and encainide for supraventricular arrhythmias. Am J Cardio. 1991; 67:976-80.
196. Cockrell JL, Scheinman MM, Titus C et al. Safety and efficacy of oral flecainide therapy in patients with atrioventricular re-entrant tachycardia. Ann Intern Med. 1991; 114:189-94. https://pubmed.ncbi.nlm.nih.gov/1898629
197. Pietersen AH, Hellemann H. Usefulness of flecainide for prevention of paroxysmal atrial fibrillation and flutter. Am J Cardiol. 1991; 67:713-7. https://pubmed.ncbi.nlm.nih.gov/1900978
198. Benditt DG, Dunnigan A, Buetikofer J et al. Flecainide acetate for long-term prevention of paroxysmal supraventricular tachyarrhythmias. Circulation. 1991; 83:345-9. https://pubmed.ncbi.nlm.nih.gov/1898643
199. van Wijk LM, den Heijer P, Crijns HJ et al. Flecainide versus quinidine in the prevention of paroxysms of atrial fibrillation. J Cardiovasc Pharmacol. 1989; 13:32-6. https://pubmed.ncbi.nlm.nih.gov/2468933
200. Pritchett ELC, DaTorre SD, Platt ML et al. Flecainide acetate treatment of paroxysmal supraventricular tachycardia and paroxysmal atrial fibrillation: dose-response studies. J Am Coll Cardiol. 1991; 17:297-303. https://pubmed.ncbi.nlm.nih.gov/1899432
201. Hughes MM, Trohman RG, Simmons TW et al. Flecainide therapy in patients treated for supraventricular tachycardia with near normal left ventricular function. Am Heart J. 1992; 123:408. https://pubmed.ncbi.nlm.nih.gov/1736577
202. Suttorp MJ, Kingma JH, Lie-A-Huen L et al. Intravenous flecainide versus verapamil for acute conversion of paroxysmal atrial fibrillation or flutter to sinus rhythm. Am J Cardiol. 1989; 63:693-6. https://pubmed.ncbi.nlm.nih.gov/2493733
203. Berns E, Rinkenberger RL, Jeang MK et al. Efficacy and safety of flecainide acetate for atrial tachycardia or fibrillation. Am J Cardiol. 1987; 59:1337-41. https://pubmed.ncbi.nlm.nih.gov/3109229
204. Crozier IG, Ikram H, Kenealy M et al. Flecainide acetate for conversion of acute supraventricular tachycardia to sinus rhythm. Am J Cardiol. 197; 59:607-9.
205. Goy JJ, Kaufmann U, Kappenberger L et al. Restortation [sic] of sinus rhythm with flecainide in patients with atrial fibrillation. Am J Cardiol. 1988; 62(Suppl):38-40D.
206. Anon. Flecainide for supraventricular tachyarrhythmias. Med Lett Drugs Ther. 1992; 34:71-2. https://pubmed.ncbi.nlm.nih.gov/1630411
207. Reviewers’ comments (personal observations): 1992 Nov.
208. Flaker GC, Blackshear JL, McBride R et al. Antiarrhythmic drug therapy and cardiac mortality in atrial fibrillation. J Am Coll Cardiol. 1992; 20:527-32. https://pubmed.ncbi.nlm.nih.gov/1512329
209. Coplen SE, Antman EM, Berlin JA et al. Efficacy and safety of quinidine therapy for maintenance of sinus rhythm after cardioversion: a meta-analysis of randomized control trials. Circulation. 1990; 82:1106-16. https://pubmed.ncbi.nlm.nih.gov/2144796
210. The United States pharmacopeia, 23rd rev, and the national formulary, 18th ed. Rockville, MD: The United States Pharmacopeial Convention, Inc; 1995(Suppl 1):2462-3.
211. Epstein AE, Hallstrom AP, Rogers WJ et al. mortality following ventricular arrhythmia suppression by encainide, flecainide, and moricizine after myocardial infarction: the original design concept of the Cardiac Arrhythmia Suppression Trial (CAST). JAMA. 1993; 270:2451-5. https://pubmed.ncbi.nlm.nih.gov/8230622
212. Searle. Norpace and Norpace CR (disopyramide phosphate) capsules prescribing information. In: Physicians’ desk reference. 50th ed. Montvale, NJ: Medical Economics Company Inc; 1996 (Suppl A):A141.
213. Berlex. Quinaglute Dura-tabs (quinidine gluconate) tablets prescribing information (dated 1994 Dec). In: Physicians’ desk reference. 50th ed. Montvale, NJ: Medical Economics Company Inc; 1996:649-651.
214. Perdue Frederick. Cardioquin (quinidine polygalacturonate) tablets prescribing information (dated 1995 Aug). In: Physicians’ desk reference. 50th ed. Montvale, NJ: Medical Economics Company Inc; 1996 (Suppl A):A57-A59.
215. Parke-Davis. ProcanSR (procainamide hydrochloride) extended-release tablets prescribing information (dated 1994 Sep). In: Physicians’ desk reference. 50th ed. Montvale, NJ: Medical Economics Company Inc; 1996:1926-8.
216. Astra Merck. Tonocard (tocainide hydrochloride) tablets information (dated 1994 Aug). In: Physicians’ desk reference. 50th ed. Montvale, NJ: Medical Economics Company Inc; 1996:531-4.
217. Boehringer Ingelheim. Mexitil (mexiletine hydrochloride) capsules prescribing information (dated 1993 Oct). In: Physicians’ desk reference. 50th ed. Montvale, NJ: Medical Economics Company Inc; 1996:678-81.
219. Lui CY, Franchina JJ. Verapamil and multifocal atrial tachycardia. Ann Intern Med. 1988; 108:485-6.
220. Scher DL, Arsura EL. Multifocal atrial tachycardia: mechanisms, clinical correlates, and treatment. Am Heart J. 1989; 118:574-80. https://pubmed.ncbi.nlm.nih.gov/2570520
221. Arsura EL, Scher DL. Verapamil and multifocal atrial tachycardia. Ann Intern Med. 1988; 108:486. https://pubmed.ncbi.nlm.nih.gov/3341685
222. Levine JH, Michael JR, Guarnieri T. Verapamil for multifocal atrial tachycardia. N Engl J Med. 1985; 312:1126-7. Reply.
223. Arsura E, Lefkin AS, Scher DL et al. A randomized, double-blind, placebo-controlled study of verapamil and metoprolol in treatment of multifocal atrial tachycardia. Am J Med. 1988; 85:519-24. https://pubmed.ncbi.nlm.nih.gov/3052051
224. Alboni P, Botto GL, Baldi Net al. Outpatient treatment of recent-onset atrial fibrillation with the “pill-in-the-pocket” approach. N Engl J Med. 2004; 351:2384-91. https://pubmed.ncbi.nlm.nih.gov/15575054
225. Gronefeld GC, Hohnloser SH. The “pill-in-the-pocket” approach to atrial fibrillation. N Engl J Med. 2005; 352:1150. https://pubmed.ncbi.nlm.nih.gov/15784671
226. Konety SH, Olshansky B. The “pill-in-the-pocket” approach to atrial fibrillation. N Engl J Med. 2005; 352:1150. https://pubmed.ncbi.nlm.nih.gov/15789457
227. Wittkowsky AK. The “pill-in-the-pocket” approach to atrial fibrillation. N Engl J Med. 2005; 352:1150-1. https://pubmed.ncbi.nlm.nih.gov/15789456
228. Alboni P, Botto GI, Baldi N. The “pill-in-the-pocket” approach to atrial fibrillation. N Engl J Med. 2005; 352:1151.
229. Botto GL, Capucci A, Bonini W et al. Conversion of recent onset atrial fibrillation to sinus rhythm using a single oral loading dose of propafenone: comparison of two regimens. Int J Cardiol. 1997; 58:55-61. https://pubmed.ncbi.nlm.nih.gov/9021428
230. Boriani G, Biffi M, Capucci A et al. Oral propafenone to convert recent-onset atrial fibrillation in patients with and without underlying heart disease. A randomized, controlled trial. Ann Intern Med. 1997; 126:621-5. https://pubmed.ncbi.nlm.nih.gov/9103129
231. Azpitarte J, Alvarez M, Baun O et al. Value of single oral loading dose of propafenone in converting recent-onset atrial fibrillation. Results of a randomized, double-blind, controlled study. Eur Heart J. 1997; 18:1649-54. https://pubmed.ncbi.nlm.nih.gov/9347277
232. Boriani G, Biffi M, Capucci A et al. Oral loading with propafenone: a placebo-controlled study in elderly and nonelderly patients with recent onset atrial fibrillation. Pacing Clin Electrophysiol. 1998; 21(11 Pt 2):2465-9. https://pubmed.ncbi.nlm.nih.gov/9825368
233. Boriani G, Biffi M, Capucci A et al. Conversion of recent-onset atrial fibrillation to sinus rhythm: effects of different drug protocols. Pacing Clin Electrophysiol. 1998; 21(11 Pt 2):2470-4. https://pubmed.ncbi.nlm.nih.gov/9825369
234. Capucci A, Villani GQ, Aschieri D et al. Safety of oral propafenone in the conversion of recent onset atrial fibrillation to sinus rhythm: a prospective parallel placebo-controlled multicentre study. Int J Cardiol. 1999; 68:187-96. https://pubmed.ncbi.nlm.nih.gov/10189007
235. Alboni P, Tomasi C, Menozzi C et al. Efficacy and safety of out-of-hospital self-administered single-dose oral drug treatment in the management of infrequent, well-tolerated paroxysmal supraventricular tachycardia. J Am Coll Cardiol. 2001; 37:548-53. https://pubmed.ncbi.nlm.nih.gov/11216977
236. Capucci A, Lenzi T, Boriani G et al. Effectiveness of loading oral flecainide for converting recent-onset atrial fibrillation to sinus rhythm in patients without organic heart disease or with only systemic hypertension. Am J Cardiol. 1992; 70:69-72. https://pubmed.ncbi.nlm.nih.gov/1615873
237. Blanc JJ, Voinov C, Maarek M. Comparison of oral loading dose of propafenone and amiodarone for converting recent-onset atrial fibrillation. PARSIFAL Study Group. Am J Cardiol. 1999; 84:1029-32. https://pubmed.ncbi.nlm.nih.gov/10569658
238. Khan IA. Single oral loading dose of propafenone for pharmacological cardioversion of recent-onset atrial fibrillation. J Am Coll Cardiol. 2001; 37:542-7. https://pubmed.ncbi.nlm.nih.gov/11216976
239. Boriani G, Martignani C, Biffi M et al. Oral loading with propafenone for conversion of recent-onset atrial fibrillation: a review on in-hospital treatment. Drugs. 2002; 62:415-23. https://pubmed.ncbi.nlm.nih.gov/11827557
240. Khan IA. Oral loading single dose flecainide for pharmacological cardioversion of recent-onset atrial fibrillation. Int J Cardiol. 2003; 87:121-8. https://pubmed.ncbi.nlm.nih.gov/12559528
241. Deneer VH, Borgh MB, Kingma JH et al. Oral antiarrhythmic drugs in converting recent onset atrial fibrillation. Pharm World Sci. 2004; 26:66-78. https://pubmed.ncbi.nlm.nih.gov/15085940
242. Reviewers’ comments (personal observations).
243. Van Gelder IC, Brugemann J, Crijns HJGM. Pharmacological management of arrhythmias in the elderly. Drugs Aging. 1997; 11:96-110. https://pubmed.ncbi.nlm.nih.gov/9259173
244. Jung F, DiMarco JP. Treatment strategies for atrial fibrillation. Am J Med. 1998; 104:272-86. https://pubmed.ncbi.nlm.nih.gov/9552091
246. Novartis Pharmaceuticals. Clozaril (clozapine) prescribing information. East Hanover, NJ; 2005 May.
247. Casiraghi A, Centin G, Selmin F et al. Critical Aspects in the Preparation of Extemporaneous Flecainide Acetate Oral Solution for Paediatrics. Pharmaceutics. 2021 Nov 19;13(11):1963. doi: 10.3390/pharmaceutics13111963. PMID: 34834378; PMCID: PMC8618881.
252. ASHP. Standardize 4 Safety: compounded oral liquid standards. Updated 2024 Mar. From ASHP website. Updates may be available at ASHP website. https://www.ashp.org/standardize4safety
300. Page RL, Joglar JA, Caldwell MA et al. 2015 ACC/AHA/HRS Guideline for the Management of Adult Patients With Supraventricular Tachycardia: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2016; 67:e27-e115.
301. January CT, Wann LS, Alpert JS et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014; 64:e1-76. https://pubmed.ncbi.nlm.nih.gov/24685669
302. Al-Khatib SM, Stevenson WG, Ackerman MJ et al. 2017 AHA/ACC/HRS Guideline for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation. 2017; https://pubmed.ncbi.nlm.nih.gov/29084733
Related/similar drugs
Xarelto
Xarelto (rivaroxaban) is a factor Xa inhibitor used to reduce the risk of blood clots and stroke in ...
Cardizem
Cardizem is used to treat hypertension (high blood pressure), angina (chest pain), and heart rhythm ...
Botox
Botox is used cosmetically to reduce facial lines and wrinkles and for medical purposes for ...
Lanoxin
Lanoxin (digoxin) is used to treat congestive heart failure and atrial fibrillation. Includes ...
Multaq
Multaq (dronedarone) is an antiarrhythmic medication used to treat atrial fibrillation and atrial ...
Edoxaban
Edoxaban is used for atrial fibrillation, deep vein thrombosis, prevention of thromboembolism in ...
Propafenone
Propafenone is used for atrial fibrillation, atrial flutter, ventricular tachycardia ...
Sotalol
Sotalol is a beta-blocker with antiarrhythmic properties that affects the heart and circulation ...
Rivaroxaban
Rivaroxaban is used for atrial fibrillation, cardiovascular risk reduction, congenital heart ...
More about flecainide
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (177)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Support group
- Drug class: group I antiarrhythmics
- Breastfeeding
- En español