Cabergoline (Monograph)
Drug class: Ergot-derivative Dopamine Receptor Agonists
VA class: AU900
Chemical name: 1-[(6-allylergolin-8β-yl)-carbonyl]-1-[3-(dimethylamino)propyl]-3-ethylurea
Molecular formula: C26H37N5O2
CAS number: 81409-90-7
Introduction
An ergot-derivative dopamine receptor agonist and prolactin inhibitor.1 2 3 8 10 11 12 15
Uses for Cabergoline
Hyperprolactinemic Disorders
Treatment of hyperprolactinemic disorders, including those caused by pituitary adenomas (i.e., prolactinomas) and those with unknown cause (idiopathic hyperprolactinemia).1 2 3 13 14
Treatment of prolactinomas may or may not be necessary depending on size of tumor.131 Therapy is routinely indicated for macroadenomas (tumor ≥10 mm), but not for microadenomas unless there is a compelling indication (e.g., infertility in a patient desiring pregnancy).131 132
Dopamine agonists are considered first-line therapy of hyperprolactinemia and prolactinomas.131 132 These drugs can decrease prolactin concentrations, reduce tumor mass, and restore gonadal function.1 2 3 13 14 128 131 132
Cabergoline is usually preferred over bromocriptine because of its longer duration of action, greater efficacy, and more favorable adverse effect profile.128 131 132 133
Parkinsonian Syndrome
Has been used for the symptomatic management of parkinsonian syndrome† [off-label].4 5 6 7 8 9 10 11 However, ergot-derived dopamine agonists such as cabergoline no longer recommended in the treatment of parkinson disease because of risks of serious adverse effects (e.g., cardiac valvulopathy); if dopamine agonist therapy is required, a nonergot-derived dopamine agonist (e.g., pramipexole, ropinirole, rotigotine) should be used.123 124 125 126 127 128 157
Acromegaly
Has been used for the treatment of acromegaly† [off-label].128 129 130 134 135 However, transsphenoidal surgery is first-line treatment for this condition; in patients who cannot undergo surgery or who have persistent disease after surgery, somatostatin receptor agonists (e.g., octreotide, lanreotide) are the drugs of choice for primary medical treatment.129 130 134
Dopamine agonists generally considered only for adjuvant medical therapy in patients with mild disease following surgery.128 129 130 134
Cabergoline is most likely to benefit patients with modest elevations of growth hormone and insulin-like growth factor I (IGF-I levels).129 134
Cabergoline Dosage and Administration
Administration
Oral Administration
Administer orally without regard to meals.1
Dosage
Adults
Hyperprolactinemic Disorders
Oral
Initiate with low dosage and increase slowly (at ≥4-week intervals) until therapeutic response is achieved.1
Initially, 0.25 mg twice weekly; may increase in increments of 0.25 mg twice weekly up to 1 mg twice weekly.1 Base dosage adjustments on serum prolactin concentrations; use lowest effective dosage.1
Periodically evaluate patient to determine continued need for therapy.1 Some patients (e.g., those with normal prolactin concentrations for 6 months) may be able to discontinue the drug with periodic monitoring of prolactin concentrations to determine whether or when cabergoline therapy should be reinstituted;1 14 15 discontinuance in those with macroadenomas should be undertaken with extreme caution.14 15 The manufacturer states that efficacy >24 months not established.1
Special Populations
Hepatic Impairment
No specific dosage recommendations at this time; use with caution in patients with severe hepatic impairment.1 (See Hepatic Impairment under Cautions and also see Absorption: Special Populations, under Pharmacokinetics.)
Renal Impairment
No specific dosage recommendations at this time.1 (See Elimination: Special Populations, under Pharmacokinetics.)
Geriatric Patients
Select dosage carefully; start at low dosage.1 (See Geriatric Use under Cautions.)
Cautions for Cabergoline
Contraindications
-
Known hypersensitivity to cabergoline or other ergot derivatives.1
-
Uncontrolled hypertension.1
-
History of cardiac valvular disorders (e.g., valve leaflet thickening, valve restriction, mixed valve restriction-stenosis).1
-
History of pulmonary, pericardial, or retroperitoneal fibrotic disorders.1
Warnings/Precautions
Warnings
Hypertension during Pregnancy
Do not use in patients with pregnancy-induced hypertension (e.g., preeclampsia, eclampsia, postpartum hypertension) unless potential benefits outweigh possible risks.1
Fibrotic Effects
Cases of cardiac valvulopathy reported in postmarketing setting.1 Generally occurred in patients receiving high dosages of the drug for treatment of parkinson disease, but also reported with lower dosages for hyperprolactinemic disorders.1 134 135
Pleural effusion, pulmonary fibrosis, and retroperitoneal fibrosis also reported.1 16 Signs and symptoms have improved after discontinuance.1
Perform cardiac evaluation (including echocardiogram) and other diagnostic procedures prior to initiating therapy; do not initiate drug in patients with valvular disease or any other evidence of past or present fibrotic disorders.1 (See Contraindications under Cautions.) Perform routine clinical monitoring and echocardiography periodically during therapy; discontinue drug if any signs of new valvular regurgitation, valvular restriction, or valve leaflet thickening occur.1
Consider clinical and diagnostic monitoring for possible extracardiac fibrotic reactions at baseline and as needed during therapy.1 Following diagnosis of pleural effusion or pulmonary fibrosis, drug discontinuance reportedly has resulted in improvement of signs and symptoms.1
Use lowest effective dosage for treatment of hyperprolactinemic disorders and periodically evaluate patient to determine need for continued treatment.1
General Precautions
Symptomatic Hypotension
Orthostatic hypotension reported, especially when initial doses >1 mg are used.1 Exercise care in patients currently receiving drugs known to lower BP.1
Postpartum Breast Engorgement
Not indicated for the inhibition or suppression of lactation.1 Hypertension, stroke, and seizures reported rarely when another dopamine receptor agonist (i.e., bromocriptine) was used for this indication.1
Impulse Control and Compulsive Behaviors
Intense urges and compulsive behaviors (e.g., urge to gamble, increased sexual urges, binge eating, uncontrolled spending, other intense urges) and inability to control these urges reported with dopaminergic drugs.1 In some cases, urges stopped when dosage was reduced or drug was discontinued.1
Consider reducing dosage or discontinuing therapy if a patient develops such urges while receiving the drug.1 (See Advice to Patients.)
Specific Populations
Pregnancy
No adequate and well-controlled studies in pregnant women.1 Animal reproduction studies revealed some evidence of maternal toxicity and postimplantation embryofetal loss, but developmental malformations not consistently observed.1 (See Hypertension during Pregnancy under Cautions.)
Lactation
Not known whether cabergoline is distributed into milk; drug is expected to interfere with lactation.1 Discontinue nursing or the drug.1
Pediatric Use
Safety and efficacy not established.1
Geriatric Use
Insufficient experience from clinical studies to determine whether patients ≥65 years of age respond differently than younger adults.1 Other clinical experience has not identified age-related differences in responses.1
Effect of age on pharmacokinetics not studied.1
Consider the greater frequency of decreased hepatic, renal, or cardiac function and of concomitant disease or drug therapy in geriatric patients.1 2 3
Hepatic Impairment
Extensively metabolized in liver; use with caution and monitor carefully.1 (See Absorption: Special Populations, under Pharmacokinetics.)
Renal Impairment
Pharmacokinetics not altered in patients with moderate to severe renal impairment.1
Common Adverse Effects
Patients with hyperprolactinemia: Nausea, constipation, abdominal pain, headache, dizziness, asthenia, fatigue, somnolence.1
Drug Interactions
Dopamine Antagonists
Concomitant use with dopamine antagonists (e.g., phenothiazines, butyrophenones, thioxanthenes, metoclopramide) not recommended because of possible reduced efficacy of cabergoline.1
Cabergoline Pharmacokinetics
Absorption
Bioavailability
Peak plasma concentrations usually attained within 1–2 hours.1 17
Absolute bioavailability unknown.1 17
Onset
Following oral administration of a single 0.6-mg dose of cabergoline, time to maximum prolactin-lowering effect was 48 hours.1
Duration
Prolactin-lowering effect persists for 14 days.1
Food
Food does not alter the pharmacokinetics of cabergoline.1
Special Populations
Peak plasma concentrations and AUC not altered in patients with mild to moderate hepatic impairment (Child-Pugh score ≤10).1 Peak plasma concentrations and AUC substantially increased in patients with severe hepatic impairment (Child-Pugh score >10).1
Distribution
Extent
Extensively distributed throughout the body, including the CNS.1 8
Plasma Protein Binding
Elimination
Metabolism
Metabolized in the liver (minimal CYP involvement), mainly by hydrolysis of the acylurea bond;1 17 undergoes substantial first-pass metabolism.1
Elimination Route
Excreted in feces (72%) and in urine (18% as metabolites and unchanged drug).17
Half-life
Special Populations
Pharmacokinetic values not altered in patients with moderate to severe renal impairment.1 17
Effect of age on pharmacokinetics not studied.1
Stability
Storage
Oral
Tablets
20–25°C.1
Actions
-
A long-acting dopamine receptor agonist; has high binding affinity for dopamine D2 receptors and lesser affinity for D1, α1- and α2-adrenergic, and serotonin (5-HT1 and 5-HT2) receptors.1 8
-
Reduces serum prolactin concentrations by inhibiting release of prolactin from the anterior pituitary gland.1 This effect on hypothalamic/pituitary function attributed to the drug’s agonist activity at D2 receptors.1
Advice to Patients
-
Importance of patients informing their clinician if cough, dyspnea, difficulty breathing when lying down, or swelling of extremities develops.1
-
Importance of asking patients whether they have developed any new or increased urges or compulsive behaviors (e.g., gambling urges, sexual urges, uncontrolled spending, binge eating) while receiving cabergoline and advising them of the importance of reporting such urges.1
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.1
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses (e.g., respiratory or cardiac disorders associated with fibrosis).1
-
Importance of informing patients of other important precautionary information.1 (See Cautions.)
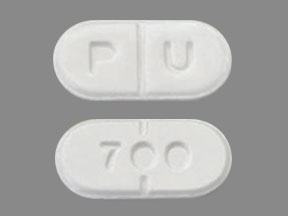
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
0.5 mg* |
Cabergoline Tablets |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions May 4, 2022. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
1. Greenstone. Cabergoline tablets prescribing information. Peapack, NJ; 2019 Nov.
2. Webster J, Piscitelli G, Polli A et al. Dose-dependent suppression of serum prolactin by carbergoline in hyperprolactinemia: a placebo controlled, double blind, multicentre study. Clin Endocrinol. 1992; 37:534-41.
3. Webster J, Piscitelli G, Polli A et al. The efficacy and tolerability of long-term cabergoline therapy in hyperprolactinemic disorders; an open, uncontrolled, multicentre study. Clin Endocrinol. 1993; 39:323-9.
4. Clarke CE, Deane KHO. Cabergoline versus bromocriptine for levodopa-induced complications in Parkinson’s disease. Cochrane Database of Systematic Reviews 2001, Issue 1. Art. No.: CD001519. DOI: 10.1002/14651858.CD001519.
5. Clarke CE, Deane KHO. Cabergoline for levodopa-induced complications in Parkinson’s disease. Cochrane Database of Systematic Reviews 2001, Issue 1. Art. No.: CD001518. DOI: 10.1002/14651858.CD001518.
6. Pahwa R, Factor SA, Lyons KE et al. Practice parameter: treatment of Parkinson disease with motor fluctuations and dyskinesia (an evidence-based review): Report of the quality standards subcommittee of the American Academy of Neurology. Neurology. 2006; 66:983-95. https://pubmed.ncbi.nlm.nih.gov/16606909
7. Olanow CW, Watts, RL, Koller WC. An algorithm (decision tree) for the management of Parkinson’s disease: treatment guidelines (2001). Neurology. 2001; 56 (Suppl):S1-88. https://pubmed.ncbi.nlm.nih.gov/11402154
8. Curran MP, Perry CM. Cabergoline: a review of its use in the treatment of Parkinson’s disease. Drugs. 2004; 64:2125-41. https://pubmed.ncbi.nlm.nih.gov/15341508
9. Miyasaki JM, Martin W, Suchowersky O et al. Practice parameter: initiation of treatment for Parkinson’s disease: an evidence-based review: Report of the quality standards subcommittee of the American Academy of Neurology. Neurology. 2002; 58:11-7. https://pubmed.ncbi.nlm.nih.gov/11781398
10. Marsden CD. Clinical experience with cabergoline in patients with advanced Parkinson’s disease treated with levodopa. Drugs. 1998; 55 (Suppl 1):17-22. https://pubmed.ncbi.nlm.nih.gov/9483166
11. Rinne UK, Bracco F, Chouza C et al. Early treatment of Parkinson’s disease with cabergoline delays the onset of motor complications: results of a double-blind levodopa controlled trial: The PKDS009 Study Group. Drugs. 1998; 55 (Suppl 1):23-30. https://pubmed.ncbi.nlm.nih.gov/9483167
12. Webster J, Piscitelli G, Polli A et al. A comparison of cabergoline and bromocriptine in the treatment of hyperprolactinemic amenorrhea: carbergoline comparative study group. N Engl J Med. 1994; 331:904-9. https://pubmed.ncbi.nlm.nih.gov/7915824
13. Webster J. Dopamine agonist therapy in hyperprolactinemia. J Reprod Med. 1999; 44:1105-10. https://pubmed.ncbi.nlm.nih.gov/10649819
14. Schlechte JA. Prolactinoma. N Engl J Med. 2003; 349:2035-41. https://pubmed.ncbi.nlm.nih.gov/14627789
15. Colao A, Di Sarno A, Cappabianca P et al. Withdrawl of long-term cabergoline therapy for tumoral and nontumoral hyperprolactinemia. N Engl J Med. 2003; 349:2023-33. https://pubmed.ncbi.nlm.nih.gov/14627787
16. Ling LH, Ahlskog JE, Munger TM et al. Constrictive pericarditis and pleuropulmonary disease linked to ergot dopamine agonist therapy (cabergoline) for Parkinson’s disease. Mayo Clin Proc. 1999; 74:371-5. https://pubmed.ncbi.nlm.nih.gov/10221467
17. Del Dotto P, Bonuccelli U. Clinical pharmacokinetics of cabergoline. Clin Pharmacokinet. 2003; 42:633-45. https://pubmed.ncbi.nlm.nih.gov/12844325
123. Connolly BS, Lang AE. Pharmacological treatment of Parkinson disease: a review. JAMA. 2014 Apr 23-30; 311:1670-83. https://pubmed.ncbi.nlm.nih.gov/24756517
124. Armstrong MJ, Okun MS. Diagnosis and Treatment of Parkinson Disease: A Review. JAMA. 2020; 323:548-560. https://pubmed.ncbi.nlm.nih.gov/32044947
125. Van Camp G, Flamez A, Cosyns B et al. Treatment of Parkinson's disease with pergolide and relation to restrictive valvular heart disease. Lancet. 2004; 363:1179-83. https://pubmed.ncbi.nlm.nih.gov/15081648
126. Zanettini R, Antonini A, Gatto G et al. Valvular heart disease and the use of dopamine agonists for Parkinson's disease. N Engl J Med. 2007; 356:39-46. https://pubmed.ncbi.nlm.nih.gov/17202454
127. Bonuccelli U, Del Dotto P, Rascol O. Role of dopamine receptor agonists in the treatment of early Parkinson's disease. Parkinsonism Relat Disord. 2009; 15 Suppl 4:S44-53. https://pubmed.ncbi.nlm.nih.gov/20123557
128. Michael Besser G, Pfeiffer RF, Thorner MO. ANNIVERSARY REVIEW: 50 years since the discovery of bromocriptine. Eur J Endocrinol. 2018; 179:R69-R75. https://pubmed.ncbi.nlm.nih.gov/29752299
129. Giustina A, Chanson P, Kleinberg D et al. Expert consensus document: A consensus on the medical treatment of acromegaly. Nat Rev Endocrinol. 2014; 10:243-8. https://pubmed.ncbi.nlm.nih.gov/24566817
130. Sandret L, Maison P, Chanson P. Place of cabergoline in acromegaly: a meta-analysis. J Clin Endocrinol Metab. 2011; 96:1327-35. https://pubmed.ncbi.nlm.nih.gov/21325455
131. Klibanski A. Clinical practice. Prolactinomas. N Engl J Med. 2010; 362:1219-26. https://pubmed.ncbi.nlm.nih.gov/20357284
132. Melmed S, Casanueva FF, Hoffman AR et al. Diagnosis and treatment of hyperprolactinemia: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011; 96:273-88. https://pubmed.ncbi.nlm.nih.gov/21296991
133. Webster J, Piscitelli G, Polli A et al. A comparison of cabergoline and bromocriptine in the treatment of hyperprolactinemic amenorrhea. Cabergoline Comparative Study Group. N Engl J Med. 1994; 331:904-9. https://pubmed.ncbi.nlm.nih.gov/7915824
134. Katznelson L, Laws ER, Melmed S et al. Acromegaly: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2014; 99:3933-51. https://pubmed.ncbi.nlm.nih.gov/25356808
135. Maione L, Garcia C, Bouchachi A et al. No evidence of a detrimental effect of cabergoline therapy on cardiac valves in patients with acromegaly. J Clin Endocrinol Metab. 2012; 97:E1714-9. https://pubmed.ncbi.nlm.nih.gov/22723314
157. . Drugs for Parkinson's disease. Med Lett Drugs Ther. 2017; 59:187-194. https://pubmed.ncbi.nlm.nih.gov/29136401
Related/similar drugs
More about cabergoline
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (119)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: prolactin inhibitors
- Breastfeeding
- En español