Diltiazem Hydrochloride (Monograph)
Brand names: Cardizem, Cartia XT, Dilt XR, Matzim LA, Taztia XT, Tiazac
Drug class: Class IV Antiarrhythmics
Introduction
Calcium-channel blocking agent; nondihydropyridine derivative.
Uses for Diltiazem Hydrochloride
Angina
Management of Prinzmetal variant angina and chronic stable angina
A drug of choice for the management of Prinzmetal variant angina (used alone or in combination with nitrates).
β-Blockers are recommended as the anti-ischemic drugs of choice in most patients with chronic stable angina; calcium-channel blockers may be substituted or added in patients who do not tolerate or respond adequately to β-blockers.
Also may be beneficial in patients with unstable angina† [off-label]; experts recommend a nondihydropyridine calcium-channel blocker (e.g., diltiazem, verapamil) for the relief of ongoing or recurrent ischemia when β-blocker therapy is inadequate, not tolerated, or contraindicated in patients with unstable angina who do not have clinically important left ventricular dysfunction, increased risk of cardiogenic shock, or AV block.
Hypertension
Oral management of hypertension (alone or in combination with other classes of antihypertensive agents).
Calcium-channel blockers are recommended as one of several preferred agents for the initial management of hypertension according to current evidence-based hypertension guidelines; other preferred options include ACE inhibitors, angiotensin II receptor antagonists, and thiazide diuretics. While there may be individual differences with respect to recommendations for initial drug selection and use in specific patient populations, current evidence indicates that these antihypertensive drug classes all generally produce comparable effects on overall mortality and cardiovascular, cerebrovascular, and renal outcomes.
Individualize choice of therapy; consider patient characteristics (e.g., age, ethnicity/race, comorbidities, cardiovascular risk) as well as drug-related factors (e.g., ease of administration, availability, adverse effects, cost).
A 2017 ACC/AHA multidisciplinary hypertension guideline classifies BP in adults into 4 categories: normal, elevated, stage 1 hypertension, and stage 2 hypertension. (See Table 1.)
Source: Whelton PK, Carey RM, Aronow WS et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13-115.
Individuals with SBP and DBP in 2 different categories (e.g., elevated SBP and normal DBP) should be designated as being in the higher BP category (i.e., elevated BP).
|
Category |
SBP (mm Hg) |
DBP (mm Hg) |
|
|---|---|---|---|
|
Normal |
<120 |
and |
<80 |
|
Elevated |
120–129 |
and |
<80 |
|
Hypertension, Stage 1 |
130–139 |
or |
80–89 |
|
Hypertension, Stage 2 |
≥140 |
or |
≥90 |
The goal of hypertension management and prevention is to achieve and maintain optimal control of BP. However, the BP thresholds used to define hypertension, the optimum BP threshold at which to initiate antihypertensive drug therapy, and the ideal target BP values remain controversial.
The 2017 ACC/AHA hypertension guideline generally recommends a target BP goal (i.e., BP to achieve with drug therapy and/or nonpharmacologic intervention) of <130/80 mm Hg in all adults regardless of comorbidities or level of atherosclerotic cardiovascular disease (ASCVD) risk. In addition, an SBP goal of <130 mm Hg generally is recommended for noninstitutionalized ambulatory patients ≥65 years of age with an average SBP of ≥130 mm Hg. These BP goals are based upon clinical studies demonstrating continuing reduction of cardiovascular risk at progressively lower levels of SBP.
Previous hypertension guidelines generally have based target BP goals on age and comorbidities. Guidelines such as those issued by the JNC 8 expert panel generally have targeted a BP goal of <140/90 mm Hg regardless of cardiovascular risk, and have used higher BP thresholds and target BPs in elderly patients compared with those recommended by the 2017 ACC/AHA hypertension guideline.
Some clinicians continue to support previous target BPs recommended by JNC 8 due to concerns about the lack of generalizability of data from some clinical trials (e.g., SPRINT study) used to support the 2017 ACC/AHA hypertension guideline and potential harms (e.g., adverse drug effects, costs of therapy) versus benefits of BP lowering in patients at lower risk of cardiovascular disease.
Consider potential benefits of hypertension management and drug cost, adverse effects, and risks associated with the use of multiple antihypertensive drugs when deciding a patient’s BP treatment goal.
For decisions regarding when to initiate drug therapy (BP threshold), the 2017 ACC/AHA hypertension guideline incorporates underlying cardiovascular risk factors. ASCVD risk assessment recommended by ACC/AHA for all adults with hypertension.
ACC/AHA currently recommend initiation of antihypertensive drug therapy in addition to lifestyle/behavioral modifications at an SBP ≥140 mm Hg or DBP ≥90 mm Hg in adults who have no history of cardiovascular disease (i.e., primary prevention) and a low ASCVD risk (10-year risk <10%).
For secondary prevention in adults with known cardiovascular disease or for primary prevention in those at higher risk for ASCVD (10-year risk ≥10%), ACC/AHA recommend initiation of antihypertensive drug therapy at an average SBP ≥130 mm Hg or an average DBP ≥80 mm Hg.
Adults with hypertension and diabetes mellitus, chronic kidney disease (CKD), or age ≥65 years of age are assumed to be at high risk for cardiovascular disease; ACC/AHA state that such patients should have antihypertensive drug therapy initiated at a BP ≥130/80 mm Hg.
In stage 1 hypertension, experts state that it is reasonable to initiate drug therapy using the stepped-care approach in which one drug is initiated and titrated and other drugs are added sequentially to achieve the target BP. Initiation of antihypertensive therapy with 2 first-line agents from different pharmacologic classes recommended in patients with stage 2 hypertension and average BP >20/10 mm Hg above BP goal.
Calcium-channel blockers may be preferred in hypertensive patients with certain coexisting conditions (e.g., ischemic heart disease) and in geriatric patients, including those with isolated systolic hypertension. Nondihydropyridine calcium-channel blockers (e.g., diltiazem, verapamil) may be beneficial in hypertensive patients with coexisting atrial fibrillation and a rapid ventricular rate.
Black hypertensive patients generally respond better to monotherapy with calcium-channel blockers or thiazide diuretics than to other antihypertensive drug classes (e.g., ACE inhibitors, angiotensin II receptor antagonists). However, the combination of an ACE inhibitor or an angiotensin II receptor antagonist with a calcium-channel blocker or thiazide diuretic produces similar BP lowering in black patients as in other racial groups.
Only extended-release formulations of diltiazem currently are recommended for management of hypertension.
Supraventricular Arrhythmias
Management of supraventricular tachycardias (SVTs), including rapid conversion to sinus rhythm of paroxysmal supraventricular tachycardias (PSVT) (e.g., those associated with Wolff-Parkinson-White or Lown-Ganong-Levine syndrome), and control of rapid ventricular rate in atrial flutter or fibrillation.
Vagal maneuvers and/or IV adenosine are considered first-line interventions for acute treatment of SVT when clinically indicated; if such measures are ineffective or not feasible, a nondihydropyridine calcium-channel blocker such as diltiazem may be used. Use only in hemodynamically stable patients who do not have impaired ventricular function.
Also has been used for treatment of other SVTs (e.g., atrial tachycardia† [off-label], junctional tachycardia† [off-label]).
Acute MI
Used in the early treatment and secondary prevention of acute MI† [off-label]; an effective anti-ischemic agent, but mortality benefit not demonstrated.
Calcium-channel blockers generally are used for their anti-ischemic and BP-reducing properties in the MI setting, and only when β-blockers (which have been shown to reduce mortality after MI) are ineffective, not tolerated, or contraindicated.
Experts state that calcium-channel blockers may be used to relieve ischemic symptoms, lower BP, or control rapid ventricular response rate associated with atrial fibrillation in patients with ST-segment-elevation MI (STEMI) who are intolerant to β-blockers.
Experts recommend a nondihydropyridine calcium-channel blocker for ongoing or recurrent ischemia in patients with non-ST-segment-elevation MI (NSTEMI) who have a contraindication to β-blockers and who do not have clinically important left ventricular dysfunction, increased risk of cardiogenic shock, or AV block.
Hyperthyroidism
Short-term adjunctive therapy in the treatment of tachycardia and tachyarrhythmias in patients with hyperthyroidism† [off-label] and/or thyrotoxicosis† in whom therapy with β-adrenergic blocking agents is contraindicated or not tolerated.
Diltiazem Hydrochloride Dosage and Administration
General
BP Monitoring and Treatment Goals
-
Monitor BP regularly (i.e., monthly) during therapy and adjust dosage of the antihypertensive drug until BP controlled.
-
If unacceptable adverse effects occur, discontinue drug and initiate another antihypertensive agent from a different pharmacologic class.
-
If adequate BP response not achieved with a single antihypertensive agent, either increase dosage of single drug or add a second drug with demonstrated benefit and preferably a complementary mechanism of action (e.g., angiotensin-converting enzyme [ACE] inhibitor, angiotensin II receptor antagonist, thiazide diuretic). Many patients will require at least 2 drugs from different pharmacologic classes to achieve BP goal; if goal BP still not achieved with 2 antihypertensive agents, add a third drug.
Administration
Administer by direct IV injection, continuous IV infusion, or orally.
Oral Administration
Conventional Tablets
Administer tablets orally 3–4 times daily before meals and at bedtime.
Extended-release Capsules
Administer orally; directions for administration (e.g., dosing frequency, whether to administer with or without food, potential for opening capsules and mixing with food) may vary by manufacturer and formulation; consult specific manufacturer’s information for additional information.
Cardizem CD, Dilt-XR, Tiazac, Taztia XT, or Cartia XT may be administered once daily; some diltiazem hydrochloride extended-release capsules (12 hours) are administered twice daily.
Cardizem CD and Cartia XT may be administered without regard to meals. However, Dilt-XR should be taken on an empty stomach, swallowed whole and not opened, chewed, or crushed.
Tiazac and Taztia XT may be opened and the entire contents sprinkled on a small amount of applesauce (not hot) immediately prior to administration; subdividing the contents of capsules is not recommended. Swallow the entire mixture without chewing. Immediately drink a glass of cool water to ensure that all of the mixture is swallowed. Do not store the sprinkle/food mixture for use at a later time.
Extended-release Tablets
Administer orally once daily without regard to meals. Tablet should be swallowed whole and not chewed or crushed.
IV Injection
Monitor ECG and BP continuously during IV administration.
Dilution
Injection solutions containing 5 mg/mL may be administered by direct IV injection without any further dilution.
Rate of Administration
Administer over 2 minutes.
IV Infusion
Reconstitution
Prepare 1-mg/mL solutions from the powder for IV infusion in ADD-Vantage vials according to the manufacturer’s directions.
Dilution
Alternatively, dilute 5-mg/mL injection solution in the appropriate volume of a compatible infusion solution (i.e., 0.9% sodium chloride, 5% dextrose, or 5% dextrose and 0.45% sodium chloride) to produce a final diltiazem hydrochloride concentration of 1, 0.83, or 0.45 mg/mL, respectively.
|
Quantity of 5 mg/mL Solution |
Diluent Volume |
Final Concentration |
|---|---|---|
|
25 mL |
100 mL |
1 mg/mL |
|
50 mL |
250 mL |
0.83 mg/mL |
|
50 mL |
500 mL |
0.45 mg/mL |
Rate of Administration
Usually 10 mg/hour; however, may range from 5–15 mg/hour.
Standardize 4 Safety
Standardized concentrations for IV diltiazem have been established through Standardize 4 Safety (S4S), a national patient safety initiative to reduce medication errors, especially during transitions of care. Because recommendations from the S4S panels may differ from the manufacturer’s prescribing information, caution is advised when using concentrations that differ from labeling, particularly when using rate information from the label. For additional information on S4S (including updates that may be available), see [Web] .
|
Patient Population |
Concentration Standards |
Dosing Units |
|---|---|---|
|
Adults |
1 mg/mL |
mg/hour |
Dosage
Available as diltiazem hydrochloride; dosage expressed in terms of the salt.
Adults
Prinzmetal Variant Angina
Conventional Tablets
OralInitially, 30 mg 4 times daily. Increase gradually at 1- to 2-day intervals until optimum control is obtained. Usual maintenance dosage is 180–360 mg daily. After manifestations are controlled, reduce dosage to lowest level that will maintain relief of symptoms.
Extended-release Capsules
OralInitially, 120 or 180 mg once daily when administered as extended-release capsules (Cardizem CD, Cartia XT). Individualize dosage based on response; titrate dosage increases over 7–14 days. Some patients may respond to higher dosages of up to 480 mg once daily.
Chronic Stable Angina
Conventional Tablets
OralInitially, 30 mg 4 times daily. Increase gradually at 1- to 2-day intervals until optimum control is obtained. Usual maintenance dosage is 180–360 mg daily. After manifestations are controlled, reduce dosage to lowest level that will maintain relief of symptoms.
Extended-release Capsules
OralInitially, 120 mg (Dilt-XR) or 120–180 mg (Cardizem CD, Cartia XT, Tiazac, Taztia XT) once daily when administered as extended-release capsules. Individualize dosage based on response; titrate dosage increases over 7–14 days. Some patients may respond to higher dosages of up to 480 (Cardizem CD, Cartia XT, Dilt-XR) to 540 mg (Tiazac, Taztia XT) once daily.
Extended-release Tablets
OralInitially, 180 mg once daily when administered as extended-release tablets (Cardizem LA or Matzim LA). Individualize dosage based on response; titrate dosage increases over 7–14 days. Some patients may respond to higher dosages of up to 360 mg once daily.
Hypertension
Extended-release Capsules or Tablets
OralManufacturer-recommended dosages vary based on formulation (see Table 4).
Per some experts, usual maintenance dosage of extended-release diltiazem hydrochloride for management of hypertension is 120–360 mg once daily.
Maximum hypotensive effect associated with a given dosage level usually is observed within 14 days.
|
Preparation |
Initial Dosage |
Usual Maintenance Dosage |
|---|---|---|
|
Cardizem LA |
180–240 mg once daily |
120–540 mg; |
|
Cardizem CD |
180–240 mg once daily |
240–360 mg daily |
|
Cartia XT |
180–240 mg once daily |
240–360 mg daily |
|
Diltiazem hydrochloride extended-release capsules (12 hours) |
60–120 mg twice daily |
240–360 mg daily |
|
Dilt-XR |
180–240 mg once daily |
180–480 mg once daily |
|
Matzim LA |
180–240 mg once daily |
|
|
Tiazac |
120–240 mg once daily |
120–540 mg once daily |
|
Taztia XT |
120–240 mg once daily |
120–540 mg once daily |
Switching to Extended-release Preparations
OralPatients whose BP is adequately controlled with diltiazem therapy (as tablets or other extended-release capsules) alone or in combination with another antihypertensive agent may be safely switched to Cardizem CD or Cartia XT extended-release capsules or Cardizem LA or Matzim LA extended-release tablets at the nearest equivalent daily dosage. Subsequent titration of dosage is based on the clinical response of the patient.
Supraventricular Arrhythmias
Conversion of PSVT to Sinus Rhythm
IVInitially, 0.25 mg/kg based on actual body weight (average dose: 20 mg) by direct IV injection over 2 minutes. If response is inadequate (i.e., conversion to normal sinus rhythm does not occur) give a second dose of 0.35 mg/kg based on actual body weight (average dose: 25 mg) 15 minutes after the initial dose.
Maintenance infusion: 5–15 mg/hour; titrate dose to heart rate.
Patients with low body weights should be dosed on a mg/kg basis.
Ventricular Rate Control in Atrial Fibrillation and Flutter
IVInitially, 0.25 mg/kg based on actual body weight (average dose: 20 mg) by direct IV injection over 2 minutes. If response is inadequate, give 0.35 mg/kg based on actual body weight (average dose: 25 mg) 15 minutes after the initial dose.
Maintenance infusion: 5–15 mg/hour; titrate dose to heart rate.
Other SVTs (e.g., Junctional Tachycardia†, Atrial Tachycardia†)
IVInitially, 0.25 mg/kg by direct IV injection over 2 minutes followed by a maintenance IV infusion of 5–10 mg/hour (up to 15 mg/hour).
Prescribing Limits
Adults
Angina
Oral
Cardizem LA and Matzim LA extended-release tablets: Maximum 360 mg daily.
Cardizem CD, Dilt-XR, and Cartia XT extended-release capsules: Maximum 480 mg daily.
Tiazac and Taztia XT extended-release capsules: Maximum 540 mg daily.
Hypertension
Oral
Cardizem CD and Cartia XT extended-release capsules: Maximum 480 mg daily.
Dilt-XR,Taztia XT, and Tiazac extended-release capsules and Cardizem LA and Matzim LA extended-release tablets: Maximum 540 mg daily.
Supraventricular Arrhythmias
IV
Maintenance infusion: Maximum 15 mg/hour for ≤24 hours.
Special Populations
Hepatic Impairment
Supraventricular Arrhythmias
Atrial Fibrillation and Flutter
IVMaintenance infusion: Dosage requirements may be lower.
Geriatric Patients
Angina
Select dosage cautiously; geriatric patients may respond to lower dosages.
Hypertension
Select dosage cautiously. The manufacturer of Dilt-XR states that patients ≥60 years of age may respond to an initial daily dosage of 120 mg.
Atrial Fibrillation and Flutter
Maintenance IV infusion: Dosage requirements may be lower.
Cautions for Diltiazem Hydrochloride
Contraindications
-
Contraindicated in patients with known hypersensitivity to the drug.
-
Sick sinus syndrome (unless a functioning ventricular pacemaker is in place).
-
Second- or third-degree AV block (unless a functioning ventricular pacemaker is in place).
-
Severe hypotension (SBP <90 mm Hg).
-
Oral preparations contraindicated in patients with acute MI with radiographically documented pulmonary congestion.
-
IV diltiazem contraindicated in patients with cardiogenic shock.
-
IV diltiazem contraindicated in patients with VT.
-
IV diltiazem contraindicated in patients with atrial flutter or fibrillation with an accessory pathway (e.g., those with Wolff-Parkinson-White or Lown-Ganong-Levine syndrome).
-
IV diltiazem contraindicated if concurrent or recent (e.g., within a few hours) administration of IV β-adrenergic blockers.
Warnings/Precautions
Warnings
Cardiac Conduction
Potential for abnormally slow heart rate (particularly in patients with sick sinus syndrome) or second- or third-degree AV block.
Additive effects on cardiac conduction (e.g., prolonging AV node conduction) possible with concomitant use of diltiazem with β-adrenergic blocking agents or digoxin.
If high-degree AV block occurs in patients with sinus rhythm receiving IV diltiazem, discontinue the drug and institute appropriate supportive measures.
Heart Failure
Risk of heart failure, especially in those with preexisting ventricular impairment; limited experience in patients with impaired ventricular function receiving concomitant β-adrenergic blocking agents. Use with caution.
Hypotension
Possible symptomatic hypotension.
Acute Hepatic Injury
Substantial elevations in hepatic function test results (e.g., serum AST [SGOT], ALT [SGPT], LDH, alkaline phosphatase) and phenomena associated with hepatocellular injury rarely reported. Usually occurs early in therapy (e.g., 1–8 weeks); reversible upon discontinuation of therapy.
Ventricular Premature Beats
With IV administration, possible transient VPB on conversion of PSVT to sinus rhythm; appear to be benign and of little clinical importance.
Sensitivity Reactions
Possible diltiazem-induced skin eruptions with oral preparations; may infrequently progress to severe dermatologic reactions (e.g., erythema multiforme, exfoliative dermatitis). If effects persist during therapy, the drug should be discontinued. Potential for occurrence with IV administration.
Specific Populations
Pregnancy
Category C.
Lactation
Distributed into milk; discontinue nursing.
Pediatric Use
Safety and efficacy not established.
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether geriatric patients respond differently than younger adults. Select dosage with caution because of age-related decreases in hepatic, renal, and/or cardiac function and potential for concomitant disease and drug therapy.
Hepatic Impairment
Use with caution.
Renal Impairment
Use with caution.
Common Adverse Effects
With oral therapy, edema, headache, dizziness, asthenia, first-degree AV block.
With IV therapy, hypotension, injection site reactions, vasodilation, arrhythmia.
Drug Interactions
Metabolized principally by CYP3A4. Inhibits CYP3A4.
Drugs Affecting Hepatic Microsomal Enzymes
Inhibitors, inducers, and substrates of CYP3A4: potential pharmacokinetic interaction (altered plasma diltiazem concentrations).
Drugs Metabolized by Microsomal Enzymes
Potential pharmacokinetic interaction: altered bioavailability and/or clearance of drugs metabolized by CYP3A4.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Anesthetics, general |
Possible increased depression of cardiac contractility, conductivity, and automaticity as well as vascular dilation |
Titrate dosage of each drug carefully |
|
Atazanavir |
Possible increased plasma diltiazem concentrations and additive effect on PR interval prolongation |
Use concomitantly with caution. Reduce diltiazem dosage by 50%; monitor ECG |
|
β-Adrenergic blockers |
Potential for additive negative effects on myocardial contractility, heart rate, and prolonging AV conduction Increased plasma concentrations of propranolol and metoprolol |
Do not administer IV diltiazem and IV β-adrenergic blocking agents within a few hours of each other Propranolol dosage adjustment may be necessary when diltiazem is initiated or discontinued |
|
Benzodiazepines (e.g., midazolam, triazolam) |
Possible increased benzodiazepine plasma concentrations and AUC resulting in increased adverse effects (e.g., prolonged sedation, respiratory depression) |
|
|
Buspirone |
Increased plasma concentration and AUC of buspirone Potential for increased effects and toxicity of buspirone |
Dosage adjustment of buspirone may be necessary based on clinical assessments |
|
Carbamazepine |
Possible increased serum or plasma carbamazepine concentrations and associated neurologic and sensory manifestations of carbamazepine toxicity |
Avoid concurrent use, if possible Monitor for manifestations of carbamazepine toxicity; adjust carbamazepine dosage accordingly |
|
Clonidine |
Sinus bradycardia resulting in hospitalization and pacemaker insertion reported |
Monitor heart rate |
|
Cyclosporine |
Possible increased blood cyclosporine concentrations and consequent nephrotoxicity |
Monitor cyclosporine concentration in biologic fluid (especially when diltiazem therapy is initiated, adjusted, or discontinued); adjust cyclosporine dosage as needed |
|
Digoxin |
Possible increased serum digoxin concentrations Potential for additive effects on cardiac conduction (e.g., prolonging AV node conduction) |
Monitor serum digoxin concentrations carefully and observe the patient closely for signs of digoxin toxicity when administered concomitantly, especially in geriatric patients, patients with unstable renal function, or those with serum digoxin concentrations in the upper therapeutic range before diltiazem is administered Reduce digoxin dosage if necessary |
|
Histamine H2-receptor antagonists (e.g., cimetidine, ranitidine) |
Possible increased plasma diltiazem concentrations with concomitant administration of cimetidine Ranitidine coadministration produced smaller and not substantial alterations in diltiazem pharmacokinetics |
Monitor effects of diltiazem carefully when cimetidine therapy is initiated or discontinued in patients receiving diltiazem; adjust diltiazem dosage, if necessary |
|
HMG-CoA reductase inhibitors (e.g., lovastatin, pravastatin, simvastatin) |
Possible increased mean AUCs and peak plasma concentrations of lovastatin with concomitant use Increased mean AUCs of simvastatin with concomitant use May increase risk of myopathy and rhabdomyolysis with statins metabolized by CYP3A4 Interaction not observed when used concomitantly with pravastatin |
When concomitant use of diltiazem and lovastatin is required, initiate lovastatin at dosage of 10 mg once daily; may increase lovastatin dosage to maximum of 20 mg once daily Do not exceed simvastatin dosage of 10 mg daily and diltiazem dosage of 240 mg daily if used concomitantly Non-CYP3A4-metabolized statin should be used if possible Monitor patients receiving lovastatin or simvastatin concomitantly with diltiazem for evidence of statin toxicity (e.g., rhabdomyolysis, myositis) |
|
Ivabradine |
Increased exposure to ivabradine; may exacerbate bradycardia and conduction disturbances |
Avoid concomitant use |
|
Nitrates |
Interaction unlikely |
|
|
Quinidine |
Possible increased AUC and decreased clearance of quinidine |
Monitor for adverse effects of quinidine; adjust dosage accordingly |
|
Rifampin |
Decreased bioavailability and increased clearance of diltiazem |
Avoid concomitant use; consider alternative therapy |
Diltiazem Hydrochloride Pharmacokinetics
Absorption
Bioavailability
Following oral administration of conventional tablets, approximately 80% of a dose is rapidly absorbed from the GI tract.
Absolute bioavailability is about 40%; undergoes extensive first-pass metabolism.
|
Preparation |
Time (hours) |
|---|---|
|
Conventional tablets (e.g., Cardizem) |
2–4 |
|
Cardizem CD extended-release capsules |
10–14 |
|
Cardizem LA or Matzim LA extended-release tablets |
11–18 |
|
Diltiazem hydrochloride extended-release capsules (12 hours) |
6–11 |
Onset
Following direct IV injection, reductions in heart rate usually occur within 3 minutes and hemodynamic effects (e.g., decrease in BP) generally occur within 2 minutes; effects on the AV node generally occur within minutes following initiation of a continuous IV infusion.
Duration
Following direct IV injection, reductions in heart rate generally persist for 1–3 hours; blood pressure reductions following direct IV injection generally are short-lived but may last 1–3 hours. Effects on the AV node may persist for 0.5–10 hours following a continuous IV infusion.
Food
Rate of absorption may be increased if Tiazac extended-release capsules are taken with a high-fat meal. Food may affect the extent of absorption of some extended-release capsules (Dilt-XR).
Distribution
Extent
Rapidly and extensively distributed into body tissues.
Distributed into milk, in concentrations approximately equal to maternal serum concentrations.
Plasma Protein Binding
About 70–85% is bound to plasma proteins, but only 30–40% is bound to albumin.
Elimination
Metabolism
Rapidly and almost completely metabolized in the liver to several active and at least 5 inactive metabolites principally via CYP enzyme system, mainly CYP3A4.
Elimination Route
Excreted principally in urine as metabolites, with approximately 2–4% of a dose excreted unchanged.
Half-life
2–11 hours.
Special Populations
In geriatric patients, plasma half-life of the drug may be increased.
In patients with severe renal impairment, pharmacokinetics were unchanged.
Oral clearance may be reduced and half-life prolonged in patients with liver cirrhosis.
Stability
Storage
Oral
Conventional Tablets
Tight containers at 25°C (may be exposed to 15–30°C).
Protect from excessive humidity.
Extended-release Capsules
25°C (may be exposed to 15–30°C).
Protect from excessive humidity.
Extended-release Tablets
Tight, light-resistant containers at 25°C (may be exposed to 15–30°C).
Protect from excessive humidity.
Parenteral
Injection
2–8°C. Do not freeze. May store at room temperature for up to 1 month; discard after 1 month if not used.
Diluted solutions (up to 1 mg/mL in 0.9% sodium chloride, 5% dextrose, or 5% dextrose and 0.45% sodium chloride injection) prepared in glass or PVC bags: Store at room temperature or under refrigeration and use within 24 hours.
Powder for IV Infusion
20–25°C. Do not freeze.
Reconstituted and activated ADD-Vantage vials prepared using 0.9% sodium chloride or 5% dextrose injection: Store at room temperature or under refrigeration and use within 24 hours.
Actions
-
Inhibits transmembrane influx of extracellular calcium ions across the membranes of myocardial cells and vascular smooth muscle cells, without changing serum calcium concentrations.
-
Peripheral arterial vasodilator; acts directly on vascular smooth muscle causing reduction in peripheral vascular resistance (afterload) and BP.
-
Substantial inhibitory effects on the cardiac conduction system, acting principally at the atrioventricular (AV) node to slow conduction time and prolong AV nodal refractoriness.
Advice to Patients
-
Importance of swallowing extended-release tablets whole; do not chew, crush, or break.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules, extended-release |
60 mg* |
Diltiazem Hydrochloride Capsules Extended-release (12 hours) |
|
|
90 mg* |
Diltiazem Hydrochloride Capsules Extended-release (12 hours) |
|||
|
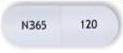
120 mg* |
Cardizem CD (24 hours) |
Valeant |
||
|
Cartia XT (24 hours) |
Actavis |
|||
|
Dilt-XR (24 hours) |
Apotex |
|||
|
Diltiazem Hydrochloride Capsules Extended-release (12 hours) |
||||
|
Diltiazem Hydrochloride Capsules Extended-release (24 hours) |
||||
|
Taztia XT (24 hours) |
Actavis |
|||
|
Tiazac (24 hours) |
Valeant |
|||
|
180 mg* |
Cardizem CD (24 hours) |
Valeant |
||
|
Cartia XT (24 hours) |
Actavis |
|||
|
Dilt-XR (24 hours) |
Apotex |
|||
|
Diltiazem Hydrochloride Capsules Extended-release (24 hours) |
||||
|
Taztia XT (24 hours) |
Actavis |
|||
|
Tiazac (24 hours) |
Valeant |
|||
|
240 mg* |
Cardizem CD (24 hours) |
Valeant |
||
|
Cartia XT (24 hours) |
Actavis |
|||
|
Dilt-XR (24 hours) |
Apotex |
|||
|
Diltiazem Hydrochloride Capsules Extended-release (24 hours) |
||||
|
Taztia XT (24 hours) |
Actavis |
|||
|
Tiazac (24 hours) |
Valeant |
|||
|
300 mg* |
Cardizem CD (24 hours) |
Valeant |
||
|
Cartia XT (24 hours) |
Actavis |
|||
|
Dilt XR (24 hours) |
Apotex |
|||
|
Diltiazem Hydrochloride Capsules Extended-release (24 hours) |
||||
|
Taztia XT (24 hours) |
Actavis |
|||
|
Tiazac (24 hours) |
Valeant |
|||
|
360 mg* |
CardizemCD (24 hours) |
Valeant |
||
|
Diltiazem Hydrochloride Capsules Extended-release (24 hours) |
||||
|
Taztia XT (24 hours) |
Actavis |
|||
|
Tiazac (24 hours) |
Valeant |
|||
|
420 mg |
Tiazac (24 hours) |
Valeant |
||
|
Tablets |
30 mg* |
Cardizem |
Valeant |
|
|
Diltiazem Hydrochloride Tablets |
||||
|
60 mg* |
Cardizem (scored) |
Valeant |
||
|
Diltiazem Hydrochloride Tablets |
||||
|
90 mg* |
Cardizem (scored) |
Valeant |
||
|
Diltiazem Hydrochloride Tablets |
||||
|
120 mg* |
Cardizem (scored) |
Valeant |
||
|
Diltiazem Hydrochloride Tablets |
||||
|
Tablets, extended-release |
120 mg* |
Cardizem LA (24 hours) |
Valeant |
|
|
Diltiazem Hydrochloride Tablets Extended-release (24 hours) |
||||
|
180 mg* |
Cardizem LA (24 hours) |
Valeant |
||
|
Diltiazem Hydrochloride Tablets Extended-release (24 hours) |
||||
|
Matzim LA (24 hours) |
Actavis |
|||
|
240 mg* |
Cardizem LA (24 hours) |
Valeant |
||
|
Diltiazem Hydrochloride Tablets Extended-release (24 hours) |
||||
|
Matzim LA (24 hours) |
Actavis |
|||
|
300 mg* |
Cardizem LA (24 hours) |
Valeant |
||
|
Diltiazem Hydrochloride Tablets Extended-release (24 hours) |
||||
|
Matzim LA (24 hours) |
Actavis |
|||
|
360 mg* |
Cardizem LA (24 hours) |
Valeant |
||
|
Diltiazem Hydrochloride Tablets Extended-release (24 hours) |
||||
|
Matzim LA (24 hours) |
Actavis |
|||
|
420 mg* |
Cardizem LA (24 hours) |
Valeant |
||
|
Diltiazem Hydrochloride Tablets Extended-release (24 hours) |
||||
|
Matzim LA (24 hours) |
Actavis |
|||
|
Parenteral |
For injection, for IV infusion only |
100 mg* |
Diltiazem Hydrochloride for Injection ADD-Vantage |
Hospira |
|
Injection |
5 mg/mL (25, 50, and 125 mg)* |
Diltiazem Hydrochloride Injection |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
More about diltiazem
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (192)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: calcium channel blockers
- Breastfeeding
Patient resources
Professional resources
- Diltiazem prescribing information
- Diltiazem CD (FDA)
- Diltiazem Extended Release Tablets (FDA)
- Diltiazem Injection (FDA)
- Diltiazem Tablets (FDA)
Other brands
Cardizem, Cartia XT, Tiadylt ER, Dilt-XR, ... +6 more