Dabigatran (Monograph)
Brand name: Pradaxa
Drug class: Direct Thrombin Inhibitors
Chemical name: N-[[2-[[[4-(Aminoiminomethyl)phenyl]amino]methyl]-1-methyl-1H-benzimidazol-5-yl]carbonyl]-N-2-pyridinyl-β-alanine
Molecular formula: C25H25N7O3C34H41N7O5C34H41N7O5•CH4O3S
CAS number: 211914-51-1
Warning
- Risk of Thrombosis Following Premature Discontinuance of Anticoagulation
-
Premature discontinuance of any oral anticoagulant, including dabigatran, increases risk of thrombotic events.1
-
If discontinuance is required for reasons other than pathologic bleeding or completion of a course of therapy, consider coverage with an alternative anticoagulant.1
- Spinal/Epidural Hematoma
-
Risk of epidural or spinal hematomas and neurologic injury, including long-term or permanent paralysis, in patients who are anticoagulated and also receiving neuraxial (spinal/epidural) anesthesia or spinal puncture.1
-
Risk increased by use of indwelling epidural catheters or by concomitant use of drugs affecting hemostasis (e.g., NSAIAs, platelet-aggregation inhibitors, other anticoagulants).1
-
Risk also increased by spinal deformity, spinal surgery, or history of traumatic or repeated epidural or spinal puncture.1
-
Monitor frequently for signs and symptoms of neurologic impairment and treat urgently if neurologic compromise noted.1
-
Consider potential benefits versus risks of spinal or epidural anesthesia or spinal puncture in patients receiving or being considered for anticoagulant therapy.1
Introduction
Anticoagulant; a synthetic reversible direct thrombin inhibitor.1 2 10 13
Uses for Dabigatran
Embolism Associated with Atrial Fibrillation
Reduction in risk of stroke and systemic embolism in adult patients with nonvalvular atrial fibrillation.1 2 3 5 18 20 21 30 32
Direct oral anticoagulants (DOACs; apixaban, dabigatran, edoxaban, rivaroxaban) are noninferior or superior to warfarin in reducing thromboembolic risk in patients with nonvalvular atrial fibrillation and associated with reduced risk of serious bleeding.18 20 82 87 1007
The American College of Chest Physicians (ACCP), American Stroke Association (ASA), American College of Cardiology (ACC), American Heart Association (AHA), and other experts recommend antithrombotic therapy in all patients with nonvalvular atrial fibrillation who are considered to be at increased risk of stroke, unless contraindicated.20 21 80 81 82 87 989 990 999 1007
Current guidelines recommend use of the CHA2DS2-VASc risk stratification tool to assess a patient’s risk of stroke and need for anticoagulant therapy.82 989 1007
Experts state that antithrombotic therapy generally is not necessary in low-risk patients (CHA2DS2-VASc score of 0 in males or 1 in females), but should be considered in all higher-risk patients.87 989 1007 1017
In patients with nonvalvular atrial fibrillation who are eligible for oral anticoagulant therapy, DOACs are recommended over warfarin based on improved safety and similar or improved efficacy.82 87 989 1007
Relative efficacy and safety of dabigatran and other DOACs (e.g., apixaban, rivaroxaban, edoxaban) remains to be fully elucidated.989
When selecting an appropriate anticoagulant, consider factors such as the absolute and relative risks of stroke and bleeding; costs; patient compliance, preference, tolerance, and comorbidities; and other clinical factors such as renal function and degree of INR control (if the patient has been taking warfarin).80 81 82 83 84 989 1007
Experts state antithrombotic therapy in patients with atrial flutter generally should be managed in the same manner as in patients with atrial fibrillation.80 82 999 1007
DOACs including dabigatran have been used for pharmacologic cardioversion† [off-label] in patients with atrial fibrillation or atrial flutter of >48 hours’ duration or of unknown duration; DOACs are recommended as an alternative to warfarin in this setting.87 1007
Contraindicated in patients with prosthetic mechanical heart valves; increased risk of serious thromboembolic and bleeding events observed in such patients receiving dabigatran compared with warfarin therapy.1 49 50
Not generally recommended in patients with other forms of valvular heart disease, including those with bioprosthetic heart valves.1 49 1164
Venous Thromboembolism – Treatment and Secondary Prevention
Treatment of acute DVT and/or PE in adults following initial treatment with a parenteral anticoagulant for 5–10 days.1 74 75 Also used to reduce the risk of recurrent DVT and PE in adults treated previously for an acute venous thromboembolic event (VTE).1 74 75 76
Treatment of VTE in pediatric patients 3 months to <18 years of age after at least 5 days of initial parenteral anticoagulant treatment and to reduce the risk of recurrent VTE in such patients who have been previously treated.1 1164
FDA indication for pediatric patients is product-specific.1 Dabigatran capsules are indicated for children ≥8 years of age.1 Dabigatran pellets are indicated for children 3 months to <12 years of age.1164
DOACs are among several anticoagulants that can be used for treatment of VTE.1005 1106 DOACs have similar efficacy to warfarin, but reduced bleeding (particularly intracranial hemorrhage) and greater convenience for patients and healthcare providers.1106
DOACs generally should not be used in settings with increased risk of bleeding, morbid obesity (body weight >120 kg or BMI >40 mg/m2), drug-drug interactions, or GI complications affecting oral therapy (e.g., poor absorption, nausea and vomiting) because of lack of safety data.1102 1106
In patients with cancer and established VTE, low molecular weight heparins (LMWHs) or oral factor Xa inhibitors (e.g., apixaban, rivaroxaban, edoxaban) are generally recommended over warfarin for long-term anticoagulation.1005 1102 1103 ACCP and ASH recommend the use of an oral factor Xa inhibitor over LMWH for the initiation and treatment phases of therapy in patients with cancer-associated thrombosis.1103 1106
Thromboprophylaxis in Major Orthopedic Surgery
Prevention of postoperative DVT and PE in adults undergoing hip-replacement surgery.1 1003
Shown to be as effective as enoxaparin in reducing risk of VTE in patients undergoing elective total hip-replacement surgery with similar rates of bleeding.1 1041 1042
Also has been used for VTE prevention in patients undergoing total knee-replacement surgery† [off-label].1003 1049 1050
ACCP and other clinicians consider DOACs an acceptable option for pharmacologic thromboprophylaxis in patients undergoing total hip- or knee-replacement surgery.1003 1008
Drug selection and duration of therapy should be individualized based on type of surgery, patient risk factors for embolism and bleeding, costs, patient compliance, preference, tolerance, and comorbidities, and other clinical factors such as renal function.1003 1108
Dabigatran Dosage and Administration
General
Pretreatment Screening
-
Prior to initiating therapy with dabigatran, assess renal function in all patients.1 1164 In children, estimate the glomerular filtration rate (eGFR) using the Schwarz formula as follows: eGFR = (0.413 × height in cm)/serum creatinine in mg/dL.1 1164 Avoid use of dabigatran in pediatric patients with an eGFR <50 mL/minute per 1.73 m2.1 1164
-
When used in pediatric patients for treatment and secondary prevention of venous thromboembolism (VTE), obtain body weight for dosing.1 1164
Patient Monitoring
-
Periodically assess renal function as clinically indicated (i.e., more frequently in situations that may be associated with a decline in renal function) and adjust therapy accordingly.1 1164
-
When used in pediatric patients for treatment and secondary prevention of VTE, periodically assess body weight and adjust doses and dosage forms accordingly.1 1164
-
If dabigatran is administered in an epidural or spinal anesthesia/analgesia or lumbar puncture setting, frequently monitor for signs or symptoms of neurological impairment (e.g., numbness, tingling, weakness in lower limbs, bowel and/or bladder dysfunction).1 1164
-
Monitor patients for any signs or symptoms of bleeding (e.g., unusual bruising) during therapy.1 1164
-
Routine monitoring of coagulation status is not required in patients receiving dabigatran.1 10 When necessary, the manufacturer states that the ecarin clotting time (ECT) or the activated partial thromboplastin time (aPTT) may be used to assess the anticoagulant effects of dabigatran; however, results of such tests should be interpreted with caution.1 10 Use of the prothrombin time (PT)/international normalized ratio (INR) should be avoided since this test is relatively insensitive to the effects of dabigatran and results may be unreliable.1 10 44 48
Dispensing and Administration Precautions
-
Dabigatran is available in different dosage forms and not all forms are approved for the same indications and age groups.1 1164 Dabigatran dosage forms are not interchangeable due to bioavailability differences.1 1164 Avoid substituting different dosage forms on a mg-to-mg basis and do not combine more than one dosage form to achieve the total dose.1 1164
-
Based on the Institute for Safe Medication Practices (ISMP), dabigatran is a high-alert medication that has a heightened risk of causing significant patient harm when used in error.1169
Administration
Oral Administration
Administer orally (as capsules or oral pellets).1 1164
Dosage forms are not interchangeable.1 1164
Capsules
Administer orally twice daily without regard to meals.1 Consider administration with food, if GI distress occurs.1
Capsules may be used in pediatric patients ≥8 years of age who are able to swallow capsules whole.1 Administer one dose in the morning and one in the evening, 12 hours apart.1
Do not remove capsules from bottle or blister package until time of use.1 36
Swallow capsules whole with full glass of water; do not chew, break, or empty the contents of the capsule.1
Take a missed dose as soon as it is remembered on the same day.1 If a missed dose cannot be taken at least 6 hours before next scheduled dose, skip the dose; do not double doses.1
Pellets
May use oral pellets in children 3 months to <12 years of age as soon as they are able to swallow soft foods.1164
Administer one dose in the morning and one in the evening, 12 hours apart.1 1164 Administer oral pellets twice daily before a meal to ensure that the child takes the full dose.1164
Swallow pellets without chewing after mixing with 2 teaspoons of a soft food at room temperature (e.g., baby rice cereal prepared with water, mashed carrots, apple sauce, or mashed banana); alternatively mix with 1–2 ounces of apple juice for drinking.1164 Do not use milk, milk products, or soft foods containing milk to prepare the dose.1164
Administer immediately after mixing or within 30 minutes.1164
Do not administer via syringe or feeding tubes.1164
Discard any dose not administered within 30 minutes and prepare a new dose as necessary.1164
Do not administer a second dose if a partial dose has been taken.1164 Administer the next dose as scheduled approximately 12 hours later.1164
Administer a missed dose as soon as it is remembered on same day; do not administer missed dose if it cannot be taken at least 6 hours before next scheduled dose.1 1164 Do not give a double dose.1164
Do not remove packet from aluminum bag until time of use.1164
Dosage
Available as dabigatran etexilate mesylate; dosage expressed in terms of the prodrug, dabigatran etexilate.1
Pediatric Patients
Venous Thromboembolism – Treatment and Secondary Prevention
Oral
Pediatric patients 3 months to <12 years of age with eGFR (Schwartz) >50 mL/minute per 1.73 m2: Table 1 provides dosing recommendations for the oral pellets in patients <2 years of age and Table 2 provides recommendations for the oral pellets in patients 2 to <12 years of age.1164
|
Actual body weight |
Age |
Dose given twice daily |
Number of packets needed |
|---|---|---|---|
|
3 kg to <4 kg |
3 to <6 months |
30 mg |
One 30 mg packet twice daily |
|
4 kg to <5 kg |
3 to <10 months |
40 mg |
One 40 mg packet twice daily |
|
5 kg to <7 kg |
3 to <5 months |
40 mg |
One 40 mg packet twice daily |
|
5 to <24 months |
50 mg |
One 50 mg packet twice daily |
|
|
7 kg to <9 kg |
3 to <4 months |
50 mg |
One 50 mg packet twice daily |
|
4 to <9 months |
60 mg |
Two 30 mg packets twice daily |
|
|
9 to <24 months |
70 mg |
One 30 mg plus one 40 mg packet twice daily |
|
|
9 kg to <11 kg |
5 to <6 months |
60 mg |
Two 30 mg packets twice daily |
|
6 to <11 months |
80 mg |
Two 40 mg packets twice daily |
|
|
11 to <24 months |
90 mg |
One 40 mg plus one 50 mg packet twice daily |
|
|
11 kg <13 kg |
8 to <18 months |
100 mg |
Two 50 mg packets twice daily |
|
18 to <24 months |
110 mg |
One 110 mg packet twice daily |
|
|
13 kg to <16 kg |
10 to <11 months |
100 mg |
Two 50 mg packets twice daily |
|
11 to <24 months |
140 mg |
One 30 mg plus one 110 mg packet twice daily |
|
|
16 kg to <21 kg |
12 to <24 months |
140 mg |
One 30 mg plus one 110 mg packet twice daily |
|
21 kg to <26 kg |
18 to <24 months |
180 mg |
One 30 mg plus one 150 mg packet twice daily |
|
Actual body weight |
Dose given twice daily |
Number of packets needed |
|---|---|---|
|
7 kg to <9 kg |
70 mg |
One 30 mg plus one 40 mg packet twice daily |
|
9 kg to <11 kg |
90 mg |
One 40 mg plus one 50 mg packet twice daily |
|
11 kg to <13 kg |
110 mg |
One 110 mg packet twice daily |
|
13 kg to <16 kg |
140 mg |
One 30 mg plus one 110 mg packet twice daily |
|
16 kg to <21 kg |
170 mg |
One 20 mg plus one 150 mg packet twice daily |
|
21 kg to <41 kg |
220 mg |
Two 110 mg packets twice daily |
|
≥41 kg |
260 mg |
One 110 mg plus one 150 mg packet twice daily |
Pediatric patients 8 to <18 years of age with eGFR (Schwartz) >50 mL/minute per 1.73 m2:Table 3 provides dosage recommendations for the capsules in patients 8 to <18 years of age.1
|
Actual body weight |
Dose given twice daily |
Number of capsules needed |
|---|---|---|
|
11 kg to <16 kg |
75 mg twice daily |
One 75 mg capsule twice daily |
|
16 kg to <26 kg |
110 mg twice daily |
One 110 mg capsule twice daily |
|
26 kg to <41 kg |
150 mg twice daily |
One 150 mg capsule twice daily |
|
Or |
||
|
Two 75 mg capsules twice daily |
||
|
41 kg to <61 kg |
185 mg twice daily |
One 110 mg plus one 75 mg capsule twice daily |
|
61 kg to <81 kg |
220 mg twice daily |
Two 110 mg capsules twice daily |
|
≥81 kg |
260 mg twice daily |
One 150 mg plus one 110 mg capsule twice daily |
|
Or |
||
|
One 110 mg plus two 75 mg capsules twice daily |
Adults
Embolism Associated with Atrial Fibrillation
Oral
Patients with Clcr >30 mL/minute: 150 mg twice daily.1
Venous Thromboembolism - Treatment and Secondary Prevention
Oral
Patients with Clcr >30 mL/minute: 150 mg twice daily following 5–10 days of therapy with a parenteral anticoagulant.1
Determine optimum duration of anticoagulation based on individual clinical situation (e.g., location of thrombi, presence or absence of precipitating factors for thrombosis, presence of cancer, risk of bleeding).1005 In general, ACCP states that anticoagulant therapy should be continued beyond the acute treatment period for ≥3 months, and possibly longer in certain patients with a high risk of recurrence and low or moderate risk of bleeding.1005
Thromboprophylaxis in Hip Replacement Surgery
Oral
Patients with Clcr >30 mL/minute: Single dose of 110 mg administered 1–4 hours after surgery, provided hemostasis has been achieved, followed by 220 mg once daily.1 If dabigatran therapy not initiated on day of surgery, initiate therapy with 220 mg once daily when hemostasis established.1
Manufacturer recommends treatment duration of 28–35 days.1 ACCP recommends at least 10–14 days, possibly up to 35 days, for patients undergoing major orthopedic surgery.1003
Transitioning from Other Anticoagulant Therapy
Transitioning from warfarin to dabigatran: Discontinue warfarin and initiate dabigatran when INR is <2.1 1164
Transitioning from LMWH to dabigatran: Discontinue LMWH and initiate dabigatran within 2 hours prior to what would have been the time of the next scheduled LMWH dose.1 1164
Transitioning from heparin IV infusion to dabigatran: Discontinue heparin infusion and initiate dabigatran at the time of discontinuance.1 1164
Transitioning to Other Anticoagulant Therapy
Pediatric Patients
Transitioning from dabigatran to warfarin: in patients with eGFR (Schwartz) ≥50 mL/minute per 1.73 m2, begin warfarin 3 days before discontinuing dabigatran.1 1164 Dabigatran may affect INR; INR for monitoring warfarin is more reliable ≥2 days after dabigatran discontinuance.1 1164
Transitioning from dabigatran to parenteral anticoagulant: discontinue dabigatran and begin parenteral anticoagulant 12 hours after the last dose of dabigatran.1 1164
Adults
Transitioning from dabigatran to warfarin:
Initiate warfarin before discontinuing dabigatran.1 Dabigatran may affect INR; INR for monitoring warfarin is more reliable ≥2 days after dabigatran discontinuance.1
Clcr ≥50 mL/minute: begin warfarin 3 days before discontinuing dabigatran.1
Clcr 30–50 mL/minute: begin warfarin 2 days before discontinuing dabigatran.1
Clcr 15–30 mL/minute: begin warfarin 1 day before discontinuing dabigatran.1
Clcr <15 mL/minute: recommendations not available.1
Transitioning from dabigatran to parenteral anticoagulant:
Clcr ≥30 mL/minute: discontinue dabigatran and begin parenteral anticoagulant 12 hours after the last dose of dabigatran.1
Clcr <30 mL/minute: discontinue dabigatran and begin parenteral anticoagulant 24 hours after the last dose of dabigatran.1
Managing Anticoagulation in Patients Requiring Invasive Procedures
Withhold dabigatran prior to surgery or other invasive procedures if possible.1 If surgery cannot be delayed, weigh increased risk of bleeding against urgency of intervention.1
Consider withholding drug for longer periods in patients who may require complete hemostasis (e.g., prior to major surgery, spinal puncture, placement of spinal or epidural catheter or port).1
Consider resumption of anticoagulant therapy as soon as medically appropriate.1 1164
Pediatric Patients
Patients with eGFR (Schwartz) >80 mL/minute per 1.73 m2: withhold dabigatran beginning 24 hours prior to procedure.1 1164
Patients with eGFR (Schwartz) 50-80 mL/minute per 1.73 m2: withhold dabigatran beginning 48 hours prior to procedure.1 1164
Idarucizumab efficacy and safety in pediatric patients not established.1 1164
Adults
Clcr ≥50 mL/minute: withhold dabigatran beginning 1–2 days prior to procedure.1
Clcr <50 mL/minute: withhold dabigatran beginning 3–5 days prior to procedure.1
Idarucizumab can be used in case of emergency surgery or urgent procedures when reversal of the anticoagulant effect of dabigatran is needed.1 1040 Dabigatran therapy can be reinitiated 24 hours after administration of idarucizumab; consider reinitiation of dabigatran as soon as medically appropriate.1040 1052 1054
Special Populations
Hepatic Impairment
Manufacturer makes no specific dosage recommendations.1 1164
Renal Impairment
Embolism Associated with Atrial Fibrillation
Reduce dosage to 75 mg orally twice daily in adults with severe renal impairment (Clcr 15–30 mL/minute).1 For patients with a creatinine clearance <15 mL/minute or who are receiving hemodialysis, dosage recommendations cannot be provided.1
In adults with Clcr 30–50 mL/minute and receiving concomitant therapy with the P-gp inhibitors dronedarone or systemic ketoconazole, reduce dosage to 75 mg twice daily.1 Avoid such concomitant use in patients with severe renal impairment (Clcr 15–30 mL/minute).1 Avoid concomitant use of P-gp inhibitors in patients with Clcr <30 mL/minute.1
Venous Thromboembolism - Treatment and Secondary Prevention
Pediatric Patients: Avoid use in children with eGFR (Schwartz) <50 mL/minute per 1.73 m2 due to risk of increased drug exposure.1 1164 Discontinue in patients who develop acute renal failure while on therapy; consider an alternative anticoagulant.1
Adults: Manufacturer states that dosage recommendations cannot be provided for patients with Clcr ≤30 mL/minute or for those receiving dialysis.1 Discontinue in patients who develop acute renal failure while on therapy; consider an alternative anticoagulant.1
Avoid concomitant use of P-gp inhibitors in patients with Clcr <50 mL/minute.1
Thromboprophylaxis in Hip-Replacement Surgery
Dosage recommendations cannot be provided for adult patients with Clcr ≤30 mL/minute or for those receiving dialysis.1 Discontinue in patients who develop acute renal failure while on therapy; consider an alternative anticoagulant.1
Avoid concomitant use of P-gp inhibitors in patients with Clcr <50 mL/minute.1
Geriatric Patients
Manufacturer makes no specific dosage recommendations.1 1164
Cautions for Dabigatran
Contraindications
Warnings/Precautions
Warnings
Risk of Thrombosis Following Premature Discontinuance of Anticoagulation
Premature discontinuance in the absence of adequate alternative anticoagulation may increase risk of thromboembolic events.1 1164 (See Boxed Warning.)
When transitioning patients from one anticoagulant therapy to another, ensure continuous anticoagulation while minimizing risk of bleeding.83
Particular caution advised when switching from a DOAC to warfarin therapy because of warfarin's slow onset of action.83
If discontinuance of dabigatran required for reasons other than pathologic bleeding or completion of a course of therapy, consider coverage with an alternative anticoagulant.1 83 1164
Advise patients regarding importance of adhering to therapeutic regimen and on steps to take if doses are missed.1 1164
Spinal/Epidural Hematoma
Epidural or spinal hematoma reported with concurrent use of anticoagulants and neuraxial (spinal/epidural) anesthesia or spinal puncture procedures.1 1164 Such hematomas have resulted in neurologic injury, including long-term or permanent paralysis.1 1164 (See Boxed Warning.)
To reduce risk of bleeding with concurrent use of dabigatran and neuraxial anesthesia or spinal puncture, carefully consider pharmacokinetic (PK) profile of dabigatran in relation to timing of such procedures.1 1164
Frequently monitor for signs and symptoms of neurologic impairment (e.g., midline back pain, numbness/tingling or weakness in lower limbs, bowel or bladder dysfunction).1 1164 If neurologic compromise noted, diagnose and treat immediately; consider spinal cord decompression.1 1164
Carefully consider potential benefits versus risks of neuraxial intervention in patients who are currently receiving or will receive anticoagulants.1 1164
Other Warnings and Precautions
Bleeding
Risk of serious, potentially fatal, bleeding.1 1164 Promptly evaluate if any manifestations of blood loss occur during therapy.1 1164
Discontinue if active pathologic bleeding occurs.1 1164 However, should not readily discontinue anticoagulation for commonly occurring minor or “nuisance” bleeding.83
Risk of bleeding may be increased in patients with renal impairment or those receiving concomitant drugs that affect hemostasis (e.g., antiplatelet agents, heparin, thrombolytic therapy, chronic use of NSAIAs).1 1164 Overdosage also may lead to hemorrhagic complications.1 1164
Temporarily interrupt therapy prior to any elective surgery or other invasive procedure to reduce risk of bleeding.1 9 1164 If serious bleeding occurs, discontinue dabigatran and initiate appropriate treatment.1 1164
Idarucizumab is a specific reversal agent for dabigatran that is used in adults for life-threatening or uncontrolled bleeding or in patients who require emergency surgery/urgent procedures.1 1040 Idarucizumab can be used in conjunction with supportive measures (e.g., maintenance of adequate diuresis, mechanical compression, surgical hemostasis, volume replacement, blood products), which should be considered as medically appropriate.10 1040 1055
Idarucizumab efficacy and safety in pediatric patients not established.1 1164
Dabigatran can be dialyzed; however, results will likely vary depending on individual patient-specific characteristics.1 10 46 1164
Consider use of procoagulant reversal agents such as anti-inhibitor coagulant complex (also known as activated prothrombin complex concentrate) or recombinant factor VIIa for immediate reversal of anticoagulation if idarucizumab not available.1 10 44 46 47
Protamine sulfate and vitamin K not expected to be effective.1 10 1164 Consider use of platelet concentrates in case of thrombocytopenia or if long-acting antiplatelet drugs have been used.1
If overdosage occurs, may consider early (e.g., within 1–2 hours) use of activated charcoal.10
Patients with Prosthetic Heart Valves
Contraindicated in patients with mechanical prosthetic heart valves.1 49 1164
Increased risk of thromboembolic events (valve thrombosis, stroke, TIA, MI) and major bleeding (mainly postoperative pericardial effusions) with dabigatran compared with warfarin therapy.1 49 88 1164
Not generally recommended in patients with other forms of valvular heart disease, including those with bioprosthetic heart valves.1 49 1164
Drugs Affecting P-glycoprotein Transport
Avoid concurrent dabigatran with P-glycoprotein transport inducers (e.g., rifampin) due to reduced exposure to dabigatran.1 1164
P-glycoprotein transport inhibitors (e.g., dronedarone, systemic ketoconazole) may increase systemic exposure to dabigatran in patients with renal impairment; dosage reduction or avoidance of such concomitant therapy may be necessary.1
Thrombosis Risk in Triple Positive Antiphospholipid Syndrome
Risk of recurrent thrombotic events in patients with triple-positive antiphospholipid syndrome (APS) (i.e., positive for lupus anticoagulant, anticardiolipin, and anti-beta 2-glycoprotein I antibodies); use not recommended in these patients.1 1164
Specific Populations
Pregnancy
No adequate data in pregnant women; increased maternal bleeding observed in animals.1 1164
Use during labor and delivery in women receiving neuraxial anesthesia may result in epidural or spinal hematomas.1 1164 Consider use of a shorter-acting anticoagulant as delivery approaches.1 Monitor for increased bleeding in the neonate.1 1164
Lactation
Distributed into milk in rats; not known whether distributed into human milk.1 1164
Females and Males of Reproductive Potential
Assess for increased risk of bleeding potentially requiring surgical intervention in females of reproductive potential and those with abnormal uterine bleeding.1 1164
Pediatric Use
Safety and efficacy of dabigatran for VTE treatment and reduction in risk of recurrent VTE have been established in pediatric patients <12 years of age (oral pellets) and pediatric patients 8 to <18 years of age (oral capsules).1 1164
Safety and efficacy not established in pediatric patients for other indications.1 1164
Geriatric Use
Risk of stroke and bleeding increases with age, but risk-benefit profile is favorable in all age groups.1
Hepatic Impairment
Large interpatient variability , but no consistent change in exposure or pharmacodynamic (PD) response observed in adults with moderate hepatic impairment (Child-Pugh class B).1 15 1164 Pediatric patients with active liver disease were excluded from the DIVERSITY trial.1166 1167
Renal Impairment
Primarily eliminated renally.1 1164 Exposure (AUC), half-life, and anticoagulant effects are increased in patients with renal impairment.1 1164 Evaluate renal function prior to initiating therapy and periodically thereafter when clinically indicated.1
Dosage adjustments in adults may be necessary depending on degree of renal impairment and indication for use.1
Not evaluated in pediatric patients with eGFR <50 mL/minute per 1.73 m2; avoid use in these patients.1164
Hemodialysis can remove dabigatran.1 1164
Common Adverse Effects
Adverse effects (>15%): GI adverse reactions, bleeding.1 1164
Drug Interactions
Does not inhibit or induce, and is not a substrate for, CYP isoenzymes.1 13 1164
Substrate for the P-glycoprotein (P-gp) transport system.1 1164
No clinical drug interaction studies have been conducted in pediatric subjects.1 1164
Drugs Affecting or Metabolized by Hepatic Microsomal Enzymes
Pharmacokinetic interactions with drugs metabolized by CYP isoenzymes unlikely.1 2 6 13 1164
Drugs Affecting P-glycoprotein Transport
P-gp inducers: Potential PK interaction (reduced dabigatran exposure); avoid concomitant use.1 1164
P-gp inhibitors: Potential PK interaction (increased dabigatran exposure).1 1164 In patients with atrial fibrillation, the Anticoagulation Forum recommends avoiding use of dabigatran in patients with Clcr <30 mL/minute who are taking P-gp inhibitors.1168 In the VTE setting, these experts recommend avoiding use of dabigatran in patients with a Clcr <50 mL/minute who are taking P-glycoprotein inhibitors.1168
Drugs Affecting Hemostasis
Potential increased risk of hemorrhage.1 1164 Promptly evaluate any manifestations of bleeding.1 1164
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Amiodarone |
Increased dabigatran concentrations and AUC; increased renal clearance of dabigatran1 No meaningful alteration of amiodarone pharmacokinetics1 |
Nonvalvular atrial fibrillation: Avoid concomitant use in patients with severe renal impairment (Clcr 15–30 mL/minute)1 Treatment or secondary prevention of venous thromboembolism: Avoid concomitant use in patients with Clcr <50 mL/minute1 Thromboprophylaxis following hip-replacement surgery: Avoid concomitant use in patients with Clcr <50 mL/minute1 Increased renal clearance of dabigatran may persist after amiodarone discontinuance due to long amiodarone half-life1 |
|
Anticoagulants, other |
Increased risk of bleeding1 |
Monitor for bleeding manifestations1 |
|
Aspirin |
Potential increased risk of bleeding with chronic NSAIA use1 |
Monitor for bleeding manifestations1 Large clinical trial in patients with atrial fibrillation demonstrated a 2-fold increase in major bleeding events/year with concomitant aspirin and dabigatran; similar to observed increased risk with concurrent aspirin and warfarin6 |
|
Atorvastatin |
||
|
Clarithromycin |
Nonvalvular atrial fibrillation: Avoid concomitant use in patients with severe renal impairment (Clcr 15–30 mL/minute)1 Treatment or secondary prevention of venous thromboembolism: Avoid concomitant use in patients with Clcr <50 mL/minute1 Thromboprophylaxis following hip-replacement surgery: Avoid concomitant use in patients with Clcr <50 mL/minute1 |
|
|
Clopidogrel |
Potentially increased dabigatran concentrations and AUC6 1043 |
Monitor for bleeding manifestations1 Large clinical trial in patients with atrial fibrillation demonstrated a 2-fold increase in major bleeding events/year with concomitant clopidogrel and dabigatran; similar to observed increased risk with concurrent clopidogrel and warfarin6 |
|
Diclofenac |
Pharmacokinetic interaction unlikely1 6 Potentially increased risk of bleeding with chronic NSAIA use1 |
Monitor for bleeding manifestations1 |
|
Digoxin |
||
|
Dronedarone |
Increased systemic exposure to dabigatran; lesser degree of increase when dronedarone administered 2 hours after dabigatran1 |
Nonvalvular atrial fibrillation: Reduce dosage to 75 mg twice daily in patients with moderate renal impairment (Clcr 30–50 mL/minute); avoid concomitant use in patients with severe renal impairment (Clcr 15–30 mL/minute)1 Treatment or secondary prevention of venous thromboembolism: Avoid concomitant use in patients with Clcr <50 mL/minute1 Thromboprophylaxis following hip-replacement surgery: Separate administration of dabigatran and dronedarone by several hours in patients with Clcr ≥50 mL/minute; avoid concomitant use in patients with Clcr <50 mL/minute1 |
|
Enoxaparin |
Increased risk of bleeding1 No alteration in dabigatran systemic exposure or pharmacodynamic assessments (i.e., aPTT, ECT, diluted thrombin time [dTT]) when dabigatran started 24 hours after last dose of enoxaparin1048 |
Monitor for bleeding manifestations1 |
|
Heparin |
Increased risk of bleeding1 |
Monitor for bleeding manifestations1 |
|
Ketoconazole |
Increased dabigatran concentrations and AUC1 |
Nonvalvular atrial fibrillation: Reduce dosage to 75 mg twice daily in patients with moderate renal impairment (Clcr 30–50 mL/minute); avoid concomitant use in patients with severe renal impairment (Clcr 15–30 mL/minute)1 Treatment or secondary prevention of venous thromboembolism: Avoid concomitant use in patients with Clcr <50 mL/minute1 Thromboprophylaxis following hip-replacement surgery: Separate administration of dabigatran and ketoconazole by several hours in patients with Clcr ≥50 mL/minute; avoid concomitant use in patients with Clcr <50 mL/minute1 |
|
NSAIAs |
Increased risk of bleeding with chronic NSAIA use1 |
Monitor for bleeding manifestations1 |
|
Pantoprazole |
||
|
Quinidine |
Increased dabigatran concentrations and AUC1 |
Nonvalvular atrial fibrillation: Avoid concomitant use in patients with severe renal impairment (Clcr 15–30 mL/minute)1 Treatment or secondary prevention of venous thromboembolism: Avoid concomitant use in patients with Clcr <50 mL/minute1 Thromboprophylaxis following hip-replacement surgery: Avoid concomitant use in patients with Clcr <50 mL/minute1 |
|
Rifampin |
Avoid concurrent use1 |
|
|
Thrombolytic agents |
Increased risk of bleeding1 |
Monitor for bleeding manifestations1 |
|
Ticagrelor |
Increased steady-state peak plasma concentration and AUC of dabigatran; magnitude of increase dependent on dose and timing of dabigatran administration1 1046 |
Increased bleeding risk with concurrent use.1 Nonvalvular atrial fibrillation: Avoid concomitant use in patients with severe renal impairment (Clcr 15–30 mL/minute)1 Treatment or secondary prevention of venous thromboembolism: Avoid concomitant use in patients with Clcr <50 mL/minute1 Thromboprophylaxis following hip-replacement surgery: Avoid concomitant use in patients with Clcr <50 mL/minute1 |
|
Verapamil |
Potentially increased dabigatran concentrations and AUC1 1044 Interaction dependent on verapamil formulation and timing of administration; verapamil immediate release given 1 hour prior to dabigatran increased dabigatran AUC 2.4-fold, while verapamil given 2 hours after dabigatran had negligible effects1043 1044 |
Nonvalvular atrial fibrillation: Avoid concomitant use in patients with severe renal impairment (Clcr 15–30 mL/minute)1 Treatment or secondary prevention of venous thromboembolism: Avoid concomitant use in patients with Clcr <50 mL/minute1 Thromboprophylaxis following hip-replacement surgery: Avoid concomitant use in patients with Clcr <50 mL/minute1 |
|
Warfarin |
Increased risk of bleeding1 |
INR for monitoring warfarin more accurate ≥2 days after discontinuing dabigatran; monitor for bleeding manifestations1 |
Dabigatran Pharmacokinetics
Dabigatran etexilate mesylate is absorbed as the dabigatran etexilate ester and hydrolyzed to the active moiety, dabigatran, by esterases in plasma and the liver.1 7 13 1164
Dabigatran undergoes conjugation to acyl glucuronides that have similar pharmacologic activity to dabigatran and account for approximately 20% of the total plasma dabigatran concentration.1 11 12 13 The PK of dabigatran are generally described in terms of total plasma dabigatran concentrations, which includes the major acyl glucuronide metabolites.1 11 Dabigatran exhibits linear, dose-dependent PK.1
Absorption
Bioavailability
Absolute bioavailability of dabigatran following oral administration of dabigatran etexilate approximately 3–7%.1
Oral absorption is formulation-dependent.1 1164 The oral pellet formulation is 37% more bioavailable in healthy adults compared to the capsule.1 1164
Available in capsules and oral pellets and relative bioavailability between dosage forms is age-dependent.1 1164
Onset
Peak plasma concentration attained approximately 1–2 hours following oral administration.1 11 13 Maximal effects on coagulation assays expected within 2 hours of administration; such effects correlate with peak plasma concentrations.1 11 13 Similar PK/PD effects on coagulation assays observed in pediatric patients.1 1164
Duration
Effects on anticoagulation assays decline by approximately 50% at 12 hours after administration.11
Food
High-fat meal delays time to peak plasma concentration by 2 hours but does not affect bioavailability.1
Special Populations
Similar PK/PD effects on coagulation assays observed in pediatric patients.1 1164
When dabigatran was administered 1–3 hours after completing hip arthroplasty, time to peak plasma concentrations was delayed to 6 hours but returned to normal day after surgery.2 12 There was no effect on AUC.2 12
In adult patients with mild, moderate, or severe renal impairment, AUC estimated to be increased 1.5-, 3.2-, or 6.3-fold respectively; peak plasma concentrations increased 1.1-, 1.7-, or 2.1-fold, respectively.1 14
Distribution
Extent
Not known whether dabigatran distributes into human milk; distributed into milk in rats.1 1164
Plasma Protein Binding
Elimination
Metabolism
Dabigatran etexilate is a prodrug of dabigatran;2 rapidly absorbed following oral administration and hydrolyzed in the plasma and liver to dabigatran, the active moiety.1 11 1164
Elimination Route
Bioavailable dabigatran excreted principally (80%) in urine as unchanged drug.1 13 1164 Approximately 86% of total oral dose is eliminated in the feces.1 1164
Removed by dialysis; redistribution may occur.1 10 46 1164
Half-life
Oral capsules: 12–17 hours in healthy adults and 12–14 hours in pediatric patients.1 11
Oral pellets: 9–11 hours in pediatric patients.1164
Special Populations
In adult patients with mild, moderate, or severe renal impairment, plasma half-life averages 15, 18, or 27 hours, respectively.1 1164
In patients with moderate hepatic impairment (Child-Pugh class B), large interpatient variability apparent, but no consistent change in exposure or PD response.1 15 1164
Stability
Storage
Oral
Capsules
20–25°C (excursions permitted to 15–30°C).1 Store in original package (i.e., bottles or blister pack) to protect from moisture.1
Once bottle is opened, manufacturer recommends that drug be used within 4 months.1 Keep bottle tightly closed.1
Oral Pellets
20–25°C (excursions permitted to 15–30°C).1164 Store in original aluminum package to protect from moisture.1164
Do not open the packets until ready for use.1164
Use the packets within 6 months of opening the aluminum bag.1164
Actions
-
Selective, competitive, reversible direct thrombin inhibitor.2 12
Prevents thrombus formation by binding free and clot-bound thrombin, thereby inhibiting the conversion of fibrinogen to fibrin.1 2 12 1164 Also inhibits thrombin-mediated platelet aggregation.1 2 12 1164 Dabigatran etexilate mesylate is absorbed as the dabigatran etexilate ester and hydrolyzed to the active moiety, dabigatran, by esterases in plasma and the liver.1 13 7 1164
-
Metabolized to several acyl glucuronides with similar activity as dabigatran.1 11 1164
-
Prolongs dTT and ECT linearly over the range of therapeutic plasma concentrations.1 10 11 1164
-
Prolongs aPTT in a curvilinear manner.1 10 11 1164 INR may be elevated, but is not a reliable assessment of dabigatran activity.1 10 11 1164
Advice to Patients
-
Instruct patients to take dabigatran exactly as prescribed and to not discontinue therapy without first consulting a clinician.1 1164
-
Inform patients that the oral capsule and pellets are not interchangeable; do not substitute different dosage forms on a mg-to-mg basis.1 1164 Consult with a health care provider to make sure the proper dosage form and dosage are used. 1 1164
-
Advise patients of the importance of having an adult caregiver administer dabigatran to pediatric patients. 1 1164
-
Instruct patients to take a missed dose (capsules or oral pellets) as soon as it is remembered on the same day, but only if it can be taken at least 6 hours prior to the next scheduled dose.1 1164 Do not take 2 doses at the same time to make up for a missed dose. 1 1164
-
Inform patients that they may bruise and/or bleed more easily and that a longer than normal time may be required to stop bleeding when taking dabigatran; advise patients on how to recognize signs and symptoms of bleeding. 1 1164
-
Advise patients to inform their clinicians immediately if any unusual bleeding or bruising, including menstrual or vaginal bleeding that is heavier than normal, occurs during therapy. 1 1164
-
Dabigatran is not for patients with artificial heart valves; advise patients to inform their health care provider if they had or will have heart valve surgery. 1 1164
-
Dabigatran is not recommended for use in patients with antiphospholipid syndrome (APS), especially with positive triple antibody testing; advise patients to inform their health care provider if they have APS. 1 1164
-
Inform patients about the risk of adverse GI reactions.1 1164 Advise patients to consult their healthcare provider if they experience dyspepsia, burning, nausea, abdominal pain/discomfort, epigastric discomfort, or indigestion.1 1164
-
Advise patients who have had neuraxial anesthesia or spinal puncture to monitor for manifestations of spinal or epidural hematoma (e.g., numbness or weakness of legs, bowel or bladder dysfunction), particularly if they are receiving concomitant nonsteroidal anti-inflammatory agents (NSAIAs), platelet inhibitors, or other anticoagulants; inform patients to seek emergency medical attention if any of these symptoms occur. 1 1164
-
Advise patients to inform their clinicians (e.g., physicians, dentists) that they are receiving dabigatran therapy before scheduling any surgery or invasive procedures, including dental procedures. 1 1164
-
Advise patients to swallow dabigatran capsules whole with a full glass of water, without opening, chewing, or otherwise emptying the contents of the capsule.1 Advise patients to inform their health care provider if they are unable to swallow the capsule whole.1 Do not sprinkle contents of capsules on food or into a beverage.1
-
Inform patients of special storage and handling requirements for dabigatran capsules.1 36 Store the drug capsules only in the original container (bottle or blister package) and protect from moisture; do not store capsules in pill boxes or organizers.1 36 Remove only one capsule from the bottle at a time, right before use, and close the bottle tightly immediately after use.1 36 When more than one bottle is dispensed, advise the patient to open only one bottle at a time.1 For blister packages of capsules, do not open or puncture the blister until time of use.36 The manufacturer states that dabigatran capsules should be used within 4 months after the bottle is first opened.1
-
Advise the adult caregiver on the proper administration of dabigatran oral pellets.1164 The oral pellets should be sprinkled on baby rice cereal (prepared with water), mashed carrots, apple sauce, or mashed bananas, or taken with apple juice.1164 Do not mix with any other food or liquid.1164 Do not mix the oral pellets with milk, milk products, or foods that contain milk.1164 The oral pellets should be administered before meals to help ensure that the full dose is taken.1164
-
Advise the caregiver to administer the oral pellets right away or within 30 minutes after mixing; discard oral pellets that have been in contact with soft food or apple juice for more than 30 minutes.1164 If the child only takes part of their oral pellet dose, do not give another dose at that time; administer the next dose at the regularly scheduled time, about 12 hours later.1164
-
Advise caregivers to not use an oral syringe or feeding tube to administer the oral pellets.1164
-
Inform caregivers of special storage and handling requirements for dabigatran oral pellets.1164 Oral pellet packets are dispensed in an aluminum bag with a desiccant.1164 Keep the oral pellet packets in the original aluminum bag to keep them dry.1164 Remove only one packet at a time.1164 Do not open the oral pellet packet until ready to administer the dose.1164 After opening the aluminum bag, oral pellets must be used within 6 months.1164
-
Advise females to inform their clinician if they are or plan to become pregnant or plan to breast-feed.1 1164
-
Advise patients to inform their clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary and herbal supplements, as well as any concomitant illnesses.1 1164
-
Advise patients of other important precautionary information.1 1164 (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
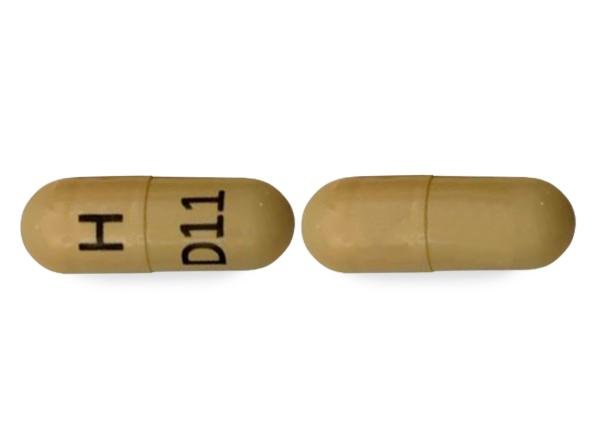
Oral |
Capsules |
75 mg (of dabigatran etexilate) |
Pradaxa |
Boehringer Ingelheim |
|
110 mg (of dabigatran etexilate) |
Pradaxa |
Boehringer Ingelheim |
||
|
150 mg (of dabigatran etexilate) |
Pradaxa |
Boehringer Ingelheim |
||
|
Pellets |
20 mg (of dabigatran etexilate) |
Pradaxa |
Boehringer Ingelheim |
|
|
30 mg (of dabigatran etexilate) |
Pradaxa |
Boehringer Ingelheim |
||
|
40 mg (of dabigatran etexilate) |
Pradaxa |
Boehringer Ingelheim |
||
|
50 mg (of dabigatran etexilate) |
Pradaxa |
Boehringer Ingelheim |
||
|
110 mg (of dabigatran etexilate) |
Pradaxa |
Boehringer Ingelheim |
||
|
150 mg (of dabigatran etexilate) |
Pradaxa |
Boehringer Ingelheim |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions March 22, 2023. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
1. Boehringer Ingelheim. Pradaxa (dabigatran etexilate mesylate) capsules prescribing information. Ridgefield, CT. 2021 Jun.
2. Siddiqui FM, Qureshi AI. Dabigatran etexilate, a new oral direct thrombin inhibitor, for stroke prevention in patients with atrial fibrillation. Expert Opin Pharmacother. 2010; 11:1403-11. https://pubmed.ncbi.nlm.nih.gov/20446854
3. Connolly SJ, Ezekowitz MD, Yusuf S et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009; 361:1139-51. https://pubmed.ncbi.nlm.nih.gov/19717844
4. Connolly SJ, Ezekowitz MD, Yusuf S et al. Newly identified events in the RE-LY trial. N Engl J Med. 2010; 363:1875-6. https://pubmed.ncbi.nlm.nih.gov/21047252
5. Ezekowitz MD, Connolly S, Parekh A et al. Rationale and design of RE-LY: randomized evaluation of long-term anticoagulant therapy, warfarin, compared with dabigatran. Am Heart J. 2009; 157:205-10.e2. https://pubmed.ncbi.nlm.nih.gov/19185626
6. Boehringer Ingelheim. Dabigatran advisory committee briefing document. Available at FDA website. http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/CardiovascularandRenalDrugsAdvisoryCommittee/UCM226009.pdf
7. Nutescu E, Chuatrisorn I, Hellenbart E. Drug and dietary interactions of warfarin and novel oral anticoagulants: an update. J Thromb Thrombolysis. 2011; 31:326-43. https://pubmed.ncbi.nlm.nih.gov/21359645
9. Stangier J, Rathgen K, Stähle H et al. Coadministration of dabigatran etexilate and atorvastatin: assessment of potential impact on pharmacokinetics and pharmacodynamics. Am J Cardiovasc Drugs. 2009; 9:59-68. https://pubmed.ncbi.nlm.nih.gov/19178132
10. van Ryn J, Stangier J, Haertter S et al. Dabigatran etexilate--a novel, reversible, oral direct thrombin inhibitor: interpretation of coagulation assays and reversal of anticoagulant activity. Thromb Haemost. 2010; 103:1116-27. https://pubmed.ncbi.nlm.nih.gov/20352166
11. Stangier J, Rathgen K, Stähle H et al. The pharmacokinetics, pharmacodynamics and tolerability of dabigatran etexilate, a new oral direct thrombin inhibitor, in healthy male subjects. Br J Clin Pharmacol. 2007; 64:292-303. https://pubmed.ncbi.nlm.nih.gov/17506785 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2000643/
12. Stangier J. Clinical pharmacokinetics and pharmacodynamics of the oral direct thrombin inhibitor dabigatran etexilate. Clin Pharmacokinet. 2008; 47:285-95. https://pubmed.ncbi.nlm.nih.gov/18399711
13. Blech S, Ebner T, Ludwig-Schwellinger E et al. The metabolism and disposition of the oral direct thrombin inhibitor, dabigatran, in humans. Drug Metab Dispos. 2008; 36:386-99. https://pubmed.ncbi.nlm.nih.gov/18006647
14. Stangier J, Rathgen K, Stähle H et al. Influence of renal impairment on the pharmacokinetics and pharmacodynamics of oral dabigatran etexilate: an open-label, parallel-group, single-centre study. Clin Pharmacokinet. 2010; 49:259-68. https://pubmed.ncbi.nlm.nih.gov/20214409
15. Stangier J, Stähle H, Rathgen K et al. Pharmacokinetics and pharmacodynamics of dabigatran etexilate, an oral direct thrombin inhibitor, are not affected by moderate hepatic impairment. J Clin Pharmacol. 2008; 48:1411-9. https://pubmed.ncbi.nlm.nih.gov/18827075
18. Wann LS, Curtis AB, Ellenbogen KA et al. 2011 ACCF/AHA/HRS Focused Update on the Management of Patients With Atrial Fibrillation (Update on Dabigatran): A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2011; 123:1144-50. https://pubmed.ncbi.nlm.nih.gov/21321155
20. Mosca L, Benjamin EJ, Berra K et al. Effectiveness-based guidelines for the prevention of cardiovascular disease in women–2011 update: a guideline from the American Heart Association. J Am Coll Cardiol. 2011; 57:1404-23. https://pubmed.ncbi.nlm.nih.gov/21388771 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3124072/
21. Cairns JA, Connolly S, McMurtry S et al. Canadian cardiovascular society atrial fibrillation guidelines 2010: prevention of stroke and systemic thromboembolism in atrial fibrillation and flutter. Can J Cardiol. 2011 Jan-Feb; 27:74-90.
23. US Food and Drug Administration. Center for Drug Evaluation and Research. Application number: 22-512: Summary review. From FDA website. Accessed 2022 Nov 3. http://www.accessdata.fda.gov/drugsatfda_docs/nda/2010/022512Orig1s000SumR.pdf
28. Healey JS, Eikelboom J, Wallentin L et al. Effect of age and renal function on the risks of stroke and major bleeding with dabigatran compared to warfarin: An analysis from the RE-LY study. J Am Coll Cardiol. 2010; 55:A4.E37. Abstract.
30. Schwartz NE, Albers GW. Dabigatran challenges warfarin’s superiority for stroke prevention in atrial fibrillation. Stroke. 2010; 41:1307-9. https://pubmed.ncbi.nlm.nih.gov/20395603
31. Raju NC, Hankey GJ. Dabigatran etexilate in people with atrial fibrillation. BMJ. 2010; 341:c3784. https://pubmed.ncbi.nlm.nih.gov/20671015
32. Gage BF. Can we rely on RE-LY?. N Engl J Med. 2009; 361:1200-2. https://pubmed.ncbi.nlm.nih.gov/19717843
33. Lane DA, Lip GY. Dabigatran in atrial fibrillation: balancing secondary stroke prevention against bleeding risk. Lancet Neurol. 2010; 9:1140-2. https://pubmed.ncbi.nlm.nih.gov/21059485
34. Stangier J, Stähle H, Rathgen K et al. Pharmacokinetics and pharmacodynamics of the direct oral thrombin inhibitor dabigatran in healthy elderly subjects. Clin Pharmacokinet. 2008; 47:47-59. https://pubmed.ncbi.nlm.nih.gov/18076218
35. Beasley BN, Unger EF, Temple R. Anticoagulant options—Why the FDA approved a higher but not a lower dose of dabigatran. N Engl J Med. 2011; 364; 19:1788-90. Editorial. https://pubmed.ncbi.nlm.nih.gov/21488759
36. US Food and Drug Administration, Center for Drug Evaluation and Research. FDA drug safety communication: special storage and handling requirements must be followed for Pradaxa (dabigatran etexilate mesylate) capsules. Rockville MD: Food and Drug Administration; 2017 Aug 4. Available from FDA website. Accessed 2022 Nov 3. http://www.fda.gov/Drugs/DrugSafety/ucm248746.htm
40. Eerenberg ES, Kamphuisen PW, Sijpkens MK et al. Reversal of Rivaroxaban and Dabigatran by Prothrombin Complex Concentrate: A Randomized, Placebo-Controlled, Crossover Study in Healthy Subjects. Circulation. 2011; :1573-9. https://pubmed.ncbi.nlm.nih.gov/21900088
44. Miyares MA, Davis K. Newer oral anticoagulants: a review of laboratory monitoring options and reversal agents in the hemorrhagic patient. Am J Health Syst Pharm. 2012; 69:1473-84. https://pubmed.ncbi.nlm.nih.gov/22899742
46. Warkentin TE, Margetts P, Connolly SJ et al. Recombinant factor VIIa (rFVIIa) and hemodialysis to manage massive dabigatran-associated postcardiac surgery bleeding. Blood. 2012; 119:2172-4. https://pubmed.ncbi.nlm.nih.gov/22383791
47. Marlu R, Hodaj E, Paris A et al. Effect of non-specific reversal agents on anticoagulant activity of dabigatran and rivaroxaban: a randomised crossover ex vivo study in healthy volunteers. Thromb Haemost. 2012; 108:217-24. https://pubmed.ncbi.nlm.nih.gov/22627883
48. Dager WE, Gosselin RC, Kitchen S et al. Dabigatran effects on the international normalized ratio, activated partial thromboplastin time, thrombin time, and fibrinogen: a multicenter, in vitro study. Ann Pharmacother. 2012; 46:1627-36. https://pubmed.ncbi.nlm.nih.gov/23232017
49. Food and Drug Administration. FDA Drug Safety Communication: Pradaxa (dabigatran etexilate mesylate) should not be used in patients with mechanical prosthetic heart valves. Rockville, MD; 2018 Feb 13. From FDA website. http://www.fda.gov/Drugs/DrugSafety/ucm332912.htm
50. Van de Werf F, Brueckmann M, Connolly SJ et al. A comparison of dabigatran etexilate with warfarin in patients with mechanical heart valves: THE Randomized, phase II study to evaluate the safety and pharmacokinetics of oral dabigatran etexilate in patients after heart valve replacement (RE-ALIGN). Am Heart J. 2012; 163:931-937.e1. https://pubmed.ncbi.nlm.nih.gov/22709744
74. Schulman S, Kearon C, Kakkar AK et al. Dabigatran versus warfarin in the treatment of acute venous thromboembolism. N Engl J Med. 2009; 361:2342-52. https://pubmed.ncbi.nlm.nih.gov/19966341
75. Schulman S, Kakkar AK, Goldhaber SZ et al. Treatment of acute venous thromboembolism with dabigatran or warfarin and pooled analysis. Circulation. 2014; 129:764-72. https://pubmed.ncbi.nlm.nih.gov/24344086
76. Schulman S, Kearon C, Kakkar AK et al. Extended use of dabigatran, warfarin, or placebo in venous thromboembolism. N Engl J Med. 2013; 368:709-18. https://pubmed.ncbi.nlm.nih.gov/23425163
77. Connors JM. Extended treatment of venous thromboembolism. N Engl J Med. 2013 Feb 21; 368(8):767-9. Editorial.
80. January CT, Wann LS, Alpert JS et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014; 64:e1-76. https://pubmed.ncbi.nlm.nih.gov/24685669
81. Meschia JF, Bushnell C, Boden-Albala B et al. Guidelines for the primary prevention of stroke: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014; 45:3754-832. https://pubmed.ncbi.nlm.nih.gov/25355838 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5020564/
82. Kleindorfer DO, Towfighi A, Chaturvedi S et al. 2021 Guideline for the Prevention of Stroke in Patients With Stroke and Transient Ischemic Attack: A Guideline From the American Heart Association/American Stroke Association. Stroke. 2021; 52:e364-e467. https://pubmed.ncbi.nlm.nih.gov/34024117
83. Heidbuchel H, Verhamme P, Alings M et al. EHRA practical guide on the use of new oral anticoagulants in patients with non-valvular atrial fibrillation: executive summary. Eur Heart J. 2013; 34:2094-106. https://pubmed.ncbi.nlm.nih.gov/23625209
84. Senoo K, Lip GY. Comparative efficacy and safety of the non-vitamin K antagonist oral anticoagulants for patients with nonvalvular atrial fibrillation. Semin Thromb Hemost. 2015; 41:146-53. https://pubmed.ncbi.nlm.nih.gov/25682085
85. Skjøth F, Larsen TB, Rasmussen LH et al. Efficacy and safety of edoxaban in comparison with dabigatran, rivaroxaban and apixaban for stroke prevention in atrial fibrillation. An indirect comparison analysis. Thromb Haemost. 2014; 111:981-8. https://pubmed.ncbi.nlm.nih.gov/24577485
87. January CT, Wann LS, Calkins H et al. 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/ American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society in Collaboration With the Society of Thoracic Surgeons. Circulation. 2019; 140:e125-e151. https://pubmed.ncbi.nlm.nih.gov/30686041
88. Eikelboom JW, Connolly SJ, Brueckmann M et al. Dabigatran versus warfarin in patients with mechanical heart valves. N Engl J Med. 2013; 369:1206-14. https://pubmed.ncbi.nlm.nih.gov/23991661
89. Mega JL. A new era for anticoagulation in atrial fibrillation. N Engl J Med. 2011; 365:1052-4. https://pubmed.ncbi.nlm.nih.gov/21870977
989. Hindricks G, Potpara T, Dagres N et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Develop with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2021; 42:373-498. https://pubmed.ncbi.nlm.nih.gov/32860505
990. Furie KL, Kasner SE, Adams RJ et al. Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack: a guideline for healthcare professionals from the american heart association/american stroke association. Stroke. 2011; 42:227-76. https://pubmed.ncbi.nlm.nih.gov/20966421
999. Fuster V, Rydén LE, Cannom DS et al. 2011 ACCF/AHA/HRS focused updates incorporated into the ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2011; 123:e269-367.
1003. Falck-Ytter Y, Francis CW, Johanson NA et al. Prevention of VTE in orthopedic surgery patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012; 141(2 Suppl):e278S-325S. https://pubmed.ncbi.nlm.nih.gov/22315265 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3278063/
1005. Kearon C, Akl EA, Ornelas J, Blaivas A, Jimenez D, Bounameaux H, Huisman M, King CS, Morris TA, Sood N, Stevens SM, Vintch JRE, Wells P, Woller SC, Moores L. Antithrombotic Therapy for VTE Disease: CHEST Guideline and Expert Panel Report. Chest. 2016 Feb;149(2):315-352. Epub 2016 Jan 7. Erratum in: Chest. 2016 Oct;150(4):988. https://pubmed.ncbi.nlm.nih.gov/26867832
1006. Ortel TL, Neumann I, Ageno W, Beyth R, Clark NP, Cuker A, Hutten BA, Jaff MR, Manja V, Schulman S, Thurston C, Vedantham S, Verhamme P, Witt DM, D Florez I, Izcovich A, Nieuwlaat R, Ross S, J Schünemann H, Wiercioch W, Zhang Y, Zhang Y. American Society of Hematology 2020 guidelines for management of venous thromboembolism: treatment of deep vein thrombosis and pulmonary embolism. Blood Adv. 2020 Oct 13;4(19):4693-4738. https://pubmed.ncbi.nlm.nih.gov/33007077 https://www.ncbi.nlm.nih.gov/pmc/articles/PMCPMC7556153/
1007. Lip GYH, Banerjee A, Boriani G et al. Antithrombotic Therapy for Atrial Fibrillation: CHEST Guideline and Expert Panel Report. Chest. 2018; 154:1121-1201. https://pubmed.ncbi.nlm.nih.gov/30144419
1008. Burnett AE, Mahan CE, Vazquez SR, Oertel LB, Garcia DA, Ansell J. Guidance for the practical management of the direct oral anticoagulants (DOACs) in VTE treatment. J Thromb Thrombolysis. 2016 Jan;41(1):206-32 https://pubmed.ncbi.nlm.nih.gov/26780747 https://www.ncbi.nlm.nih.gov/pmc/articles/PMCPMC4715848/
1012. Bates SM, Greer IA, Middeldorp S et al. VTE, thrombophilia, antithrombotic therapy, and pregnancy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012; 141(2 Suppl):e691S-736S. https://pubmed.ncbi.nlm.nih.gov/22315276 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3278054/
1017. Bushnell C, McCullough LD, Awad IA et al; on behalf of the American Heart Association Stroke Council, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Council for High Blood Pressure Research. Guidelines for the prevention of stroke in women: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014; 45:1545-88. https://pubmed.ncbi.nlm.nih.gov/24503673
1030. Stewart RA. Clinical trials of direct thrombin and factor Xa inhibitors in atrial fibrillation. Curr Opin Cardiol. 2011; 26:294-9. https://pubmed.ncbi.nlm.nih.gov/21537165
1040. Boehringer Ingelheim. Praxbind (idarucizumab) injection prescribing information. Ridgefield, CT; 2021 Oct.
1041. Eriksson BI, Dahl OE, Rosencher N et al. Dabigatran etexilate versus enoxaparin for prevention of venous thromboembolism after total hip replacement: a randomised, double-blind, non-inferiority trial. Lancet. 2007; 370:949-56. https://pubmed.ncbi.nlm.nih.gov/17869635
1042. Eriksson BI, Dahl OE, Huo MH et al. Oral dabigatran versus enoxaparin for thromboprophylaxis after primary total hip arthroplasty (RE-NOVATE II). A randomised, double-blind, non-inferiority trial. Thromb Haemost. 2011; 105:721-9. https://pubmed.ncbi.nlm.nih.gov/21225098
1043. US Food and Drug Administration. Center for Drug Evaluation and Research. Application number: 22-512: Clinical pharmacology and biopharmaceutics review(s). From FDA website. http://www.accessdata.fda.gov/drugsatfda_docs/nda/2010/022512Orig1s000ClinPharmR.pdf
1044. Härtter S, Sennewald R, Nehmiz G et al. Oral bioavailability of dabigatran etexilate (Pradaxa()) after co-medication with verapamil in healthy subjects. Br J Clin Pharmacol. 2013; 75:1053-62. https://pubmed.ncbi.nlm.nih.gov/22946890
1045. Härtter S, Koenen-Bergmann M, Sharma A et al. Decrease in the oral bioavailability of dabigatran etexilate after co-medication with rifampicin. Br J Clin Pharmacol. 2012; 74:490-500. https://pubmed.ncbi.nlm.nih.gov/22348256 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3477350/
1046. Boehringer Ingelheim. Pradaxa (dabigatran etexilate mesylate) capsules prescribing information. Ridgefield, CT. 2014 Aug.
1047. Härtter S, Sennewald R, Schepers C et al. Pharmacokinetic and pharmacodynamic effects of comedication of clopidogrel and dabigatran etexilate in healthy male volunteers. Eur J Clin Pharmacol. 2013; 69:327-39. https://pubmed.ncbi.nlm.nih.gov/22782539
1048. Clemens A, van Ryn J, Sennewald R et al. Switching from enoxaparin to dabigatran etexilate: pharmacokinetics, pharmacodynamics, and safety profile. Eur J Clin Pharmacol. 2012; 68:607-16. https://pubmed.ncbi.nlm.nih.gov/22252796 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3332339/
1049. Eriksson BI, Dahl OE, Rosencher N et al. Oral dabigatran etexilate vs. subcutaneous enoxaparin for the prevention of venous thromboembolism after total knee replacement: the RE-MODEL randomized trial. J Thromb Haemost. 2007; 5:2178-85. https://pubmed.ncbi.nlm.nih.gov/17764540
1050. RE-MOBILIZE Writing Committee, Ginsberg JS, Davidson BL et al. Oral thrombin inhibitor dabigatran etexilate vs North American enoxaparin regimen for prevention of venous thromboembolism after knee arthroplasty surgery. J Arthroplasty. 2009; 24:1-9. https://pubmed.ncbi.nlm.nih.gov/18534438
1051. Pollack CV, Reilly PA, Eikelboom J et al. Idarucizumab for Dabigatran Reversal. N Engl J Med. 2015; 373:511-20. https://pubmed.ncbi.nlm.nih.gov/26095746
1052. Miyares MA, Kuyumjian Y, Eaves S et al. Idarucizumab, a humanized, monoclonal antibody fragment for immediate reversal of dabigatran. J Pharm Pract. 2015; 28:548-54. https://pubmed.ncbi.nlm.nih.gov/26894245
1054. Eikelboom JW, Quinlan DJ, van Ryn J et al. Idarucizumab: The Antidote for Reversal of Dabigatran. Circulation. 2015; 132:2412-22. https://pubmed.ncbi.nlm.nih.gov/26700008
1055. Boehringer Ingelheim Pharmaceuticals, Inc. Pradaxa (dabigatran etexilate mesylate) management of medical emergency. From Pradaxa website. https://www.pradaxapro.com/pradaxa-reversal
1102. Key NS, Khorana AA, Kuderer NM et al. Venous Thromboembolism Prophylaxis and Treatment in Patients With Cancer: ASCO Clinical Practice Guideline Update. J Clin Oncol. 2020; 38:496-520. https://pubmed.ncbi.nlm.nih.gov/31381464
1103. Lyman GH, Carrier M, Ay C, Di Nisio M, Hicks LK, Khorana AA, Leavitt AD, Lee AYY, Macbeth F, Morgan RL, Noble S, Sexton EA, Stenehjem D, Wiercioch W, Kahale LA, Alonso-Coello P. American Society of Hematology 2021 guidelines for management of venous thromboembolism: prevention and treatment in patients with cancer. Blood Adv. 2021 Feb 23;5(4):927-974. Erratum in: Blood Adv. 2021 Apr 13;5(7):1953. PMID: 33570602; PMCID: PMC7903232.
1106. Stevens SM, Woller SC, Kreuziger LB, Bounameaux H, Doerschug K, Geersing GJ, Huisman MV, Kearon C, King CS, Knighton AJ, Lake E, Murin S, Vintch JRE, Wells PS, Moores LK. Antithrombotic Therapy for VTE Disease: Second Update of the CHEST Guideline and Expert Panel Report. Chest. 2021 Dec;160(6):e545-e608. Epub 2021 Aug 2. https://pubmed.ncbi.nlm.nih.gov/34352278
1107. Cohen AT, Hamilton M, Mitchell SA, Phatak H, Liu X, Bird A, Tushabe D, Batson S. Comparison of the Novel Oral Anticoagulants Apixaban, Dabigatran, Edoxaban, and Rivaroxaban in the Initial and Long-Term Treatment and Prevention of Venous Thromboembolism: Systematic Review and Network Meta-Analysis. PLoS One. 2015 Dec 30;10(12):e0144856. https://pubmed.ncbi.nlm.nih.gov/26716830 https://www.ncbi.nlm.nih.gov/pmc/articles/PMCPMC4696796/
1108. Mont MA, Jacobs JJ, Boggio LN, Bozic KJ, Della Valle CJ, Goodman SB, Lewis CG, Yates AJ Jr, Watters WC 3rd, Turkelson CM, Wies JL, Donnelly P, Patel N, Sluka P; AAOS. Preventing venous thromboembolic disease in patients undergoing elective hip and knee arthroplasty. J Am Acad Orthop Surg. 2011 Dec;19(12):768-76. https://pubmed.ncbi.nlm.nih.gov/22134209
1109. Anderson DR, Morgano GP, Bennett C, Dentali F, Francis CW, Garcia DA, Kahn SR, Rahman M, Rajasekhar A, Rogers FB, Smythe MA, Tikkinen KAO, Yates AJ, Baldeh T, Balduzzi S, Brozek JL, Ikobaltzeta IE, Johal H, Neumann I, Wiercioch W, Yepes-Nuñez JJ, Schünemann HJ, Dahm P. American Society of Hematology 2019 guidelines for management of venous thromboembolism: prevention of venous thromboembolism in surgical hospitalized patients. Blood Adv. 2019 Dec 10;3(23):3898-3944. https://pubmed.ncbi.nlm.nih.gov/31794602 https://www.ncbi.nlm.nih.gov/pmc/articles/PMCPMC6963238/
1125. Bates SM, Rajasekhar A, Middeldorp S, McLintock C, Rodger MA, James AH, Vazquez SR, Greer IA, Riva JJ, Bhatt M, Schwab N, Barrett D, LaHaye A, Rochwerg B. American Society of Hematology 2018 guidelines for management of venous thromboembolism: venous thromboembolism in the context of pregnancy. Blood Adv. 2018 Nov 27;2(22):3317-3359. doi: 10.1182/bloodadvances.2018024802. PMID: 30482767; PMCID: PMC6258928.
1126. American College of Obstetricians and Gynecologists' Committee on Practice Bulletins—Obstetrics.. ACOG Practice Bulletin No. 196: Thromboembolism in Pregnancy. Obstet Gynecol. 2018; 132:e1-e17. https://pubmed.ncbi.nlm.nih.gov/29939938
1143. Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP 3rd, Gentile F, Jneid H, Krieger EV, Mack M, McLeod C, O'Gara PT, Rigolin VH, Sundt TM 3rd, Thompson A, Toly C. 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021 Feb 2;143(5):e72-e227. doi: 10.1161/CIR.0000000000000923. Epub 2020 Dec 17. Erratum in: Circulation. 2021 Feb 2;143(5):e229. PMID: 33332150.
1162. Cuker A, Burnett A, Triller D et al. Reversal of direct oral anticoagulants: Guidance from the Anticoagulation Forum. Am J Hematol. 2019; 94:697-709. (IDIS ) (PubMed 30916798) (DOI 10.1002/ajh.25475) (URL )
1163. Zuily S, Cohen H, Isenberg D et al. Use of direct oral anticoagulants in patients with thrombotic antiphospholipid syndrome: Guidance from the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis. J Thromb Haemost. 2020; 18:2126-2137. (IDIS ) (PubMed 32881337) (DOI 10.1111/jth.14935)
1164. Boehringer Ingelheim. Pradaxa (dabigatran etexilate mesylate) oral pellets prescribing information. Ridgefield, CT. 2021 Jun.
1166. Halton J, Brandão LR, Luciani M, Bomgaars L, Chalmers E, Mitchell LG, Nurmeev I, Sharathkumar A, Svirin P, Gorbatikov K, Tartakovsky I, Simetzberger M, Huang F, Sun Z, Kreuzer J, Gropper S, Reilly P, Brueckmann M, Albisetti M; DIVERSITY Trial Investigators. Dabigatran etexilate for the treatment of acute venous thromboembolism in children (DIVERSITY): a randomised, controlled, open-label, phase 2b/3, non-inferiority trial. Lancet Haematol. 2021 Jan;8(1):e22-e33. Epub 2020 Dec 5. https://pubmed.ncbi.nlm.nih.gov/33290737
1167. Open Label Study Comparing Efficacy and Safety of Dabigatran Etexilate to Standard of Care in Paediatric Patients With Venous Thromboembolism (VTE). From Clinicaltrials.gov registry. Accessed 28 Jan 2022.
1168. Anticoagulation Forum. Direct oral anticoagulant (DOAC) drug-drug interaction guidance. Updated June 2020. Accessed October 31, 2022. https://acforum-excellence.org/Resource-Center/resource_files/-2021-04-28-132351.pdf
1169. Institute for Safe Medication Practices (ISMP). ISMP list of high-alert medications in acute care settings. ISMP; 2018.
Related/similar drugs
Frequently asked questions
More about dabigatran
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (102)
- Drug images
- Latest FDA alerts (5)
- Side effects
- Dosage information
- During pregnancy
- Drug class: thrombin inhibitors
- Breastfeeding
- En español