aMILoride (Monograph)
Drug class: Potassium-sparing Diuretics
- Diuretics, Potassium-sparing
aMILoride (Systemic) is also contained as an ingredient in the following combinations:
aMILoride Hydrochloride and Hydrochlorothiazide
Warning
-
Hyperkalemia (i.e., serum potassium concentrations >5.5 mEq/L) may occur with all potassium-sparing agents, including amiloride.a b c
-
Hyperkalemia occurs in about 10% of patients receiving amiloride without a kaliuretic diuretic and more frequently in patients with renal impairment or diabetes (even without evidence of renal impairment) and in geriatric patients.b In patients without the mentioned complications, incidence of hyperkalemia is reduced to 1–2% by concomitant use of amiloride with a thiazide diuretic.b
-
Uncorrected hyperkalemia may be fatal; monitor serum potassium concentrations carefully, especially during initial therapy or dosage adjustments, and in patients with concurrent illness that may affect renal function.a b c
Introduction
Potassium-sparing diuretic; pyrazinecarbonyl guanidine derivative.a b
Uses for aMILoride
Amiloride should rarely be used alone, because such use may result in increased risk of hyperkalemia.a b Use alone only when persistent hypokalemia has been documented.b
Hypokalemia Induced by Kaliuretic Diuretics
Treatment or prevention of hypokalemia induced by thiazide or other kaliuretic diuretics in patients with heart failure or hypertension.a b c
May be particularly useful for preventing diuretic-induced hypokalemia in patients in whom the clinical consequences of hypokalemia represent an important risk, such as patients receiving cardiac glycosides or those with cardiac arrhythmias.a b c
Also useful in patients with hypokalemia who do not respond to potassium supplements or those who cannot tolerate potassium supplements.a
Potassium-sparing effect of amiloride generally persists during prolonged therapy with the drug, but may diminish with time in some patients.a
Potassium-sparing effect of amiloride is additive with that of spironolactone.a May be effective in some patients unresponsive to spironolactone; unlike spironolactone, diuretic effect of amiloride is independent of aldosterone concentrations.a
Edema
Management of edema associated with heart failure, cirrhosis of the liver, or secondary hyperaldosteronism.a
Generally, use in combination with other more effective, rapidly acting diuretics, such as thiazides, chlorthalidone, or loop diuretics (e.g., furosemide), to decrease potassium excretion caused by kaliuretic diuretics.a b
Used in fixed combination with hydrochlorothiazide for treatment of edema in patients who require a thiazide diuretic and in whom the development of hypokalemia cannot be risked.c
Heart Failure
Management of edema associated with heart failure, generally used in conjunction with other more effective, rapidly acting diuretics (e.g., thiazides, chlorthalidone, loop diuretics).a
Most experts state that loop diuretics (e.g., bumetanide, ethacrynic acid, furosemide, torsemide) are the diuretics of choice for most patients with heart failure.524
Most experts state that all patients with symptomatic heart failure who have evidence for, or a history of, fluid retention generally should receive diuretic therapy in conjunction with moderate sodium restriction, an agent to inhibit the renin-angiotensin-aldosterone (RAA) system (e.g., ACE inhibitor, angiotensin II receptor antagonist, angiotensin receptor-neprilysin inhibitor [ARNI]), a β-adrenergic blocking agent (β-blocker), and in selected patients, an aldosterone antagonist.524 700 713
Hypertension
Management of hypertension alone or in combination with other classes of antihypertensive agents;502 504 1200 however, other agents (i.e., ACE inhibitors, angiotensin II receptor antagonists, calcium-channel blockers, thiazide diuretics) are preferred for initial management according to current evidence-based practice guidelines for the management of hypertension in adults.501 502 503 504 1200
Amiloride alone has mild hypotensive activity.a b
Used concomitantly with a thiazide diuretic mainly to prevent or treat diuretic-induced hypokalemia.a b (See Hypokalemia Induced by Kaliuretic Diuretics under Uses.) The manufacturers state that amiloride produces little additive hypotensive activity when used concurrently with a thiazide diuretic.a b
Some experts state that amiloride may be useful as a component of combination therapy in the management of resistant hypertension.502
Used in fixed combination with hydrochlorothiazide for treatment of hypertension in patients who require a thiazide diuretic and in whom the development of hypokalemia cannot be risked and in patients who develop hypokalemia during hydrochlorothiazide monotherapy.c
Use the amiloride/hydrochlorothiazide fixed combination alone or as an adjunct to other antihypertensive agents (e.g., methyldopa, β-blocker).c
Individualize choice of therapy; consider patient characteristics (e.g., age, ethnicity/race, comorbidities, cardiovascular risk) as well as drug-related factors (e.g., ease of administration, availability, adverse effects, cost).501 502 503 504 515 1200 1201
A 2017 ACC/AHA multidisciplinary hypertension guideline classifies BP in adults into 4 categories: normal, elevated, stage 1 hypertension, and stage 2 hypertension.1200 (See Table 1.)
Source: Whelton PK, Carey RM, Aronow WS et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13-115.
Individuals with SBP and DBP in 2 different categories (e.g., elevated SBP and normal DBP) should be designated as being in the higher BP category (i.e., elevated BP).
|
Category |
SBP (mm Hg) |
DBP (mm Hg) |
|
|---|---|---|---|
|
Normal |
<120 |
and |
<80 |
|
Elevated |
120–129 |
and |
<80 |
|
Hypertension, Stage 1 |
130–139 |
or |
80–89 |
|
Hypertension, Stage 2 |
≥140 |
or |
≥90 |
The goal of hypertension management and prevention is to achieve and maintain optimal control of BP.1200 However, the BP thresholds used to define hypertension, the optimum BP threshold at which to initiate antihypertensive drug therapy, and the ideal target BP values remain controversial.501 503 504 505 506 507 508 515 523 526 530 1200 1201 1207 1209 1222 1223 1229
The 2017 ACC/AHA hypertension guideline generally recommends a target BP goal (i.e., BP to achieve with drug therapy and/or nonpharmacologic intervention) of <130/80 mm Hg in all adults regardless of comorbidities or level of atherosclerotic cardiovascular disease (ASCVD) risk.1200 In addition, an SBP goal of <130 mm Hg generally is recommended for noninstitutionalized ambulatory patients ≥65 years of age with an average SBP of ≥130 mm Hg.1200 These BP goals are based upon clinical studies demonstrating continuing reduction of cardiovascular risk at progressively lower levels of SBP.1200 1202 1210
Other hypertension guidelines generally have based target BP goals on age and comorbidities.501 504 536 Guidelines such as those issued by the JNC 8 expert panel generally have targeted a BP goal of <140/90 mm Hg regardless of cardiovascular risk, and have used higher BP thresholds and target BPs in elderly patients501 504 536 compared with those recommended by the 2017 ACC/AHA hypertension guideline.1200
Some clinicians continue to support previous target BPs recommended by JNC 8 due to concerns about the lack of generalizability of data from some clinical trials (e.g., SPRINT study) used to support the 2017 ACC/AHA hypertension guideline and potential harms (e.g., adverse drug effects, costs of therapy) versus benefits of BP lowering in patients at lower risk of cardiovascular disease.1222 1223 1224 1229
Consider potential benefits of hypertension management and drug cost, adverse effects, and risks associated with the use of multiple antihypertensive drugs when deciding a patient's BP treatment goal.1200 1220 1229
For decisions regarding when to initiate drug therapy (BP threshold), the 2017 ACC/AHA hypertension guideline incorporates underlying cardiovascular risk factors.1200 1207 ASCVD risk assessment is recommended by ACC/AHA for all adults with hypertension.1200
ACC/AHA currently recommend initiation of antihypertensive drug therapy in addition to lifestyle/behavioral modifications at an SBP ≥140 mm Hg or DBP ≥90 mm Hg in adults who have no history of cardiovascular disease (i.e., primary prevention) and a low ASCVD risk (10-year risk <10%).1200
For secondary prevention in adults with known cardiovascular disease or for primary prevention in those at higher risk for ASCVD (10-year risk ≥10%), ACC/AHA recommend initiation of antihypertensive drug therapy at an average SBP ≥130 mm Hg or an average DBP ≥80 mm Hg.1200
Adults with hypertension and diabetes mellitus, CKD, or age ≥65 years are assumed to be at high risk for cardiovascular disease; ACC/AHA state that such patients should have antihypertensive drug therapy initiated at a BP ≥130/80 mm Hg.1200 Individualize drug therapy in patients with hypertension and underlying cardiovascular or other risk factors.502 1200
In stage 1 hypertension, experts state that it is reasonable to initiate drug therapy using the stepped-care approach in which one drug is initiated and titrated and other drugs are added sequentially to achieve the target BP.1200 Initiation of antihypertensive therapy with 2 first-line agents from different pharmacologic classes recommended in adults with stage 2 hypertension and average BP >20/10 mm Hg above BP goal.1200
Hyperaldosteronism
Has been used to control hypertension and correct electrolyte abnormalities associated with primary hyperaldosteronism† [off-label].a
Also has been used for the management of secondary hyperaldosteronism† [off-label] (Bartter’s syndrome) to correct hypokalemia.a
Diuretic-induced Metabolic Alkalosis
Has been used to correct the metabolic alkalosis† [off-label] produced by thiazides and other kaliuretic diuretics.a
Calcium Nephrolithiasis
Has been used in combination with hydrochlorothiazide in patients with recurrent calcium nephrolithiasis† [off-label].a
Lithium-induced Polyuria
Has been used for the management of lithium-induced polyuria† [off-label] (secondary to lithium-induced nephrogenic diabetes insipidus).100 a (See Specific Drugs, Foods, and Laboratory Tests under Interactions.)
aMILoride Dosage and Administration
General
Monitoring and BP Treatment Goals
-
Monitor BP regularly (i.e., monthly) during therapy and adjust dosage of the antihypertensive drug(s) until BP controlled.1200
-
If unacceptable adverse effects occur, discontinue drug and initiate another antihypertensive agent from a different pharmacologic class.1216
-
If adequate BP response not achieved with a single antihypertensive, either increase dosage of single drug or add a second drug with demonstrated benefit and preferably a complementary mechanism of action (e.g., ACE inhibitor, angiotensin II receptor antagonist, calcium-channel blocker).1200 1216 Many patients will require at least 2 drugs from different pharmacologic classes to achieve BP goal; if goal BP still not achieved with 2 antihypertensive agents, add a third drug.1200 1216 1220
-
Assess patient's renal function and electrolytes 2–4 weeks after initiation of diuretic therapy.1200
-
Monitor serum potassium and other electrolyte concentrations following changes in dosage or with concurrent illness or drug therapy.a b (See Hyperkalemia under Cautions and also see Interactions.)
-
According to some clinicians, amiloride hydrochloride dosage should be reduced to the lowest effective level in any disease state, following initial diuresis with a kaliuretic diuretic.a
-
Do not use fixed-combination amiloride/hydrochlorothiazide tablets for initial therapy of edema or hypertension, except in patients in whom the clinical consequences of hypokalemia represent an important risk (e.g., patients receiving cardiac glycosides, patients with cardiac arrhythmias).a c Adjust dosage by administering each drug separately.a If the optimum maintenance dosage corresponds to the ratio in the commercial combination preparation, the fixed combination may be used.a
Administration
Oral Administration
Administer orally, preferably with food to decrease GI adverse effects.a b
Fixed-combination amiloride/hydrochlorothiazide tablets: Administer orally with food.c
Dosage
Available as amiloride hydrochloride; dosage expressed in terms of the salt.b c
Individualize dosage according to patient’s requirements and response.a
For the management of fluid retention (e.g., edema) associated with heart failure, experts state that diuretics should be administered at a dosage sufficient to achieve optimal volume status and relieve congestion without inducing an excessively rapid reduction in intravascular volume, which could result in hypotension, renal dysfunction, or both.524
Pediatric Patients
Usual Dosage†
Oral
A dosage of 0.625 mg/kg daily has been used in children weighing 6–20 kg†.a
Hypertension†
Oral
Some experts have recommended an initial dosage of 0.4–0.625 mg/kg daily given once daily.111 a Increase dosage as necessary up to a maximum of 20 mg once daily.111 a
Adults
Heart Failure
Combination Therapy
OralUsually combined with a kaliuretic diuretic (e.g., hydrochlorothiazide) to prevent or treat hypokalemia induced by the diuretic.a b
Initially, 5 mg daily;a b 524 increase dosage as necessary to 10 mg daily.a b
If hypokalemia persists after an adequate trial of 10 mg daily may increase dosage to 15 and then 20 mg daily.a b
Dosages exceeding 10 mg daily usually are not necessary, and there is little controlled clinical experience with dosages exceeding 10 mg daily.a b
ACCF and AHA recommend a maximum total daily dosage of 20 mg,524 however, according to some clinicians, the maximum effective daily dosage may be as high as 40 mg.a
Reevaluate need for amiloride therapy following initial diuresis with a kaliuretic diuretic, since potassium loss may decrease.a Subsequent dosage adjustment may be necessary, or amiloride may be used intermittently.a b
Hypertension
Monotherapy
OralUse amiloride alone only when persistent hypokalemia is documented.a b
Initially, 5 mg daily; increase dosage as necessary to 10 mg daily.a b
Titrate dosage carefully and monitor serum electrolytes closely because of increased risk of hyperkalemia with monotherapy.a
If hypokalemia persists after an adequate trial of 10 mg daily, may increase dosage to 15 and then 20 mg daily.a b
Some experts state that the usual dosage range is 5–10 mg daily (given in 1 dose or 2 divided doses).1200 Dosages exceeding 10 mg daily usually are not necessary, and there is little controlled clinical experience with dosages exceeding 10 mg daily.a b
However, some clinicians state maximum effective dosage may be as high as 40 mg daily.a
Combination Therapy
OralUsually combined with a kaliuretic diuretic (e.g., hydrochlorothiazide) to prevent or treat potassium loss induced by the diuretic.a b
Initially, 5 mg daily; increase dosage as necessary to 10 mg daily.a b
If hypokalemia persists after an adequate trial of 10 mg daily, may increase dosage to 15 and then 20 mg daily with careful monitoring of serum electrolytes.a b
Dosages exceeding 10 mg daily usually are not necessary, and there is little controlled clinical experience with dosages exceeding 10 mg daily.a b
According to some clinicians, maximum effective daily dosage may be as high as 40 mg daily.a
The fixed-combination preparation with hydrochlorothiazide should be used for initial antihypertensive therapy only in selected patients in whom the potential development of thiazide-induced hypokalemia cannot be risked.a c (See General under Dosage and Administration.)
Lithium-induced Polyuria
Monotherapy
OralDosages of 5–10 mg twice daily have been effective in the management of lithium-induced polyuria in adults†.100 a (See Specific Drugs, Foods, and Laboratory Tests under Interactions.)
Prescribing Limits
Pediatric Patients
Hypertension†
Oral
Maximum 20 mg once daily.111 a
Adults
Heart Failure
Oral
Maximum 40 mg daily.a
Maximum 20 mg daily recommended by some experts.524
Hypertension
Oral
Maximum 40 mg daily.a
Special Populations
Geriatric Patients
Select dosage with caution because of age-related decreases in hepatic, renal, and/or cardiac function and concomitant disease and drug therapy.b
Cautions for aMILoride
Contraindications
-
Anuria, acute or chronic renal insufficiency, diabetic nephropathy.a b
-
Preexisting hyperkalemia (≥5.5 mEq/L).b
-
Concurrent potassium supplementation (e.g., potassium salts, potassium-containing salt substitutes) except in severe and/or refractory hypokalemia when may be used with careful monitoring of serum potassium concentrations.a b (See Specific Drugs, Foods, and Laboratory Tests under Interactions.)
-
Concurrent therapy with potassium-sparing agents (e.g., spironolactone, triamterene).a b (See Specific Drugs, Foods, and Laboratory Tests under Interactions.)
-
Known hypersensitivity to amiloride or any ingredient in the formulation.a b c
Warnings/Precautions
Warnings
Hyperkalemia
Hyperkalemia (i.e., serum potassium concentrations >5.5 mEq/L) may occur with all potassium-sparing agents, including amiloride.a b c (See Boxed Warning.)
If hyperkalemia occurs, discontinue amiloride immediately.a b
Serum potassium concentrations >6.5 mEq/L require specific measures such as administration of sodium bicarbonate and/or oral or parenteral glucose with a rapid-acting insulin preparation to correct the hyperkalemia.a b If necessary, a cation exchange resin (e.g., sodium polystyrene sulfonate) may be administered orally or as a retention enema.b
Patients with persistent hyperkalemia may require dialysis.a b
Evaluate BUN and serum potassium and creatinine concentrations regularly, especially in patients with suspected or confirmed renal insufficiency.a b Monitor serum potassium concentrations closely in geriatric and diabetic patients.a b Avoid use in diabetic patients, if possible, because of the risk of hyperkalemia.a b
Warning signs of hyperkalemia include paresthesias, muscular weakness, fatigue, flaccid paralysis of the extremities, bradycardia, and shock.a b
Hyperkalemia has been associated with cardiac irregularities.a b ECG changes associated with hyperkalemia are mainly characterized by tall, peaked T waves or elevations since previous tracings.a b Lowering of the R wave and increased depth of the S wave, widening or absence of the P wave, progressive widening of the QRS complex, prolongation of the PR interval, and/or depression of the ST segment also may occur.a b ECG changes do not usually occur in patients who develop mild hyperkalemia during amiloride therapy.a b
Metabolic or Respiratory Acidosis
Use with caution in patients with cardiopulmonary disease or uncontrolled diabetes mellitus because of risk of developing metabolic or respiratory acidosis, which may result in rapid increases in serum potassium concentration.a b Monitor acid-base balance frequently in such patients.a b
General Precautions
Use of Fixed Combinations
When amiloride is used in fixed combination with hydrochlorothiazide, consider the cautions, precautions, and contraindications associated with hydrochlorothiazide.c
Electrolyte Imbalance
Electrolyte disturbance (e.g., hyponatremia, hypochloremia) may occur when amiloride is used with other diuretics.a b
Hypochloremia usually does not require specific treatment except in patients with severe hepatic or renal disease.a
Use appropriate replacement therapy in those who are sodium depleted.a Use water restriction rather than replacement of sodium chloride in edematous patients with dilutional hyponatremia during hot weather, except in rare instances when hyponatremia is life-threatening.a
Despite amiloride’s potassium-sparing effect, hypokalemia may develop in patients receiving amiloride with other diuretics.a
Although amiloride usually prevents hypokalemia associated with thiazide diuretics, some clinicians (using the fixed-dose combination of amiloride and hydrochlorothiazide) have questioned whether 5 mg of amiloride hydrochloride is sufficient to counteract the potassium loss produced by 50 mg of hydrochlorothiazide.a
Renal Effects
Increased BUN concentration may occur, most frequently during forced diuresis in debilitated patients with hepatic cirrhosis with ascites and metabolic alkalosis or in those with resistant edema.a b In such patients, monitor BUN concentration carefully when amiloride is used with other diuretics.a b
Specific Populations
Pregnancy
Lactation
Distributed into milk in animals.a b c Discontinue nursing or the drug.a b
Pediatric Use
Safety and efficacy of amiloride alone or in fixed combination with hydrochlorothiazide not established;a b c however, some experts have suggested an amiloride dosage for hypertension based on limited clinical experience.a (See Pediatric Patients under Dosage and Administration.)
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether geriatric patients respond differently than younger adults.b
Substantially eliminated by kidneys; assess renal function periodically since geriatric patients are more likely to have decreased renal function.b
Hepatic Impairment
Use with caution in patients with severe, preexisting hepatic insufficiency because of risk of hepatic encephalopathy; monitor such patients carefully for signs and symptoms of hepatic encephalopathy.a
Monitor serum electrolyte and BUN concentrations closely in patients with hepatic cirrhosis with ascites and metabolic alkalosis receiving amiloride in combination with other diuretics.a b
Renal Impairment
Use with caution in patients with impaired renal function (BUN concentration >30 mg/dL or Scr >1.5 mg/dL), because of risk of hyperkalemia.a b
Monitor serum electrolyte, creatinine, and BUN periodically; some clinicians recommend weekly determinations during initiation of therapy.a
Common Adverse Effects
Hyperkalemia,b nausea,b vomiting,b diarrhea,b abdominal pain,b flatulence,b anorexia,b mild skin rash,b headache.b
Drug Interactions
Specific Drugs, Foods, and Laboratory Tests
|
Drug, Food, or Test |
Interaction |
Comments |
|---|---|---|
|
ACE inhibitors |
Use caution with concomitant ACE inhibitor therapy; monitor serum potassium concentrations frequentlya b Risk of hyperkalemia may be increased in patients with renal impairmenta Discontinue or reduce dosage of amiloride as necessary in patients receiving an ACE inhibitora |
|
|
Angiotensin II receptor antagonists |
Increased risk of hyperkalemiab |
Use caution with concomitant angiotensin II receptor antagonist therapy; monitor serum potassium concentrations frequentlyb |
|
Antihypertensive agents |
Possible additive antihypertensive effectsa |
Adjust amiloride dosage carefully when drug is added to an antihypertensive regimena |
|
Cyclosporine |
Increased risk of hyperkalemiab |
Use caution with concomitant cyclosporine therapy; monitor serum potassium concentrations frequentlyb |
|
Digoxin |
Possible alteration of response to digoxin therapya |
Observe patient carefully for altered response to digoxin therapya |
|
Diuretics, potassium-sparing (e.g., spironolactone, triamterene) |
Increased risk of hyperkalemiab |
Concomitant use contraindicatedb |
|
Lithium |
Reduced renal clearance of lithium and increased risk of lithium toxicitya b |
Concomitant use generally contraindicated; if concomitant therapy is necessary, monitor serum electrolyte and lithium concentrations, urine output, and serum and urine osmolality and adjust lithium dosage as necessary100 a |
|
NSAIAs (e.g., indomethacin) |
Concomitant use with indomethacin may affect potassium kinetics and renal functiona b Possible decrease in the diuretic, natriuretic, and hypotensive effects of amiloride with concomitant use of NSAIAs101 a b |
Consider potential effects on potassium kinetics and renal function101 a b Observe patient closely to determine whether the desired effect of amiloride is attained101 a b |
|
Potassium supplements, potassium-containing medications (e.g., parenteral penicillin G potassium), and/or foods containing potassium (e.g., salt substitutes, low-salt milk) |
Increased risk of hyperkalemia, especially in patients with renal insufficiencya b |
Concomitant use generally contraindicatedb |
|
Tacrolimus |
Increased risk of hyperkalemiab |
Use with caution; monitor serum potassium concentrations frequentlyb |
|
Tests, glucose tolerance |
Possible severe hyperkalemia following IV glucose tolerance testing in patients with uncontrolled diabetic mellitus receiving short-term administration of amiloridea |
Discontinue amiloride in patients with diabetes mellitus at least 3 days prior to glucose tolerance testinga b |
aMILoride Pharmacokinetics
Absorption
Bioavailability
About 50% of an oral dose is absorbed.a
Onset
Diuretic activity usually occurs within 2 hours.a b
Peak urinary electrolyte excretion within 6–10 hours.a b
Duration
Effect on urinary electrolyte excretion persists for about 24 hours.a b
Food
Food decreases the extent of GI absorption to about 30%, but does not affect the rate of absorption.a
Distribution
Extent
Crosses the placenta in animals; not known whether crosses placenta in humans.a
Distributed into milk in animals; not known whether distributed into human milk.a
Elimination
Metabolism
Not metabolized in the liver.b
Elimination Route
Excreted in urine (50%) as unchanged drug and in feces (40%), possibly as unabsorbed drug.a b
Half-life
Special Populations
Renal clearance may be reduced in patients with renal impairment.a b
Stability
Storage
Oral
Tablets
<40°C (preferably 15–30°C);a protect from moisture, freezing, and excessive heat.a b
Fixed Combination Tablets with Hydrochlorothiazide
15–30°C; protect from light, moisture, and freezing.c
Actions
-
Exhibits potassium-sparing effect when used with kaliuretic diuretics.b
-
Exerts potassium-sparing effect by decreasing sodium reabsorption in the distal tubule and reducing both potassium and hydrogen secretion and subsequent excretion.a b
-
Exhibits weak natriuretic, diuretic, and hypotensive effects.a b
-
Does not competitively inhibit aldosterone; activity is independent of aldosterone concentrations.a b
-
Does not inhibit carbonic anhydrase and has no effect on free water clearance or concentrating mechanisms.a
-
Increases urinary excretion of sodium, calcium, and bicarbonate with little, if any, increase in chloride excretion.a
-
Concomitant administration with a more potent natriuretic diuretic results in approximately additive effects of the drugs on urinary sodium excretion and an antagonistic effect on potassium excretion.a
-
May increase urinary aldosterone and plasma renin concentrations, probably as a compensatory feedback mechanism caused by potassium retention and natriuresis.a
-
Unlike thiazide diuretics, does not consistently inhibit the excretion of uric acid; has variable effects on serum uric acid concentration.a
-
Does not appear to be diabetogenic or to alter carbohydrate metabolism in humans.a
Advice to Patients
-
Importance of taking drug with food to help avoid stomach upset.a b
-
Importance of avoiding ingestion of potassium supplements, salt substitutes, or excessive amounts of potassium-rich foods.b
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.a
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.a
-
Importance of informing patients of other important precautionary information.a (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
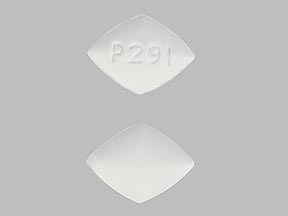
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
5 mg* |
Amiloride Hydrochloride Tablets |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
5 mg Amiloride Hydrochloride and Hydrochlorothiazide 50 mg* |
Amiloride Hydrochloride and Hydrochlorothiazide Tablets |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions April 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
100. Battle DC, von Riotte AB, Gaviria M et al. Amelioration of polyuria by amiloride in patients receiving long-term lithium therapy. N Engl J Med. 1985; 312:408-14. https://pubmed.ncbi.nlm.nih.gov/3969096
101. Merck & Co. Midamor (amiloride hydrochloride) tablets prescribing information. West Point, PA; 1992 Apr.
103. Anon. Consensus recommendations for the management of chronic heart failure. On behalf of the membership of the advisory council to improve outcomes nationwide in heart failure. Part II. Management of heart failure: approaches to the prevention of heart failure. Am J Cardiol. 1999; 83:9-38A.
104. The Captopril-Digoxin Multicenter Research Group. Comparative effects of therapy with captopril and digoxin in patients with mild to moderate heart failure. JAMA. 1988; 259:539-44. https://pubmed.ncbi.nlm.nih.gov/2447297
105. Richardson A, Bayliss J, Scriven AJ et al. Double-blind comparison of captopril alone against frusemide plus amiloride in mild heart failure. Lancet. 1987; 2:709-11. https://pubmed.ncbi.nlm.nih.gov/2888942
106. Sherman LG, Liang CS, Baumgardner S et al. Piretanide, a potent diuretic with potassium-sparing properties, for the treatment of congestive heart failure. Clin Pharmacol Ther. 1986; 40:587-94. https://pubmed.ncbi.nlm.nih.gov/3533372
107. Patterson JH, Adams KF Jr, Applefeld MM et al. Oral torsemide in patients with chronic congestive heart failure: effects on body weight, edema, and electrolyte excretion. Pharmacotherapy. 1994; 14:514-21. https://pubmed.ncbi.nlm.nih.gov/7997385
108. Wilson JR, Reichek N, Dunkman WB et al. Effect of diuresis on the performance of the failing left ventricle in man. Am J Med. 1981;70:234-9.
109. Parker JO. The effects of oral ibopamine in patients with mild heart failure—a double blind placebo controlled comparison to furosemide. Int J Cardiol. 1993; 40:221-7. https://pubmed.ncbi.nlm.nih.gov/8225657
111. National high blood pressure education program working group on hypertension control in children and adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004; 114(Suppl 2):555-76. https://pubmed.ncbi.nlm.nih.gov/15286277
500. National Heart, Lung, and Blood Institute National High Blood Pressure Education Program. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7). Bethesda, MD: National Institutes of Health; 2004 Aug. (NIH publication No. 04-5230.)
501. James PA, Oparil S, Carter BL et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014; 311:507-20. https://pubmed.ncbi.nlm.nih.gov/24352797
502. Mancia G, Fagard R, Narkiewicz K et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013; 31:1281-357. https://pubmed.ncbi.nlm.nih.gov/23817082
503. Go AS, Bauman MA, Coleman King SM et al. An effective approach to high blood pressure control: a science advisory from the American Heart Association, the American College of Cardiology, and the Centers for Disease Control and Prevention. Hypertension. 2014; 63:878-85. https://pubmed.ncbi.nlm.nih.gov/24243703
504. Weber MA, Schiffrin EL, White WB et al. Clinical practice guidelines for the management of hypertension in the community: a statement by the American Society of Hypertension and the International Society of Hypertension. J Clin Hypertens (Greenwich). 2014; 16:14-26. https://pubmed.ncbi.nlm.nih.gov/24341872
505. Wright JT, Fine LJ, Lackland DT et al. Evidence supporting a systolic blood pressure goal of less than 150 mm Hg in patients aged 60 years or older: the minority view. Ann Intern Med. 2014; 160:499-503. https://pubmed.ncbi.nlm.nih.gov/24424788
506. Mitka M. Groups spar over new hypertension guidelines. JAMA. 2014; 311:663-4. https://pubmed.ncbi.nlm.nih.gov/24549531
507. Peterson ED, Gaziano JM, Greenland P. Recommendations for treating hypertension: what are the right goals and purposes?. JAMA. 2014; 311:474-6. https://pubmed.ncbi.nlm.nih.gov/24352710
508. Bauchner H, Fontanarosa PB, Golub RM. Updated guidelines for management of high blood pressure: recommendations, review, and responsibility. JAMA. 2014; 311:477-8. https://pubmed.ncbi.nlm.nih.gov/24352759
515. Thomas G, Shishehbor M, Brill D et al. New hypertension guidelines: one size fits most?. Cleve Clin J Med. 2014; 81:178-88. https://pubmed.ncbi.nlm.nih.gov/24591473
523. Fihn SD, Gardin JM, Abrams J et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation. 2012; 126:e354-471.
524. WRITING COMMITTEE MEMBERS, Yancy CW, Jessup M et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013; 128:e240-327.
526. Kernan WN, Ovbiagele B, Black HR et al. Guidelines for the Prevention of Stroke in Patients With Stroke and Transient Ischemic Attack: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2014; 45:2160-2236. https://pubmed.ncbi.nlm.nih.gov/24788967
530. Myers MG, Tobe SW. A Canadian perspective on the Eighth Joint National Committee (JNC 8) hypertension guidelines. J Clin Hypertens (Greenwich). 2014; 16:246-8. https://pubmed.ncbi.nlm.nih.gov/24641124
536. Kidney Disease: Improving Global Outcomes (KDIGO) Blood Pressure Work Group. KDIGO clinical practice guideline for the management of blood pressure in chronic kidney disease. Kidney Int Suppl. 2012: 2: 337-414.
700. Yancy CW, Jessup M, Bozkurt B et al. 2016 ACC/AHA/HFSA Focused Update on New Pharmacological Therapy for Heart Failure: An Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation. 2016; :.
713. Gupta D, Georgiopoulou VV, Kalogeropoulos AP et al. Dietary sodium intake in heart failure. Circulation. 2012; 126:479-85. https://pubmed.ncbi.nlm.nih.gov/22825409
723. Hummel SL, Konerman MC. Dietary Sodium Restriction in Heart Failure: A Recommendation Worth its Salt?. JACC Heart Fail. 2016; 4:36-8. https://pubmed.ncbi.nlm.nih.gov/26738950
724. Yancy CW. The Uncertainty of Sodium Restriction in Heart Failure: We Can Do Better Than This. JACC Heart Fail. 2016; 4:39-41. https://pubmed.ncbi.nlm.nih.gov/26738951
1200. Whelton PK, Carey RM, Aronow WS et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018; 71:el13-e115. https://pubmed.ncbi.nlm.nih.gov/29133356
1201. Bakris G, Sorrentino M. Redefining hypertension - assessing the new blood-pressure guidelines. N Engl J Med. 2018; 378:497-499. https://pubmed.ncbi.nlm.nih.gov/29341841
1202. Carey RM, Whelton PK, 2017 ACC/AHA Hypertension Guideline Writing Committee. Prevention, detection, evaluation, and management of high blood pressure in adults: synopsis of the 2017 American College of Cardiology/American Heart Association hypertension guideline. Ann Intern Med. 2018; 168:351-358. https://pubmed.ncbi.nlm.nih.gov/29357392
1207. Burnier M, Oparil S, Narkiewicz K et al. New 2017 American Heart Association and American College of Cardiology guideline for hypertension in the adults: major paradigm shifts, but will they help to fight against the hypertension disease burden?. Blood Press. 2018; 27:62-65. https://pubmed.ncbi.nlm.nih.gov/29447001
1209. Qaseem A, Wilt TJ, Rich R et al. Pharmacologic treatment of hypertension in adults aged 60 years or older to higher versus lower blood pressure targets: a clinical practice guideline from the American College of Physicians and the American Academy of Family Physicians. Ann Intern Med. 2017; 166:430-437. https://pubmed.ncbi.nlm.nih.gov/28135725
1210. SPRINT Research Group, Wright JT, Williamson JD et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015; 373:2103-16. https://pubmed.ncbi.nlm.nih.gov/26551272
1216. Taler SJ. Initial treatment of hypertension. N Engl J Med. 2018; 378:636-644. https://pubmed.ncbi.nlm.nih.gov/29443671
1220. Cifu AS, Davis AM. Prevention, detection, evaluation, and management of high blood pressure in adults. JAMA. 2017; 318:2132-2134. https://pubmed.ncbi.nlm.nih.gov/29159416
1222. Bell KJL, Doust J, Glasziou P. Incremental benefits and harms of the 2017 American College of Cardiology/American Heart Association high blood pressure guideline. JAMA Intern Med. 2018; 178:755-7. https://pubmed.ncbi.nlm.nih.gov/29710197
1223. LeFevre M. ACC/AHA hypertension guideline: what is new? what do we do?. Am Fam Physician. 2018; 97(6):372-3. https://pubmed.ncbi.nlm.nih.gov/29671534
1224. Brett AS. New hypertension guideline is released. From NEJM Journal Watch website. Accessed 2018 Jun 18. https://www.jwatch.org/na45778/2017/12/28/nejm-journal-watch-general-medicine-year-review-2017
1229. Ioannidis JPA. Diagnosis and treatment of hypertension in the 2017 ACC/AHA guidelines and in the real world. JAMA. 2018; 319(2):115-6. https://pubmed.ncbi.nlm.nih.gov/29242891
a. AHFS Drug Information 2017. McEvoy GK, ed. Amiloride hydrochloride. American Society of Health-System Pharmacists; 2017: .
b. Merck & Co., Inc. Midamor (amiloride HCl) tablets prescribing information. Whitehouse Station, NJ; 2002 Nov.
c. Merck & Co., Inc. Moduretic (amiloride HCl-hydrochlorothiazide) tablets prescribing information. Whitehouse Station, NJ; 2002 Nov.
Related/similar drugs
More about amiloride
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (5)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: potassium-sparing diuretics
- Breastfeeding
- En español