busPIRone (Monograph)
Brand names: BuSpar, BuSpar Dividose
Drug class: Non-benzodiazepine Anxiolytics
Introduction
Anxiolytic agent; structurally and pharmacologically different than benzodiazepines, barbiturates, and other available anxiolytic agents.
Uses for busPIRone
Anxiety Disorders
Management of anxiety disorders (anxiety and phobic neuroses) and short-term relief of symptoms of anxiety.
Efficacy generally comparable to that of benzodiazepines (e.g., alprazolam, clorazepate, diazepam, lorazepam) in the management of generalized anxiety disorder (GAD).
Preferred by some clinicians for the management of anxiety disorders in patients with a history of aggression or in whom disinhibition has occurred during benzodiazepine therapy.
busPIRone Dosage and Administration
General
-
Slower onset of action than some anxiolytics (e.g., diazepam). Optimum therapeutic effect usually requires at least 3–4 weeks and occasionally up to 4–6 weeks of therapy.
-
Periodically reassess need for continued therapy.
Administration
Oral Administration
Administer orally in a consistent manner, either always with or always without food. (See Food under Pharmacokinetics.)
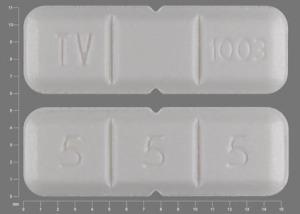
The 15- and 30-mg tablets (Dividose tablets) are scored to be broken in 2 halves (each providing a dose of 7.5 and 15 mg, respectively) or in 3 thirds (each providing a dose of 5 and 10 mg, respectively).
Dosage
Available as buspirone hydrochloride; dosage is expressed in terms of the salt.
Adults
Anxiety Disorders
Oral
Initially, 10–15 mg daily in 2 or 3 divided doses. Increase dosage in increments of 5 mg daily every 2–4 days according to individual response and tolerance. Maintenance, 15–30 mg daily in 2 or 3 divided doses.
Reduced dosage recommended in patients receiving concomitant therapy with potent CYP3A4 inhibitor. (See Drugs Affecting Hepatic Microsomal Enzymes under Interactions.)
Prescribing Limits
Adults
Maximum 60 mg daily.
Special Populations
Hepatic Impairment
Prolonged elimination. Consider dosage reduction. Manufacturer states that use in patients with severe hepatic impairment is not recommended.
Renal Impairment
Some clinicians recommend that dosage be reduced by 25–50% in anuric patients. However, other clinicians state that dosage recommendations cannot be made for patients with renal impairment due to variability in plasma buspirone concentrations. (See Absorption under Pharmacokinetics.) Manufacturer states that use in patients with severe renal impairment is not recommended.
Cautions for busPIRone
Contraindications
-
Known hypersensitivity to buspirone hydrochloride.
Warnings/Precautions
Warnings
MAO Inhibitors
Avoid concomitant use. (See Specific Drugs under Interactions.)
Psychiatric Indications
No established antipsychotic efficacy at usual dosages; should not be used in place of appropriate antipsychotic therapy.
General Precautions
CNS Effects
Generally does not produce substantial impairment of cognitive or psychomotor function at usual dosages; however, CNS effects show interindividual variation and may not be predictable.
Prudent to avoid concomitant use with alcohol. (See Specific Drugs under Interactions.)
Benzodiazepine or Sedative/Hypnotic Withdrawal
No cross-tolerance with benzodiazepines or other sedative/hypnotic drugs; will not prevent symptoms of withdrawal following cessation of such therapy. Withdraw therapy with such drugs gradually in patients being switched to buspirone, particularly following prolonged or relatively high-dose therapy.
Dopaminergic Effects
Potential for causing changes in dopamine-mediated neurologic function (e.g., dystonia, parkinsonian-like manifestations, akathisia, tardive dyskinesia) not fully elucidated.
Specific Populations
Pregnancy
Category B.
Lactation
Buspirone and its metabolites are distributed into milk in rats. Avoid whenever clinically possible.
Pediatric Use
Safety and efficacy not established in children <18 years of age. Has been used in pediatric patients 6–17 years of age with GAD without unusual adverse effects; however, dosage of 7.5–30 mg twice daily for 6 weeks was no more effective than placebo.
Geriatric Use
No substantial differences in safety, efficacy, or phamacokinetic profile relative to younger adults; however, increased sensitivity cannot be ruled out.
Hepatic Impairment
Prolonged elimination. Use with caution.
Manufacturer states that use in patients with severe hepatic impairment is not recommended.
Renal Impairment
Decreased clearance. Use with caution. Need for dosage adjustment not fully elucidated. (See Renal Impairment under Dosage and Administration.)
Manufacturer states that use in patients with severe renal impairment is not recommended.
Common Adverse Effects
Dizziness, nausea, headache, nervousness, drowsiness, light-headedness, excitement.
Drug Interactions
Metabolized by CYP3A4.
Drugs Affecting Hepatic Microsomal Enzymes
Possible pharmacokinetic interaction (increased plasma buspirone concentrations) with CYP3A4 inhibitors. Low buspirone dosage (i.e., 2.5 mg once or twice daily) recommended in patients receiving potent CYP3A4 inhibitor; base subsequent adjustments of buspirone and CYP3A4 inhibitor dosage on clinical assessment.
Possible pharmacokinetic interaction (decreased plasma buspirone concentrations) with CYP3A4 inducers. May require dosage adjustment to maintain anxiolytic effect.
Protein-bound Drugs
Possible displacement from binding sites of buspirone or other protein-bound drugs.
One report of increased prothrombin time when buspirone was added to a regimen of warfarin, phenytoin, phenobarbital, digoxin, and levothyroxine (Synthroid); clinical importance unknown.
Specific Drugs and Foods
|
Drug or Food |
Interaction |
Comments |
|---|---|---|
|
Alcohol |
Does not appear to alter blood alcohol concentrations or substantially potentiate alcohol-induced impairment of psychomotor and cognitive performance |
Prudent to avoid concomitant use |
|
Amitriptyline |
No interaction reported |
|
|
Cimetidine |
Possible decrease in buspirone clearance |
Clinical importance not established |
|
CNS depressants (e.g., analgesics, antihistamines, sedative/hypnotics including benzodiazepines) |
Possible CNS depression, although few interactions reported to date |
Use with caution |
|
Diltiazem |
Increased plasma buspirone concentrations |
Buspirone dosage adjustment may be necessary |
|
Erythromycin |
Increased plasma buspirone concentrations and increased incidence of adverse effects attributable to buspirone |
Decrease buspirone dosage (e.g., 2.5 mg twice daily); base subsequent adjustments of buspirone and erythromycin dosage on clinical assessment |
|
Grapefruit juice |
Increased plasma buspirone concentrations |
Avoid drinking large amounts of grapefruit juice |
|
Haloperidol |
Increased serum haloperidol concentrations |
Clinical importance not established |
|
Itraconazole |
Increased plasma buspirone concentrations and increased incidence of adverse effects attributable to buspirone |
Decrease buspirone dosage (e.g., 2.5 mg daily); base subsequent adjustments of buspirone and itraconazole dosage on clinical assessment |
|
MAO inhibitors (e.g., tranylcypromine) |
Increased blood pressure; possible contribution to a fatal case of serotonin syndrome when used concomitantly with fluoxetine and tranylcypromine |
Do not use concomitantly; allow 10 days between discontinuance of MAO inhibitor and administration of buspirone |
|
Nefazodone |
Marked increase in plasma buspirone concentration; slight increase in concentrations of nefazodone and its metabolite |
Use with caution; decrease buspirone dosage (e.g., 2.5 mg daily); base subsequent adjustments of buspirone and nefazodone dosage on clinical assessment |
|
Rifampin |
Decreased plasma buspirone concentrations |
Adjust buspirone dosage as necessary to maintain anxiolytic effect |
|
Trazodone |
Possible elevation of serum ALT |
|
|
Verapamil |
Increased plasma buspirone concentrations |
Buspirone dosage adjustment may be necessary |
busPIRone Pharmacokinetics
Absorption
Bioavailability
Rapidly and almost completely absorbed following oral administration. Undergoes extensive first-pass metabolism in the liver; only about 4% of a dose reaches systemic circulation unchanged.
Peak plasma concentrations occur within 40–90 minutes following oral administration.
Onset
Anxiolytic activity may be apparent within the first 2 weeks, but optimum therapeutic effect usually requires at least 3–4 weeks and occasionally up to 4–6 weeks.
Food
Food may delay absorption, thereby decreasing the extent of presystemic clearance and increasing the amount of unchanged buspirone reaching systemic circulation.
Distribution
Extent
Extensively distributed into body tissues in animals.
Buspirone and metabolites are distributed into milk in animals; extent of distribution into human milk is unknown.
Plasma Protein Binding
Approximately 86–95% (mainly albumin; α1-acid glycoprotein to a lesser extent).
Elimination
Metabolism
Extensively metabolized in the liver, mainly via oxidation by CYP3A4.
In animals, the major active metabolite (1-pyrimidinylpiperazine) has about 20–25% of the anxiolytic activity of buspirone but is present in the brain in concentrations up to 15-to 30-fold greater than those of unchanged drug. Contribution to the drug’s effects in humans is not fully elucidated.
Elimination Route
Excreted principally in urine and to a lesser extent in feces; excreted mainly as metabolites.
Half-life
2–4 hours.
Special Populations
Elimination half-life may be prolonged in patients with renal impairment, particularly in those with anuria, and in patients with liver impairment, including those with cirrhosis.
Stability
Storage
Oral
Tablets
Tight, light-resistant containers at ≤30°C.
Actions
-
Anxioselective drug; unlike benzodiazepines, has no anticonvulsant or muscle relaxant activity, does not substantially impair psychomotor function, and has little sedative effect.
-
Mechanism of action is unknown; appears to be complex and distinct from that of benzodiazepines; probably involves several central neurotransmitter systems.
-
Effects may be mediated by a variety of CNS sites including serotonergic, dopaminergic, cholinergic, and noradrenergic (α-adrenergic) systems. No appreciable affinity for the benzodiazepine receptor complex.
Advice to Patients
-
Potential for drug to impair mental alertness or physical coordination; avoid driving or operating machinery until effects on individual are known.
-
Importance of taking buspirone in a consistent manner, either always with or always without food.
-
Importance of not drinking large quantities of grapefruit juice.
-
Symptomatic relief may occur within 2 weeks, but optimum effect usually requires at least 3–4 weeks and occasionally 4–6 weeks of therapy.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, and alcohol consumption. Prudent to avoid alcohol-containing beverages or products.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Contraindications and also Warnings/Precautions under Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
5 mg* |
BuSpar (scored) |
Bristol-Myers Squibb |
|
Buspirone Hydrochloride (scored) |
Aegis |
|||
|
7.5 mg* |
Buspirone Hydrochloride (with povidone; scored) |
Par |
||
|
10 mg* |
BuSpar (multi-scored) |
Bristol-Myers Squibb |
||
|
Buspirone Hydrochloride (scored) |
Aegis |
|||
|
15 mg* |
BuSpar Dividose (scored) |
Bristol-Myers Squibb |
||
|
Buspirone Hydrochloride (multi-scored) |
Aegis |
|||
|
30 mg* |
BuSpar Dividose (multi-scored) |
Bristol-Myers Squibb |
||
|
Buspirone Hydrochloride (multi-scored) |
Mylan |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
Frequently asked questions
More about buspirone
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (1,375)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: miscellaneous anxiolytics, sedatives and hypnotics
- Breastfeeding
- En español