Dulaglutide (Monograph)
Brand name: Trulicity
Drug class: Incretin Mimetics
Warning
- Risk of Thyroid C-Cell Tumors
-
Dulaglutide causes dose- and treatment duration-dependent thyroid C-cell tumors (adenomas and carcinomas) in male and female rats after lifetime exposure.
-
Unknown whether dulaglutide causes thyroid C-cell tumors, including medullary thyroid carcinoma (MTC), in humans, as relevance to humans has not been determined.
-
Contraindicated in patients with a personal or family history of MTC and in patients with multiple endocrine neoplasia syndrome type 2 (MEN 2).
Counsel patients regarding potential risk of MTC and inform them about symptoms of thyroid tumors.
Routine monitoring of serum calcitonin or use of thyroid ultrasound of uncertain value for early detection of MTC in patients receiving dulaglutide.
Introduction
Antidiabetic agent; long-acting glucagon-like peptide-1 (GLP-1) receptor agonist (incretin mimetic).
Uses for Dulaglutide
Type 2 Diabetes Mellitus
Glycemic Control
Used as an adjunct to diet and exercise to improve glycemic control in adults and pediatric patients ≥10 years of age with type 2 diabetes mellitus.
Used alone or as add-on therapy with metformin, the combination of metformin and a sulfonylurea, the combination of metformin and a thiazolidinedione, a sodium-glucose cotransporter 2 (SGLT2) inhibitor with or without metformin, basal insulin with or without metformin, and prandial insulin with or without metformin.
Current guidelines for the treatment of type 2 diabetes mellitus generally recommend metformin as first-line therapy in addition to lifestyle modifications in patients with recent-onset type 2 diabetes mellitus or mild hyperglycemia because of its well-established safety and efficacy (i.e., beneficial effects on glycosylated hemoglobin [hemoglobin A1c; HbA1c], weight, and cardiovascular mortality).
In patients with metformin contraindications or intolerance (e.g., risk of lactic acidosis, GI intolerance) or in selected other patients, some experts suggest that initial therapy with a drug from another class of antidiabetic agents (e.g., a GLP-1 receptor agonist, SGLT2 inhibitor, dipeptidyl peptidase-4 [DPP-4] inhibitor, sulfonylurea, thiazolidinedione, basal insulin) may be acceptable based on patient factors.
May need to initiate therapy with 2 agents (e.g., metformin plus another drug) in patients with high initial HbA1c (>7.5% or ≥1.5% above target). In such patients with metformin intolerance, some experts suggest initiation of therapy with 2 drugs from other antidiabetic drug classes with complementary mechanisms of action.
Consider early initiation of combination therapy for the treatment of type 2 diabetes mellitus to extend the time to treatment failure and more rapidly attain glycemic goals.
For patients with inadequate glycemic control on metformin monotherapy, consider patient comorbidities (e.g., atherosclerotic cardiovascular disease [ASCVD], established kidney disease, heart failure), hypoglycemia risk, impact on weight, cost, risk of adverse effects, and patient preferences when selecting additional antidiabetic agents for combination therapy.
Consider early introduction of insulin for severe hyperglycemia (e.g., blood glucose of ≥300 mg/dL or HbA1c >9–10%), especially if accompanied by catabolic manifestations (e.g., weight loss, hypertriglyceridemia, ketosis) or symptoms of hyperglycemia.
Experts recommend that patients with type 2 diabetes mellitus who have established (or are at a high risk for) ASCVD, established kidney disease, or heart failure receive a GLP-1 receptor agonist or SGLT2 inhibitor with demonstrated cardiovascular disease benefit. In patients with these comorbidities, consider GLP-1 receptor agonist or SGLT2 inhibitor therapy independently of patient's HbA1c.
In patients with type 2 diabetes mellitus and CKD, consider a GLP-1 receptor agonist or SGLT2 inhibitor shown to reduce the risk of CKD progression, cardiovascular events, or both, in addition to metformin therapy or in those in whom metformin cannot be used.
In patients on metformin monotherapy without established ASCVD or indicators of high ASCVD risk, heart failure, or CKD, base decision regarding addition of other antidiabetic agents on avoidance of adverse effects, cost, and individual patient factors.
Safety and efficacy not established in patients with a history of pancreatitis; consider other antidiabetic agents.
Not recommended for use in patients with severe GI disease, including severe gastroparesis.
Not indicated for the treatment of type 1 diabetes mellitus.
Reduction in Risk of Major Adverse Cardiovascular Events
Used to reduce the risk of major adverse cardiovascular events in adults with type 2 diabetes mellitus and established cardiovascular disease or multiple cardiovascular risk factors.
Beneficial Effects on Renal Function
Some experts suggest that use of a GLP-1 receptor agonist (e.g., dulaglutide, liraglutide, semaglutide) may reduce risk of progression of albuminuria, cardiovascular events, or both† [off-label] in patients with type 2 diabetes mellitus and CKD who are at increased risk for cardiovascular events.
Dulaglutide Dosage and Administration
General
Patient Monitoring
-
Perform regular monitoring (e.g., blood glucose determinations, HbA1c) to determine therapeutic response.
Administration
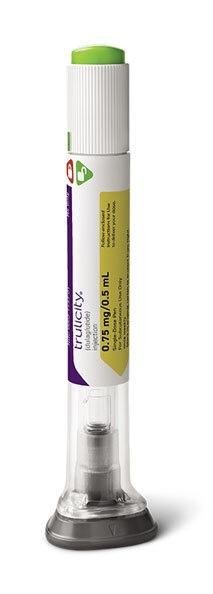
Administer by sub-Q injection using a prefilled injection pen.
If a dose is missed, administer it as soon as possible if there are at least 3 days (72 hours) until the next scheduled dose, followed by resumption of the regular weekly schedule. If less than 3 days remain before the next scheduled dose, skip the missed dose and resume the regular schedule with the next scheduled dose.
Administer dulaglutide and insulin as separate injections in patients receiving both medications; do not mix insulin and dulaglutide. May inject dulaglutide and insulin in the same body regions; do not administer injections adjacent to each other.
Sub-Q Administration
Administer by sub-Q injection once weekly, on the same day each week, at any time of day without regard to meals. If changing the day of weekly administration, allow at least 3 days to elapse between doses.
Administer into abdomen, thigh, or upper arm; rotate injection sites with each dose.
Dosage
Pediatric Patients
Type 2 Diabetes Mellitus
Sub-Q
Pediatric patients ≥10 years of age: Initially, 0.75 mg once weekly. If additional glycemic control is needed, increase to maximum recommended dosage of 1.5 mg once weekly after at least 4 weeks on the 0.75 mg dosage.
Adults
Type 2 Diabetes Mellitus
Sub-Q
Initially, 0.75 mg once weekly. May increase dosage to 1.5 mg once weekly for additional glycemic control.
If further glycemic conctrol is needed, increase dosage in 1.5-mg increments after at least 4 weeks on the current dosage. Maximum recommended dosage is 4.5 mg once weekly.
Special Populations
No special population dosage recommendations.
Use caution in patients with end-stage renal impairment.
Cautions for Dulaglutide
Contraindications
-
Personal or family history of MTC.
-
MEN 2.
-
Prior serious hypersensitivity to dulaglutide or any component in the formulation.
Warnings/Precautions
Warnings
Risk of Thyroid C-Cell Tumors
Thyroid C-cell tumors found in rats and mice receiving GLP-1 receptor agonists at clinically relevant exposures. Dulaglutide causes dose- and treatment duration-dependent thyroid C-cell tumors in male and female rats after lifetime exposure. Unknown whether dulaglutide causes thyroid C-cell tumors, including MTC, in humans; relevance to humans could not be ruled out by clinical or nonclinical studies.
Very elevated serum calcitonin values may suggest MTC; such values generally exceed 50 ng/mL in patients with MTC. Uncertain value of routine monitoring of serum calcitonin; if serum calcitonin is found elevated, refer patient to endocrinologist for further evaluation. Role of monitoring serum calcitonin concentrations or thyroid ultrasound examinations for the purpose of early detection of MTC unknown. Refer patients with thyroid nodules noted on physical examination or neck imaging to an endocrinologist.
Sensitivity Reactions
Hypersensitivity Reactions
Serious hypersensitivity reactions (severe urticaria, systemic rash, facial edema, lip swelling), including anaphylaxis and angioedema, reported. Discontinue dulaglutide and treat promptly according to standard of care if hypersensitivity reaction occurs; monitor patient until signs and symptoms have resolved. Exercise caution if used in patients with history of anaphylaxis or angioedema to other GLP-1 receptor agonists.
Other Warnings and Precautions
Risks During General Anesthesia and Deep Sedation
GLP-1 agonists are associated with adverse GI effects such as nausea, vomiting, and delayed gastric emptying.
Delayed gastric emptying from GLP-1 agonists can increase the risk of regurgitation and pulmonary aspiration of gastric contents during general anesthesia and deep sedation.
The American Society of Anesthesiologists (ASA) Task Force on Preoperative Fasting has issued a consensus-based guidance for management of GLP-1 receptor agonists prior to elective surgery. The task force suggests that for patients on daily GLP-1 agonist dosing (irrespective of indication, dose, or type of surgery), consider holding the drug on the day of procedure/surgery. For patients on weekly dosing (irrespective of indication, dose, or type of surgery), consider holding the GLP-1 agonist a week prior to procedure/surgery. If GLP-1 agonists prescribed for diabetes management are held for longer than the dosing schedule, consider consulting an endocrinologist for bridging the antidiabetic therapy to avoid hyperglycemia.
For patients requiring urgent or emergent procedures, the task force states to proceed and treat the patient as ‘full stomach’ and manage accordingly.
Pancreatitis and Pancreatic Precancerous Changes
Acute pancreatitis reported during clinical trials.
Observe patients carefully for signs and symptoms of pancreatitis, including persistent severe abdominal pain, sometimes radiating to the back, which may or may not be accompanied by vomiting.
If pancreatitis is suspected, promptly discontinue dulaglutide. If pancreatitis is confirmed, do not restart dulaglutide.
Efficacy and safety not established in patients with a history of pancreatitis; consider other antidiabetic agents in such patients.
Use with Drugs Known to Cause Hypoglycemia
Patients receiving dulaglutide in combination with an insulin secretagogue (e.g., sulfonylurea) or insulin have an increased risk of hypoglycemia. A lower dosage of the concomitant insulin secretagogue or insulin may be required to reduce the risk of hypoglycemia.
Renal Effects
Acute renal failure and worsening of chronic renal failure (sometimes requiring hemodialysis) reported with GLP-1 receptor agonists during postmarketing experience. Some patients did not have known underlying renal disease. Most events occurred in patients experiencing nausea, vomiting, diarrhea, or dehydration. Because such adverse GI effects may worsen renal function, use caution when initiating dulaglutide or escalating dosage in patients with renal impairment.
GI Effects
Adverse GI effects, sometimes severe, associated with dulaglutide use.
Data lacking on use of dulaglutide in patients with severe GI disease, including severe gastroparesis; use not recommended in such patients.
Diabetic Retinopathy Complications
In a clinical study, more diabetic retinopathy complications occurred in patients receiving dulaglutide compared with those receiving placebo. Rapid improvement in glycemic control has been associated with a temporary worsening of diabetic retinopathy. Monitor patients with a history of diabetic retinopathy for progression of this condition.
Acute Gallbladder Disease
Acute events of gallbladder disease have been reported with GLP-1 receptor agonist use, including dulaglutide.
If cholelithiasis is suspected, gallbladder studies and appropriate clinical follow-up are indicated.
Immunogenicity
Anti-drug antibodies, including neutralizing antibodies, detected in adults and pediatric patients receiving dulaglutide. Such antibodies did not appear to have clinically significant effects on pharmacokinetics, pharmacodynamics, safety, or effectiveness of dulaglutide in adults. Incidence was too low to determine whether antibodies have any clinical effects in pediatric patients.
Specific Populations
Pregnancy
Data lacking on use of dulaglutide in pregnant women. Reproduction studies in rats and rabbits using dulaglutide have demonstrated decreased growth and teratogenic effects. Use during pregnancy only if potential benefit justifies possible risk to the fetus.
Lactation
Data lacking on the presence of dulaglutide in milk in humans, effects on breast-fed infant, or effects on milk production.
Consider developmental and health benefits of breast-feeding along with mother's clinical need for dulaglutide and any potential adverse effects on breast-fed infant from the drug or underlying maternal condition.
Pediatric Use
Safety and efficacy established in patients ≥10 years of age with type 2 diabetes mellitus.
Higher incidence of injection-site reactions reported in pediatric patients compared with adults.
Safety and efficacy not established in pediatric patients <10 years of age.
Geriatric Use
No substantial differences in safety and efficacy relative to younger adults.
Hepatic Impairment
Limited experience in patients with hepatic impairment; use caution. No clinically important changes in systemic exposure in patients with hepatic impairment.
Renal Impairment
No substantial differences in safety and efficacy observed in patients with mild, moderate, or severe renal impairment. Limited experience in patients with end-stage renal disease (ESRD); use caution.
Monitor renal function in patients with renal impairment experiencing severe adverse GI effects.
Common Adverse Effects
Most common adverse reactions (≥5%): nausea, diarrhea, vomiting, abdominal pain, decreased appetite.
Drug Interactions
Insulin Secretagogues
When initiating dulaglutide, consider reducing the dose of concomitantly administered insulin secretagogues (e.g., sulfonylureas) or insulin to reduce the risk of hypoglycemia.
Orally Administered Drugs
Dulaglutide delays gastric emptying in a dose-dependent manner. Possible altered rate and extent of absorption of concomitantly administered oral drugs;.
Monitor concentrations of oral drugs with a narrow therapeutic index (e.g., warfarin) when such drugs are administered concomitantly with dulaglutide.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Acetaminophen |
No substantial change in acetaminophen peak plasma concentration or overall AUC |
No dosage adjustment necessary |
|
Atorvastatin |
Decreased AUC and peak plasma concentration of atorvastatin |
Clinical relevance not known; no dosage adjustment necessary |
|
Digoxin |
No substantial change in digoxin peak plasma concentration or overall AUC |
No dosage adjustment necessary |
|
Lisinopril |
No substantial change in lisinopril peak plasma concentration or overall AUC |
No dosage adjustment necessary |
|
Metformin |
No substantial change in metformin peak plasma concentration or overall AUC |
No dosage adjustment necessary |
|
Metoprolol |
No substantial change in metoprolol peak plasma concentration or overall AUC |
No dosage adjustment necessary |
|
Hormonal contraceptives, oral |
No substantial change in ethinyl estradiol or norelgestromin peak plasma concentration or overall AUC |
No dosage adjustment necessary |
|
Sitagliptin |
Increased dulaglutide AUC and peak plasma concentration; no change in sitagliptin AUC and peak plasma concentration |
No dosage adjustment of either drug necessary |
|
Warfarin |
No change in overall AUC of R- or S-warfarin |
No dosage adjustment necessary |
Dulaglutide Pharmacokinetics
Absorption
Bioavailability
Mean absolute bioavailability 65 and 47% following 0.75- and 1.5-mg doses, respectively.
Peak plasma dulaglutide concentration at steady state achieved in 24–72 hours (median 48 hours). Steady-state concentrations achieved at 2–4 weeks with once-weekly administration.
Special Populations
In patients with mild, moderate, or severe hepatic impairment, AUC decreased by 23, 33, or 21%, respectively.
In patients with mild, moderate, or severe renal impairment or ESRD, AUC increased by 20, 28, 14, or 12%, respectively.
Elimination
Metabolism
Presumed to be metabolized into component amino acids by general protein catabolism pathways. Resistant to degradation by dipeptidyl peptidase-4 (DPP-4).
Half-life
Approximately 5 days.
Stability
Storage
Parenteral
Injection
2–8°C in original carton; do not freeze.
After dispensing, may be stored at room temperature up to 30°C for up to 14 days.
Actions
-
Two disulfide-linked chains, each containing a glucagon-like peptide (GLP-1) analog molecule covalently fused to the Fc portion of a modified human IgG4 heavy chain by a small peptide linker; resistant to degradation by dipeptidyl peptidase-4 (DPP-4) due to structural modifications. Each GLP-1 analog is 90% homologous to human GLP-1 (7–37).
-
Increases insulin release in the presence of elevated glucose concentrations.
-
Suppresses glucagon secretion.
-
Delays gastric emptying, reducing postprandial glucose concentrations.
Advice to Patients
-
Importance of informing patients that dulaglutide causes benign and malignant thyroid C-cell tumors in rats and that relevance of this finding to humans is unknown. Patients should report symptoms of thyroid tumors (e.g., a lump in the neck, persistent hoarseness, dysphagia, dyspnea) to their clinician.
-
Importance of informing patients about the possibility of acute pancreatitis with dulaglutide therapy. Importance of patients informing clinicians if they have a history of pancreatitis. Importance of informing patients about signs and symptoms of pancreatitis, including persistent severe abdominal pain sometimes radiating to the back that may or may not be accompanied by vomiting; importance of patients discontinuing dulaglutide and promptly notifying clinician if such signs or symptoms occur.
-
Importance of informing patients of risk of hypoglycemia, particularly if concomitant therapy with an insulin secretagogue (e.g., sulfonylurea) or insulin is used. Importance of reviewing signs, symptoms, and management of hypoglycemia.
-
Importance of informing patients of possibility of hypersensitivity reactions. Patients should be instructed to discontinue dulaglutide and promptly seek medical advice if symptoms of hypersensitivity occur.
-
Inform patients of the potential risk for cholelithiasis or cholecystitis. Instruct patients to contact their physician if cholelithiasis or cholecystitis is suspected for appropriate clinical follow-up.
-
Importance of informing patients of potential risk of adverse GI effects and possibility of dehydration due to such adverse effects; advise patients to take precautions to avoid fluid depletion. Importance of informing patients of potential risk of worsening renal function, which may require dialysis in some cases.
-
Importance of informing patients to contact their clinician if they experience changes in vision during treatment with dulaglutide.
-
Importance of patients reading the manufacturer's instructions for use before starting dulaglutide therapy. Importance of instructing patients regarding proper use, storage, and disposal of injection pen. After dispensing, store pens in refrigerator, or at room temperature for up to 14 days; protect injection pens from direct heat and light and do not freeze.
-
Importance of informing patients not to take an extra dose of dulaglutide to make up for a missed dose. If a dose is missed, patients should take the dose as soon as possible if there are at least 3 days (72 hours) until the next dose; the next dose can be taken on their usual weekly day. If there are less than 3 days until the next dose, the missed dose should be skipped and patients should take the next dose on their usual weekly day.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses (e.g., pancreatitis, diabetic retinopathy, GI disease).
-
Inform patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Injection, for subcutaneous use only |
0.75 mg/0.5 mL |
Trulicity (available as prefilled single-dose injection pen) |
Lilly |
|
1.5 mg/0.5 mL |
Trulicity (available as prefilled single-dose injection pen) |
Lilly |
||
|
3 mg/0.5 mL |
Trulicity (available as prefilled single-dose injection pen) |
Lilly |
||
|
4.5 mg/0.5 mL |
Trulicity (available as prefilled single-dose injection pen) |
Lilly |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions October 16, 2023. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Biological Products Related to dulaglutide
Find detailed information on biosimilars for this medication.
Frequently asked questions
- Trulicity vs Ozempic: Which is right for you?
- Does Trulicity cause weight loss?
- Does Trulicity need to be refrigerated?
- Trulicity and diet: What foods should you avoid?
- How do you use/inject Trulicity?
- Can Trulicity be injected cold?
- Can Trulicity be used with insulin?
- Is Trulicity a form of insulin?
- How does Trulicity work?
More about dulaglutide
- Check interactions
- Compare alternatives
- Reviews (994)
- Latest FDA alerts (2)
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: GLP-1 Agonists (Incretin Mimetics)
- Breastfeeding
- En español