Ethosuximide (Monograph)
Brand name: Zarontin
Drug class: Succinimides
VA class: CN400
Chemical name: 3-Ethyl-3-methyl-2,5-pyrrolidinedione
Molecular formula: C7H11NO2
CAS number: 77-67-8
Introduction
Succinimide-derivative anticonvulsant; structurally related to other succinimide anticonvulsants (e.g., methsuximide, phensuximide [no longer commercially available in the US]).
Uses for Ethosuximide
Absence Seizures
Monotherapy or adjunctive therapy (i.e., in conjunction with other anticonvulsants) in the prophylactic management of absence (petit mal) seizures; generally considered first-line anticonvulsant drug of choice for such seizures.
Usually ineffective in management of other seizure types such as partial seizures† [off-label] or generalized tonic-clonic seizures† [off-label].
May use concomitantly with other anticonvulsants (e.g., valproic acid) for treatment of coexisting seizure types (e.g., generalized tonic-clonic seizures). (See Specific Drugs under Interactions.)
Ethosuximide Dosage and Administration
General
-
Closely monitor for notable changes in behavior that could indicate emergence or worsening of suicidal thoughts or behavior or depression. (See Suicidality Risk under Cautions.)
-
Proceed slowly with ethosuximide dosage increases or decreases, when adding or withdrawing another anticonvulsant, or when replacing one anticonvulsant with another. Do not discontinue abruptly to avoid precipitating seizures or absence status. (See Discontinuance of Therapy under Cautions.)
Administration
Administer orally as a capsule or oral solution without regard to meals. However, administration with food and/or fluids may help minimize adverse GI effects.
Dosage
Carefully and slowly adjust dosage according to individual requirements and response.
Pediatric Patients
Absence Seizures
Oral
Children 3–6 years of age: Initially, 250 mg daily in a single dose.
Children ≥6 years of age: Initially, 500 mg daily in a single dose or divided doses.
Increase dosage in small increments. One method of establishing maintenance dosage is to slowly increase the daily dosage by 250 mg every 4–7 days until seizure control is achieved with minimal adverse effects. Dosage usually should not be >1.5 g daily, given in divided doses. If dosage is >1.5 g daily, clinician must closely supervise patient.
Usual maintenance dosage: 20 mg/kg or 1.2 g/m2 daily.
Some studies indicate that when patient is well stabilized, may give total daily dosage as one dose; however, clinical efficacy of once-daily regimen not established.
Adults
Absence Seizures
Oral
Initially, 500 mg daily in a single dose or divided doses.
Increase dosage in small increments. One method of establishing maintenance dosage is to slowly increase the daily dosage by 250 mg every 4–7 days until seizure control is achieved with minimal adverse effects. Dosage usually should not be >1.5 g daily, given in divided doses. If dosage is >1.5 g daily, clinician must closely supervise patient.
Usual maintenance dosage: 20 mg/kg or 1.2 g/m2 daily.
Some studies indicate that when patient is well stabilized, may give total daily dosage as one dose; however, clinical efficacy of once-daily regimen not established.
Prescribing Limits
Pediatric Patients
Absence Seizures
Oral
Maximum 1.5 g daily. Closely supervise patient if dosage is >1.5 g daily.
Adults
Absence Seizures
Oral
Maximum 1.5 g daily. Closely supervise patient if dosage is >1.5 g daily.
Special Populations
Renal Impairment
Patients undergoing hemodialysis may require a supplemental dose following each dialysis session or dosage adjustment. (See Renal Impairment under Cautions.)
Cautions for Ethosuximide
Contraindications
-
Known hypersensitivity to ethosuximide or other succinimides (e.g., methsuximide, phensuximide [no longer commercially available in the US]).
Warnings/Precautions
Warnings
Shares the toxic potentials of the succinimide-derivative anticonvulsants, and the usual precautions of anticonvulsant therapy should be observed.
Hematologic Effects
Blood dyscrasias (e.g., leukopenia, agranulocytosis, pancytopenia with or without bone marrow suppression, aplastic anemia, eosinophilia), sometimes fatal, reported. Obtain CBC at baseline and periodically during therapy. Also obtain CBC if signs and/or symptoms of infection (e.g., sore throat, fever) develop.
Hepatic Effects
Morphological and functional liver changes reported in animals. Abnormal liver function test results reported in humans. Obtain baseline and periodic evaluations of hepatic function.
Renal Effects
Abnormal renal function test results reported. Obtain urinalyses periodically.
Systemic Lupus Erythematosus
Systemic lupus erythematosus (SLE) reported; clinicians should be alert to this possibility.
Suicidality Risk
Increased risk of suicidality (suicidal ideation or behavior) observed in an analysis of studies using various anticonvulsants in patients with epilepsy, psychiatric disorders (e.g., bipolar disorder, depression, anxiety), and other conditions (e.g., migraine, neuropathic pain); risk in patients receiving anticonvulsants (0.43%) was approximately twice that in patients receiving placebo (0.24%). Increased suicidality risk was observed ≥1 week after initiation of anticonvulsant therapy and continued through 24 weeks. Risk was higher for patients with epilepsy compared with those receiving anticonvulsants for other conditions.
Closely monitor all patients currently receiving or beginning anticonvulsant therapy for changes in behavior that may indicate emergence or worsening of suicidal thoughts or behavior or depression.
Balance risk of suicidality with the risk of untreated illness. Epilepsy and other illnesses treated with anticonvulsants are themselves associated with morbidity and mortality and an increased risk of suicidality. If suicidal thoughts or behavior emerge during anticonvulsant therapy, consider whether these symptoms may be related to the illness itself. (See Advice to Patients.)
Dermatologic Reactions
Serious dermatologic reactions (e.g., Stevens-Johnson syndrome) reported. Onset usually within first 28 days of therapy, but may occur at any time.
Discontinue drug at the first sign of a rash (unless clearly not drug related). If manifestations are suggestive of Stevens-Johnson syndrome, do not resume therapy and consider alternative therapies.
Fetal/Neonatal Morbidity and Mortality
May cause fetal harm; cases of birth defects reported with ethosuximide. Reports suggest an association between use of anticonvulsants in pregnant, epileptic women and an increased incidence of birth defects in children born to these women; however, definite causal relationship not established. (See Pregnancy under Cautions.)
Sensitivity Reactions
Multi-organ Hypersensitivity Reactions
Multi-organ hypersensitivity (also known as drug reaction with eosinophilia and systemic symptoms [DRESS]) reported; potentially fatal or life-threatening. Clinical presentation is variable but typically includes fever, rash, lymphadenopathy, and/or facial swelling associated with other organ system involvement (e.g., eosinophilia, hepatitis, nephritis, hematologic abnormalities, myocarditis, myositis).
If a multi-organ hypersensitivity reaction is suspected, evaluate patient immediately. If an alternative cause cannot be identified, discontinue ethosuximide.
General Precautions
Seizures
May increase the frequency of tonic-clonic seizures when used alone in mixed seizures.
Discontinuance of Therapy
Abrupt withdrawal of anticonvulsants may precipitate absence (petit mal) status.
Specific Populations
Pregnancy
Risk of fetal harm. (See Fetal/Neonatal Morbidity and Mortality under Cautions.)
May consider discontinuance of the drug prior to and during pregnancy in individual cases where withdrawal of therapy does not pose a serious threat to the patient; however, there is a possibility that even minor seizures can adversely affect the developing fetus. Carefully weigh these considerations when treating or counseling epileptic women of childbearing potential.
North American Antiepileptic Drug (NAAED) Pregnancy Registry at 888-233-2334 (for patients); registry information also available on the website [Web].
Lactation
Distributes into breast milk. Caution if used in nursing women.
Pediatric Use
Safety and efficacy not established in children <3 years of age.
Hepatic Impairment
Use with extreme caution in patients with hepatic impairment or abnormal liver function test values. (See Hepatic Effects under Cautions.)
Renal Impairment
Use with extreme caution in patients with renal impairment. (See Renal Impairment under Dosage and Administration and see Renal Effects under Cautions.)
Common Adverse Effects
Adverse GI effects (anorexia and weight loss, gastric upset, cramps, epigastric and abdominal pain, diarrhea, nausea, vomiting), drowsiness, or tiredness.
Drug Interactions
Drugs Affecting Hepatic Microsomal Enzymes
Pharmacokinetic interactions with inhibitors or inducers of CYP3A4 are possible.
Protein-bound Drugs
Does not substantially bind to plasma proteins; pharmacokinetic interaction with drugs that are highly protein bound unlikely.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Alcohol |
Potential additive CNS depressant effects |
|
|
Anticonvulsants (e.g., phenobarbital, phenytoin; see also valproic acid entry in this table) |
Pharmacokinetic interaction likely; possible increased and/or decreased antiepileptic concentrations |
If used concomitantly, closely monitor serum concentrations and adjust dosage of both anticonvulsants as required |
|
Antidepressants, tricyclic |
May precipitate seizures |
Monitor closely for decreased seizure control; adjust ethosuximide dosage if necessary |
|
CNS depressants |
Potential additive CNS depressant effects |
|
|
Isoniazid |
Possible increased or decreased plasma ethosuximide concentrations and effects |
|
|
Oral contraceptives |
Pharmacokinetic interaction unlikely |
|
|
Valproic acid |
Pharmacokinetic interaction likely; possible increased and/or decreased antiepileptic concentrations Valproic acid inhibits metabolism of ethosuximide; concurrent administration in healthy individuals resulted in a 25% increase in ethosuximide elimination half-life and a 15% decrease in total ethosuximide clearance |
If used concomitantly, closely monitor serum concentrations and adjust dosage of both anticonvulsants as required, particularly if receiving other anticonvulsants |
Ethosuximide Pharmacokinetics
Absorption
Bioavailability
Readily absorbed from the GI tract.
Peak plasma concentrations generally attained within 4 hours after single-dose, oral administration.
Plasma Concentrations
Anticonvulsant therapeutic range generally considered to be 40–100 mcg/mL; plasma concentrations <40 mcg/mL are rarely effective and plasma concentrations ≤150 mcg/mL have been reported without toxicity.
Distribution
Extent
Anticonvulsants generally are widely distributed in the body and succinimides are freely distributed throughout body water.
Crosses the placenta. Distributed into milk.
Plasma Protein Binding
Does not appear to be substantially protein bound.
Elimination
Metabolism
Metabolized in the liver via hydroxylation and glucuronide formation to several metabolites.
Elimination Route
Eliminated principally in urine, approximately 20% as unchanged drug and ≤50% as hydroxylated metabolite and/or its glucuronide. Small amount of unchanged drug excreted in bile and feces.
Half-life
Adults: 60 hours; children: about 30 hours.
Special Populations
Removed by hemodialysis; dosage adjustment may be necessary.
Stability
Storage
Oral
Capsules
Tight containers at 15–30°C.
Oral Solution
Tight, light-resistant containers at 20–25°C; avoid freezing.
Actions
-
Ethosuximide shares the actions of succinimide-derivative anticonvulsants.
-
Exact mechanism of anticonvulsant action not known.
-
Increases seizure threshold in the cortex and basal ganglia and reduces synaptic response to low-frequency repetitive stimulation.
-
Ethosuximide suppresses paroxysmal spike and wave activity of the EEG associated with lapses of consciousness common in absence seizures.
Advice to Patients
-
Importance of strictly adhering to prescribed directions for use and not altering the anticonvulsant regimen without first consulting with the clinician. Importance of instructing patients to read the patient information (medication guide) prior to initiating ethosuximide and each time the drug is refilled.
-
Risk of suicidality (anticonvulsants may increase risk of suicidal thoughts or actions in about 1 in 500 people). Importance of patients, family, and caregivers being alert to day-to-day changes in mood, behavior, and actions and immediately informing clinician of any new or worrisome behaviors (e.g., talking or thinking about wanting to hurt oneself or end one’s life, withdrawing from friends and family, becoming depressed or experiencing worsening of existing depression, becoming preoccupied with death and dying, giving away prized possessions).
-
Importance of not abruptly discontinuing therapy.
-
Importance of advising patients that a rash may be indicative of a serious medical event and to report such occurrences.
-
Importance of informing patients that ethosuximide may cause serious, even life-threatening blood cell abnormalities such as reduced red or white blood cells and that periodic blood counts should therefore be performed. Advise patients to promptly contact their clinician if signs and/or symptoms of such blood cell abnormalities or infection (e.g., sore throat, fever) develop.
-
Advise patients that drug may impair their ability to perform activities requiring mental alertness or physical coordination (e.g., driving a motor vehicle).
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and herbal products, as well as any concomitant illnesses.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed; advise pregnant women of possible risk to fetus. Importance of clinicians informing women about the existence of and encouraging enrollment in pregnancy registries (see Pregnancy under Cautions).
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
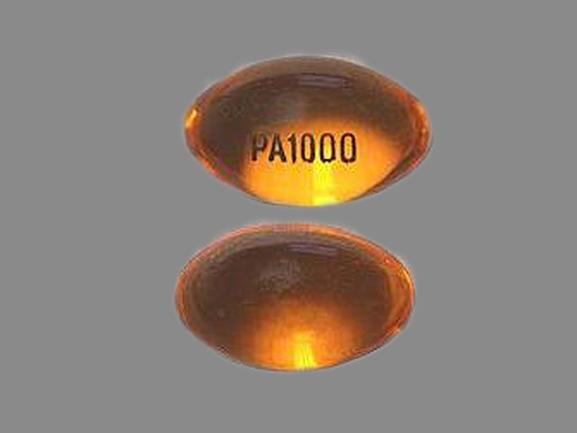
Oral |
Capsules |
250 mg* |
Ethosuximide Capsules |
|
|
Zarontin |
Pfizer |
|||
|
Solution |
250 mg/5 mL* |
Ethosuximide Solution |
||
|
Zarontin Solution |
Pfizer |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions July 2, 2018. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
More about ethosuximide
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (12)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: succinimide anticonvulsants
- Breastfeeding
- En español