Dronedarone (Monograph)
Brand name: Multaq
Drug class: Class III Antiarrhythmics
VA class: CV300
Chemical name: N-[2-butyl-3-[4-[3-(dibutylamino)propoxy]benzoyl]-5-benzofuranyl]-methanesulfonamide monohydrochloride
Molecular formula: C31H44N2O5S•HCl
CAS number: 141625-93-6
Warning
Risk Evaluation and Mitigation Strategy (REMS):
FDA approved a REMS for dronedarone to ensure that the benefits outweigh the risks. However, FDA later rescinded REMS requirements. See https://www.accessdata.fda.gov/scripts/cder/rems/.
Warning
-
Contraindicated in patients with NYHA class IV heart failure or symptomatic heart failure with recent decompensation requiring hospitalization.1 (See New-Onset or Worsening Heart Failure under Cautions.)
-
In the ANDROMEDA study in patients with severe heart failure requiring recent hospitalization or referral to a specialized heart failure clinic for worsening symptoms, dronedarone therapy was associated with a greater than twofold increase in mortality rate relative to placebo;1 4 do not use dronedarone in such patients.1
-
Contraindicated in patients with permanent atrial fibrillation; doubles the risk of cardiovascular death and heart failure in such patients.1 9 35 (See Warnings under Cautions.)
Introduction
Predominantly Class III antiarrhythmic agent;5 6 7 also appears to exhibit activity in each of the 4 Vaughan-Williams antiarrhythmic classes.1 5 6 8
Uses for Dronedarone
Supraventricular Tachyarrhythmias
Reduction of risk of hospitalization for atrial fibrillation in patients in sinus rhythm who have a history of paroxysmal or persistent atrial fibrillation.1 9
Do not use in patients with permanent atrial fibrillation (i.e., patients in whom normal sinus rhythm will not or cannot be restored); increased risk of cardiovascular events and death in such patients.1 9 29 30 32 33 35 (See Warnings.)
Less effective than amiodarone in preventing recurrence of atrial fibrillation but appears to have an improved safety profile (based on short-term data).4 5 8 9 14 16 19 24 Long-term data and experience needed to elucidate relative safety and tolerability of dronedarone versus amiodarone because of some late-onset adverse effects of amiodarone (e.g., pulmonary toxicity).6 8 14 16 18 19
Efficacy of retreatment with dronedarone in patients who relapse after initial successful treatment or in those who fail therapy with amiodarone not established.17 21
Individualize treatment of atrial fibrillation/flutter based on relative benefits and risks of various therapies (e.g., rhythm versus rate control, nondrug therapies such as ablation and pacemaker implantation), patient age, and patient preference and tolerance of the arrhythmia.15 17 18 20 21 22 23 24 26
Related/similar drugs
diltiazem, Xarelto, digoxin, rivaroxaban, flecainide, sotalol, propafenone
Dronedarone Dosage and Administration
General
REMS
-
FDA-required Risk Evaluation and Mitigation Strategy (REMS) implemented to assist healthcare professionals in identifying appropriate patients to receive dronedarone and ensure safe use while minimizing risk.10 11 12
-
REMS program consists of educational materials for healthcare professionals and patients, including patient medication guide.1 10 11 12
-
For additional information, consult the Multaq website at [Web].10
Administration
Oral Administration
Administer orally twice daily with morning and evening meals (to enhance bioavailability).1 (See Food under Pharmacokinetics.)
Dosage
Available as dronedarone hydrochloride; dosage expressed in terms of dronedarone.1
Adults
Supraventricular Tachyarrhythmias
Oral
400 mg twice daily for reduction of risk of hospitalization for atrial fibrillation in selected patients in sinus rhythm with a history of paroxysmal or persistent atrial fibrillation.1
Must discontinue class I or III antiarrhythmic agents and drugs that are potent CYP3A inhibitors prior to initiating dronedarone.1 9 (See Contraindications under Cautions and also see Interactions.)
Special Populations
The manufacturer states that no dosage other than 400 mg twice daily of dronedarone is recommended for any population at this time.9
Hepatic Impairment
No dosage adjustment required in patients with moderate hepatic impairment.1 Contraindicated in patients with severe hepatic impairment.1 (See Hepatic Impairment under Cautions.)
Renal Impairment
No dosage adjustment required.1
Cautions for Dronedarone
Contraindications
-
Permanent atrial fibrillation (patients in whom normal sinus rhythm will not or cannot be restored).1
-
Symptomatic heart failure with NYHA class IV symptoms or recent decompensation requiring hospitalization.1
-
Second- or third-degree AV block or sick sinus syndrome (except in patients with a functioning pacemaker).1
-
Bradycardia (<50 beats/minute).1
-
QT interval corrected for rate, Bazett’s formula (QTc) of ≥500 msec or PR interval >280 msec.1 9 (See Prolongation of QT Interval under Cautions.)
-
Concomitant use of potent inhibitors of CYP3A (e.g., clarithromycin, cyclosporine, itraconazole, ketoconazole, nefazodone, ritonavir, telithromycin, voriconazole).1 (See Interactions.)
-
Concomitant use with drugs or herbal supplements that prolong the QT interval and may increase the risk of torsades de pointes (e.g., class I or III antiarrhythmic agents, phenothiazine antipsychotics, tricyclic antidepressants, certain oral macrolides (e.g., erythromycin).1 9
-
Liver toxicity related to previous use of amiodarone.1 (See Severe Hepatic Injury under Cautions.)
-
Severe hepatic impairment.1 (See Hepatic Impairment under Cautions.)
-
Women who are or may become pregnant.1 (See Fetal/Neonatal Morbidity and Mortality under Cautions.)
-
Nursing women.1
Warnings/Precautions
Warnings
Cardiovascular Death in Patients with Decompensated Heart Failure
Contraindicated in patients with NYHA class IV heart failure or symptomatic heart failure and recent decompensation requiring hospitalization; twofold increase in cardiovascular death in such patients.1 33
Cardiovascular Death and Heart Failure in Patients with Permanent Atrial Fibrillation
Offers no benefit and is contraindicated in patients with permanent atrial fibrillation (i.e., those who cannot or will not be converted to normal sinus rhythm) due to doubling of risk of cardiovascular death (principally due to arrhythmia) and heart failure.1 33
Monitor heart rate via ECG at least every 3 months.1 33 Discontinue therapy in patients who have atrial fibrillation, or perform cardioversion if clinically indicated.1 33
Increased Risk of Stroke in Patients with Permanent Atrial Fibrillation
Associated with increased risk of stroke in patients with permanent atrial fibrillation, particularly in first 2 weeks of therapy.1 33 Initiate only in patients in sinus rhythm who are receiving appropriate antithrombotic therapy.1 33
Other Warnings and Precautions
New-Onset or Worsening Heart Failure
New-onset or worsening heart failure reported.1 If heart failure develops or worsens, discontinue dronedarone therapy in patients receiving dronedarone during postmarketing experience.1
Contraindicated in patients with NYHA class IV heart failure or heart failure with recent decompensation requiring hospitalization.1 (See Boxed Warning.)
Severe Hepatic Injury
Severe hepatic injury reported with dronedarone therapy.1 28 Acute hepatic failure requiring liver transplantation reported in at least 2 patients; in both cases, explanted liver showed evidence of extensive hepatocellular necrosis.28
Consider periodic monitoring of serum hepatic enzymes, especially during first 6 months of therapy.1 28
If hepatic injury suspected (e.g., anorexia, nausea, vomiting, fever, malaise, fatigue, right upper quadrant pain, jaundice, dark urine, itching), discontinue dronedarone therapy promptly and assess AST, ALT, alkaline phosphatase, and bilirubin values; initiate appropriate therapy if hepatic injury found.1 28
Do not reinitiate dronedarone therapy in patients who experience hepatic injury without another explanation for such injury.1 28
Hypokalemia and Hypomagnesemia
Possible hypokalemia or hypomagnesemia with concomitant use of potassium-depleting diuretics.1 Ascertain that serum potassium and magnesium concentrations are within normal range prior to initiation of dronedarone; maintain within normal range during therapy.1 9 24
Prolongation of QT Interval
Moderate prolongation of QTc interval reported; QTc interval increased by an average of about 10 msec, however, greater prolongation reported.1 Discontinue dronedarone if QTc interval is ≥500 msec.1 (See Contraindications under Cautions.)
Increased Scr
Small increases in Scr (about 0.1 mg/dL) reported following dronedarone treatment initiation; result of inhibition of creatinine tubular secretion.1 5 13 16
Larger increases in Scr after dronedarone initiation also reported.1 Creatinine elevation has rapid onset and reaches plateau after 7 days.1 Increased BUN also reported.1 Effects generally reversible upon drug discontinuance.1
Monitor renal function periodically.
Fetal/Neonatal Morbidity and Mortality
May cause fetal harm; teratogenicity demonstrated in animals at dosages equivalent to those used in humans.1
Avoid pregnancy during therapy.1 Counsel women of childbearing potential (i.e., premenopausal women who have not undergone hysterectomy or oophorectomy) regarding appropriate contraceptive choices; such women must use effective contraception during dronedarone therapy.1 If dronedarone used during pregnancy or if patient becomes pregnant while receiving the drug, apprise of potential fetal hazard.1
Contraindicated in women who are or may become pregnant.1
Specific Populations
Pregnancy
Category X.1 (See Fetal/Neonatal Morbidity and Mortality under Cautions.)
Lactation
Dronedarone and its metabolites distributed into milk in rats; not known whether distributed into milk in humans.1 Discontinue nursing or the drug.1 Contraindicated in nursing women.1
Pediatric Use
Safety and efficacy not established in children or adolescents <18 years of age.1
Geriatric Use
No substantial differences in safety and efficacy relative to those in younger adults.1 (See Special Populations under Pharmacokinetics.)
Hepatic Impairment
Not studied in patients with severe hepatic impairment; limited clinical experience available in patients with moderate hepatic impairment.1 Severe liver injury reported rarely with dronedarone therapy.28 (See Severe Hepatic Injury under Cautions.) Contraindicated in patients with severe hepatic impairment.1 (See Special Populations under Pharmacokinetics.)
Renal Impairment
No dosage adjustment required because dronedarone undergoes minimal renal excretion.1 (See Special Populations and also see Elimination Route under Pharmacokinetics.)
Common Adverse Effects
Early increases in Scr (increase of ≥10%),1 prolonged QTc interval,1 diarrhea,1 2 14 asthenic conditions,1 nausea,1 2 skin reactions (e.g., rash [generalized, macular, maculopapular, erythematous], pruritus, eczema, dermatitis, allergic dermatitis),1 2 abdominal pain,1 bradycardia,1 2 vomiting,1 dyspeptic manifestations.1 (See Prolongation of QT Interval and Increased Scr under Cautions.)
Drug Interactions
Metabolized mainly by CYP isoenzyme 3A.1
Moderate inhibitor of CYP isoenzymes 3A and 2D6; does not appear to substantially inhibit CYP isoenzymes 1A2, 2C9, 2C19, 2C8, or 2B6.1
May inhibit P-glycoprotein transport system.1
Dronedarone or metabolites are weak inhibitors of organic cation transporter (OCT1), organic anion transporting polypeptide (OATP1B1, OATP1B3), and organic anion transporter (OAT3) in vitro.1
Drugs Affecting Hepatic Microsomal Enzymes
Potent inhibitors of CYP3A: Pharmacokinetic interaction (increased peak plasma concentrations of and exposure to dronedarone).1 Concomitant use contraindicated.1
Inducers of CYP3A: Potential pharmacokinetic interaction (substantially decreased exposure to dronedarone).1 Avoid concomitant use.1
Drugs Metabolized by Hepatic Microsomal Enzymes
Substrates of CYP3A: Potential pharmacokinetic interaction (possible increased plasma concentrations of the CYP3A substrate).1 9 25 Monitor plasma concentrations and appropriately adjust dosage of CYP3A substrates with a narrow therapeutic index when administered orally.1 9 Some clinicians state that dronedarone should be used with caution in patients receiving drugs with a narrow therapeutic index that are metabolized by CYP3A4.25
Substrates of CYP2D6: Potential pharmacokinetic interaction (possible increased exposure to the CYP2D6 substrate).1
Drugs that Prolong the QT Interval
Pharmacologic interaction (potential risk of torsades de pointes-type ventricular tachycardia) with drugs that prolong the QT interval; concomitant use contraindicated.1 9 (See Contraindications under Cautions.)
Drugs Affected by the P-glycoprotein Transport System
Potential pharmacokinetic interaction (increased exposure to substrates of P-glycoprotein transport system).1 Some clinicians state that dronedarone should be used with caution in patients receiving drugs with a narrow therapeutic index that are affected by the P-glycoprotein transport system.25
Specific Drugs and Foods
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Antiarrhythmic agents, class I or III (e.g., amiodarone, disopyramide, dofetilide, flecainide, propafenone, quinidine, sotalol) |
Potential risk of torsades de pointes-type ventricular tachycardia due to QT-interval prolongation1 9 |
|
|
Anticoagulants, oral (e.g., warfarin) |
Slightly increased exposure to S-warfarin in healthy individuals; no change in exposure to R-warfarin or clinically important increases in INR1 No excess risk of bleeding observed with concomitant use of dronedarone and oral anticoagulants in patients with atrial fibrillation/flutter; cases of increased INR with/without bleeding reported during postmarketing experience1 |
Monitor INR according to manufacturers’ labeling for warfarin1 |
|
Antidepressants, SSRI |
Possible increased exposure to SSRI1 |
|
|
Antidepressants, tricyclic |
Potential risk of torsades de pointes-type ventricular tachycardia due to QT-interval prolongation1 Possible increased exposure to tricyclic antidepressants1 |
Concomitant use contraindicated1 |
|
β-Adrenergic blocking agents (e.g., metoprolol, propranolol) |
Increased incidence of bradycardia1 Increased exposure to propranolol and metoprolol1 |
Use lower initial dosage of the β-adrenergic blocking agent and increase dosage of β-adrenergic blocker only if well tolerated as documented by ECG1 9 |
|
Calcium-channel blocking agents (e.g., diltiazem, nifedipine, verapamil) |
Calcium-channel blocking agents with depressant effects on the sinus and AV nodes may potentiate the conduction effects of dronedarone1 Dronedarone increases exposure to verapamil, diltiazem, and nifedipine; verapamil and diltiazem increase exposure to dronedarone1 |
Use lower initial dosage of the calcium-channel blocking agent and increase dosage of calcium-channel blocker only if well tolerated as documented by ECG1 9 |
|
Carbamazepine |
Substantially decreased exposure to dronedarone due to CYP3A induction1 |
Avoid concomitant use1 |
|
Cyclosporine |
Increased peak plasma concentrations of and exposure to dronedarone1 |
Concomitant use contraindicated1 |
|
Dabigatran |
Increased exposure to dabigatran1 |
|
|
Digoxin |
Possible potentiation of electrophysiologic effects of dronedarone (e.g., decreased AV node conduction)1 Increased digoxin concentrations and exposure1 Increased incidence of GI disorders1 |
When initiating dronedarone therapy, reassess need for continued digoxin therapy; discontinue digoxin or reduce digoxin dosage by 50%1 Monitor serum digoxin concentrations; close observation for signs of digoxin toxicity recommended1 |
|
Grapefruit juice |
Increased peak plasma concentrations of and exposure to dronedarone1 |
|
|
HMG-CoA reductase inhibitors (statins) |
Increased exposure to simvastatin and simvastatin acid1 |
Avoid simvastatin dosages >10 mg daily Consult respective statin manufacturer’s labeling for specific recommendations regarding concomitant use1 |
|
Itraconazole |
Increased peak plasma concentrations of and exposure to dronedarone1 |
Concomitant use contraindicated1 |
|
Ketoconazole |
Increased peak plasma concentrations of and exposure to dronedarone1 |
Concomitant use contraindicated1 |
|
Losartan |
No losartan dosage adjustment required1 |
|
|
Macrolides (e.g., clarithromycin, erythromycin, telithromycin) |
Clarithromycin, telithromycin: Increase exposure to and peak plasma concentrations of dronedarone1 Certain oral macrolides (e.g., erythromycin): Potential risk of torsades de pointes-type ventricular tachycardia due to QT-interval prolongation1 9 |
Clarithromycin, telithromycin, and certain oral macrolides (e.g., erythromycin): Concomitant use contraindicated1 |
|
Metformin |
No metformin dosage adjustment required1 |
|
|
Nefazodone |
Increased peak plasma concentrations of and exposure to dronedarone1 |
Concomitant use contraindicated1 |
|
Omeprazole |
No omeprazole dosage adjustment required1 |
|
|
Oral contraceptives |
No dosage adjustments for ethinyl estradiol or levonorgestrel required1 |
|
|
Pantoprazole |
No dronedarone dosage adjustment required1 |
|
|
Phenobarbital |
Substantially decreased exposure to dronedarone due to CYP3A induction1 |
Avoid concomitant use1 |
|
Phenothiazines |
Potential risk of torsades de pointes-type ventricular tachycardia due to QT-interval prolongation1 9 |
Concomitant use contraindicated1 |
|
Phenytoin |
Substantially decreased exposure to dronedarone due to CYP3A induction1 |
Avoid concomitant use1 |
|
Potassium-depleting diuretics |
Possible hypokalemia or hypomagnesemia1 |
Ascertain that serum potassium and magnesium concentrations are within normal range prior to initiation of dronedarone; maintain within normal range during therapy1 |
|
Rifampin |
Substantially decreased exposure to dronedarone due to CYP3A induction1 |
Avoid concomitant use1 |
|
Ritonavir |
Increased peak plasma concentrations of and exposure to dronedarone1 |
Concomitant use contraindicated1 |
|
St. John’s wort |
Substantially decreased exposure to dronedarone due to CYP3A induction1 |
Avoid concomitant use1 |
|
Sirolimus |
Possible substantial increase in plasma concentrations of sirolimus1 |
Monitor sirolimus concentrations and adjust dosage as needed1 If concurrent administration cannot be avoided, consider reducing sirolimus dosage by 50–75% prior to dronedarone initiation; monitor trough sirolimus concentrations regularly (possibly even daily) during titration phase25 |
|
Tacrolimus |
Possible substantial increase in plasma concentrations of tacrolimus1 |
Monitor tacrolimus concentrations and adjust dosage as needed1 |
|
Theophylline |
No theophylline dosage adjustment required1 |
|
|
Voriconazole |
Increased peak plasma concentrations of and exposure to dronedarone1 |
Concomitant use contraindicated1 |
Dronedarone Pharmacokinetics
Absorption and Distribution
Bioavailability
Low systemic bioavailability; undergoes first-pass metabolism.1 Absolute bioavailability about 4% when administered without food.1
Steady-state concentrations achieved within 4–8 days following repeated oral administration of dronedarone 400 mg twice daily.1
Food
Food increases bioavailability; bioavailability approximately 15% when administered with a high-fat meal.1
Peak plasma concentrations of dronedarone and N-debutyl metabolite reached within 3–6 hours following oral administration with food.1
Special Populations
Exposure to dronedarone increased by 23% in patients ≥65 years of age compared with that in younger adults.1 (See Geriatric Use under Cautions.)
Mean exposure to dronedarone increased by 1.3-fold in patients with moderate hepatic impairment compared with individuals with normal hepatic function; mean exposure to N-debutyl metabolite decreased by about 50%.1
Pharmacokinetics not studied in patients with severe hepatic impairment.1 (See Hepatic Impairment under Cautions.)
No apparent differences in pharmacokinetics observed in healthy individuals with mild or moderate renal impairment versus those with normal renal function, or in patients with atrial fibrillation and mild to severe renal impairment versus those with normal renal function.1 9
Exposure to dronedarone averages 30% higher in women than in men.1
Pharmacokinetic differences related to race not formally studied.1 However, based on a cross-study comparison, exposure to dronedarone twofold higher in Asian men (of Japanese ancestry) than in Caucasian men following single-dose administration of dronedarone 400 mg.1
Distribution
Extent
Dronedarone and its metabolites distributed into milk in rats; not known whether distributed into human milk.1
Plasma Protein Binding
Dronedarone and N-debutyl metabolite are >98% bound to plasma proteins (mainly albumin); binding not saturable.1
Elimination
Metabolism
Extensively metabolized, mainly by CYP3A.1
Initial metabolic pathway includes N-debutylation to form active N-debutyl metabolite, oxidative deamination to form inactive propanoic acid metabolite, and direct oxidation.1 Monoamine oxidase contributes to metabolism of active metabolite.1 Metabolites further metabolized to >30 uncharacterized metabolites.1 N-debutyl metabolite exhibits pharmacodynamic activity; only up to one-third as potent as dronedarone.1
Elimination Route
Excreted in urine (6%) and in feces (84%) mainly as metabolites; no unchanged drug excreted in urine.1
Half-life
13–19 hours following IV administration.1
Stability
Storage
Oral
Tablets
25°C (may be exposed to 15–30°C).1
Actions
-
Mechanism of antiarrhythmic action not fully elucidated; exact contribution of activities in each of the 4 Vaughan-Williams antiarrhythmic classes to the clinical effect of the drug unknown.1 5
-
Benzofuran derivative structurally related to amiodarone, but with structural modifications that include removal of the iodine group and addition of a methane-sulfonyl group.1 2 3 5 6 7 8 16
-
Removal of the iodine group intended to reduce risk of nontarget organ (e.g., thyroid, pulmonary) adverse effects associated with amiodarone therapy; addition of the methane-sulfonyl group aimed at reducing lipophilicity, decreasing risk of neurotoxic adverse effects, and shortening half-life of dronedarone.2 3 5 6 8 16
-
Electrophysiologic profile similar to amiodarone, but with different relative effects on individual ion channels.2 3 4 5 6
-
Prolongs action potential duration (APD) mainly by inhibition of potassium channels, including transmembrane delayed rectifier, ultrarapid delayed rectifier, inward rectifier, and transient outward potassium currents.5 6
-
Inhibits sodium currents (at rapid pacing rates), calcium channels and slow L-type calcium currents, and demonstrates noncompetitive, antiadrenergic (α- and β-blocking) activity.5 6 8 16
-
Prolongs PR interval and slows sinus rate by prolonging atrial and ventricular refractory periods.1 8
-
Produces a dose-dependent increase in PR interval and a moderate prolongation of the QTc interval similar to amiodarone.1 5 8
Advice to Patients
-
Importance of instructing patients to carefully read the manufacturer’s patient information (medication guide) before initiating therapy and each time the prescription is refilled.1 (See REMS.)
-
Importance of patients not taking dronedarone if they have signs and symptoms of heart failure that recently worsened or required hospitalization, or if they have severe heart failure, because of an increased risk of death.1 Importance of informing clinician if signs or symptoms of heart failure (e.g., weight gain, dependent edema, increasing shortness of breath) occur during dronedarone treatment.1
-
Risk of hepatic injury, including life-threatening hepatic failure.1 Importance of patients not taking dronedarone if they have severe hepatic injury or had hepatic injury after using amiodarone.1 Importance of advising patients to immediately report symptoms suggesting hepatic injury (e.g., anorexia, nausea, vomiting, fever, malaise, fatigue, right upper quadrant pain or discomfort, jaundice, dark urine, itching).1 28
-
Importance of patients not taking dronedarone if they have permanent atrial fibrillation.1 Importance of patients informing clinicians immediately if they notice an irregular pulse (a sign of atrial fibrillation) during treatment with dronedarone.1
-
Importance of advising patients to avoid grapefruit juice while taking dronedarone.1
-
Importance of women informing clinicians immediately if they are or plan to become pregnant or plan to breast-feed; necessity of advising women to avoid pregnancy and breast-feeding during dronedarone therapy.1 9 Necessity of advising women of childbearing potential to use an effective method of contraception while receiving therapy and importance of advising these patients regarding appropriate contraceptive choices (taking into consideration their underlying medical conditions and lifestyle preferences).1 If pregnancy occurs, advise patient of risk to the fetus.1
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and herbal supplements (e.g., St. John’s wort), as well as any concomitant illnesses (e.g., heart failure, rhythm disturbance other than atrial fibrillation/flutter, uncorrected hypokalemia).1
-
Importance of taking dronedarone exactly as prescribed (e.g., with meals).1 Importance of advising patients that if a dose of dronedarone is missed, the next dose should be taken at the regularly scheduled time; the dose should not be doubled.1
-
Importance of informing patients of other important precautionary information.1 (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
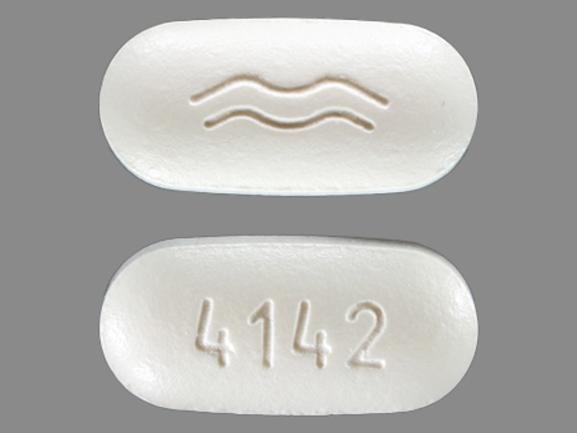
Oral |
Tablets, film-coated |
400 mg (of dronedarone) |
Multaq |
Sanofi-Aventis |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions June 2, 2016. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
References
1. Sanofi-Aventis. Multaq (dronedarone hydrochloride) tablets prescribing information. Bridgewater, NJ; 2012 Jun.
2. Hohnloser SH, Crijns HJ, van Eickels M et al. Effect of dronedarone on cardiovascular events in atrial fibrillation. N Engl J Med. 2009; 360:668-78. http://www.ncbi.nlm.nih.gov/pubmed/19213680?dopt=AbstractPlus
3. Singh BN, Connolly SJ, Crijns HJ et al. Dronedarone for maintenance of sinus rhythm in atrial fibrillation or flutter. N Engl J Med. 2007; 357:987-99. http://www.ncbi.nlm.nih.gov/pubmed/17804843?dopt=AbstractPlus
4. Køber L, Torp-Pedersen C, McMurray JJ et al. Increased mortality after dronedarone therapy for severe heart failure. N Engl J Med. 2008; 358:2678-87. http://www.ncbi.nlm.nih.gov/pubmed/18565860?dopt=AbstractPlus
5. Hoy SM, Keam SJ. Dronedarone. Drugs. 2009; 69:1647-63. http://www.ncbi.nlm.nih.gov/pubmed/19678715?dopt=AbstractPlus
6. Riera AR, Uchida AH, Ferreira C et al. Relationship among amiodarone, new class III antiarrhythmics, miscellaneous agents and acquired long QT syndrome. Cardiol J. 2008; 15:209-19. http://www.ncbi.nlm.nih.gov/pubmed/18651412?dopt=AbstractPlus
7. Coletta AP, Cleland JG, Cullington D et al. Clinical trials update from Heart Rhythm 2008 and Heart Failure 2008: ATHENA, URGENT, INH study, HEART and CK-1827452. Eur J Heart Fail. 2008; 10:917-20. http://www.ncbi.nlm.nih.gov/pubmed/18678526?dopt=AbstractPlus
8. Garcia D, Cheng-Lai A. Dronedarone: a new antiarrhythmic agent for the treatment of atrial fibrillation. Cardiol Rev. 2009 Sep-Oct; 17:230-4.
9. Sanofi-Aventis, Bridgewater, NJ: Personal communication.
10. Sanofi-Aventis. Healthcare professional information sheet for Multaq (dronedarone). Bridgewater, NJ; 2012 Mar.
11. Sanofi-Aventis. Prescribing Multaq: Information for health care professionals. 2009 Dec. Available from website. Accessed 2010 Mar 18. http://www.multaq.com/HCP/MPACT/MPACT.aspx
12. Sanofi-Aventis. Risk evaluation and mitigation strategy (REMS): NDA 22-425 Multaq (dronedarone). 2009 Jun 9. Available from website. Accessed 2010 Mar 18. http://www.fda.gov/downloads/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/UCM187494.pdf
13. Tschuppert Y, Buclin T, Rothuizen LE et al. Effect of dronedarone on renal function in healthy subjects. Br J Clin Pharmacol. 2007; 64:785-91. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=2198776&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/17662087?dopt=AbstractPlus
14. Le Heuzey JY, De Ferrari GM, Radzik D et al. A short-term, randomized, double-blind, parallel-group study to evaluate the efficacy and safety of dronedarone versus amiodarone in patients with persistent atrial fibrillation. The DIONYSOS study. J Cardiovasc Electrophysiol. 2010 Jun; 21:597-605.
15. Savelieva I, Camm J. Update on atrial fibrillation: part II. Clin Cardiol. 2008; 31:102-8. http://www.ncbi.nlm.nih.gov/pubmed/18383050?dopt=AbstractPlus
16. Zimetbaum PJ. Dronedarone for atrial fibrillation—an odyssey. N Engl J Med. 2009 Apr; 360:1811-3. Commentary.
17. Schafer JA, Kjesbo NK, Gleason PP. Dronedarone: current evidence and future questions. Cardiovasc Ther. 2010; 28:38-47. http://www.ncbi.nlm.nih.gov/pubmed/20074258?dopt=AbstractPlus
18. Singh D, Cingolani E, Diamond GA et al. Dronedarone for atrial fibrillation. Have we expanded the therapeutic armamentarium? JACC. 2010; 55:1569-76. Commentary.
19. Ezekowitz MD. Maintaining sinus rhythm—making treatment better than the disease. N Engl J Med. 2009; 357:1039-41. Editorial.
20. Wyse DG, Waldo AL, DiMarco JP et al, for theAtrial Fibrillation Follow-up Investigation of Rhythm Management (AFFIRM) Investigators. A comparison of rate control and rhythm control in patients with atrial fibrillation. N Engl J Med. 2002 Dec 5;347:1825-33.
21. Falk RH. Management of atrial fibrillation—radical reform or modest modification? N Engl J Med. 2002; 347:1883-4. Editorial.
22. Opolski G, Torbicki A, Kosior DA et al, for the Investigators of the Polish HOT CAFE Trial. Rate control vs rhythm control in patients with nonvalvular persistent atrial fibrillation. Chest. 2004; 126:476–86. http://www.ncbi.nlm.nih.gov/pubmed/15302734?dopt=AbstractPlus
23. Prystowsky EN. Dronedarone and amiodarone—the safety versus efficacy debate. Nat Rev Cardiol. 2010 Jan;7:5-6.
24. Reviewers’ comments (personal observations).
25. Tichy EM, Medwid AJ, Mills EA et al. Significant sirolimus and dronedarone interaction in a kidney transplant recipient. Ann Pharmacother. 2010 Jul-Aug; 44:1338-41.
26. Coons JC, Plauger KM, Seybert AL et al. Worsening heart failure in the setting of dronedarone initiation. Ann Pharmacother. 2010; 44:1496-500. http://www.ncbi.nlm.nih.gov/pubmed/20628043?dopt=AbstractPlus
27. European Heart Rhythm Association, European Association for Cardio-Thoracic Surgery, Camm AJ et al. Guidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). Eur Heart J. 2010; 31:2369-429. http://www.ncbi.nlm.nih.gov/pubmed/20802247?dopt=AbstractPlus
28. Food and Drug Administration. FDA drug safety communication: severe liver injury associated with the use of dronedarone (marketed as Multaq). Rockville, MD: Food and Drug Administration; 2011 Jan 14. Available from FDA website. Accessed 2011 Feb 4. http://www.fda.gov/drugs/drugsafety/ucm240011.htm
29. Food and Drug Administration. FDA drug safety communication: Multaq (dronedarone) and increased risk of death and serious cardiovascular adverse events. Rockville, MD: Food and Drug Administration; 2011 Jul 21. Available from FDA website. Accessed 2011 Sep 15. http://www.fda.gov/Drugs/DrugSafety/ucm264059.htm
30. Permanent Atrial fibriLLAtion outcome Study using dronedarone on top of standard therapy (PALLAS). National Institutes of Health. Updated 2011 Jul 11. Available at clinicaltrials.gov website. Accessed 2011 Sep 15. http://clinicaltrials.gov/ct2/show/NCT01151137
32. Chew PH. Dear healthcare provider letter: Increased cardiovascular risk in permanent AF patients treated with Multaq (dronedarone). Bridgewater, NJ: Sanofi-Aventis; 2011 Aug.
33. Food and Drug Administration. FDA drug safety communication: Multaq (dronedarone) and increased risk of death and serious cardiovascular adverse events. Rockville, MD: Food and Drug Administration; 2011 Dec 19. Available from FDA website. Accessed 2012 Jan 15.
35. Connolly SJ, Camm AJ, Halperin JL et al. Dronedarone in high-risk permanent atrial fibrillation. N Engl J Med. 2011; 365:2268-76. http://www.ncbi.nlm.nih.gov/pubmed/22082198?dopt=AbstractPlus
More about dronedarone
- Check interactions
- Compare alternatives
- Reviews (53)
- Side effects
- Dosage information
- During pregnancy
- Drug class: group III antiarrhythmics
- En español