Amantadine Hydrochloride (Antiparkinson) (Monograph)
Drug class: Adamantanes
Introduction
Synthetic adamantane derivative that has pharmacologic activity as an antiparkinson and antiviral agent.
Uses for Amantadine Hydrochloride (Antiparkinson)
Parkinsonian Syndrome
Treatment of parkinsonism, including idiopathic parkinson disease (paralysis agitans) and parkinsonism resulting from encephalitis (postencephalitic parkinsonism), carbon monoxide intoxication, or cerebral arteriosclerosis.
Various preparations are commercially available for this use, including immediate-release and extended-release formulations.
Levodopa (in combination with carbidopa) is currently the most effective drug for relieving the motor symptoms of parkinson disease; however, effectiveness decreases over time as the disease progresses and most patients develop motor complications (e.g., motor fluctuations, dyskinesias) with long-term use. Strategies for reducing the risk of motor complications include adjusting the dosage of levodopa or adding other antiparkinsonian agents such as amantadine.
Amantadine extended-release capsules are specifically indicated for the treatment of dyskinesia in patients with parkinson disease receiving levodopa-based therapy, with or without concomitant dopaminergic medications, and as adjunctive treatment to levodopa/carbidopa in patients with parkinson disease experiencing "off" episodes.
Drug-induced Extrapyramidal Effects
Treatment of drug-induced extrapyramidal symptoms (EPS).
Generally used in patients with antipsychotic-induced pseudoparkinsonism and appears to be as effective as anticholinergic agents for this type of EPS.
Amantadine may be especially useful when anticholinergic agents should be avoided (e.g., in patients with glaucoma or urinary retention).
Amantadine Hydrochloride (Antiparkinson) Dosage and Administration
General
Patient Monitoring
-
Patients with a history of seizures should be observed closely for possible increased seizure activity.
-
Monitor patients for impulse control/compulsive behaviors such as intense urges to gamble, increased sexual urges, uncontrolled spending, or other urges.
-
Monitor patients for depression, including suicidal ideation or behavior.
-
Monitor patients frequently and regularly for melanoma; periodic skin examinations should be performed by appropriately qualified individuals (e.g., dermatologists).
-
Monitor patients for dizziness and orthostatic hypotension, especially after starting therapy or increasing the dosage.
-
Monitor patients for hallucinations throughout treatment, particularly after initiation of therapy and after dosage changes.
Other General Considerations
-
Do not discontinue amantadine treatment abruptly in patients with parkinson disease.
-
When discontinuing therapy, taper dosage gradually.
Administration
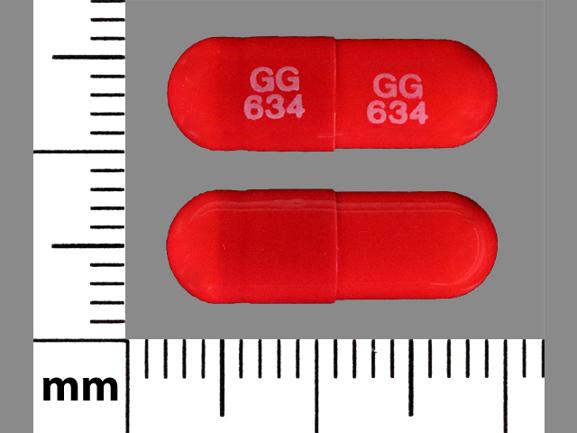
Administer orally as conventional (i.e., immediate-release) tablets, conventional capsules, extended-release capsules, or conventional oral solution.
Conventional preparations: commercially available as tablets or liquid-filled capsules containing 100 mg of the drug or as an oral solution containing 50 mg/5 mL.
Extended-release capsules: administer orally once daily at bedtime with or without food. Swallow capsules whole; do not crush, chew, or divide. If necessary, capsules may be opened and contents sprinkled on a small amount (e.g., teaspoonful) of soft food such as applesauce; swallow the drug/food mixture immediately without chewing and do not store for later use.
Dosage
Dosage of amantadine hydrochloride conventional tablets, capsules, and oral solution is expressed in terms of amantadine hydrochloride; dosage of amantadine hydrochloride extended-release capsules is expressed in terms of amantadine.
Adults
Parkinsonism
Conventional (Immediate-release) Preparations
OralUsual dosage of conventional tablets, capsules, or oral solution is 100 mg twice daily.
In patients receiving high dosages of other antiparkinsonian drugs or with other serious comorbid illnesses, recommended initial dosage is 100 mg daily; after one to several weeks, may increase dosage to 100 mg twice daily if necessary.
Some patients may benefit from a dosage increase up to 400 mg daily in divided doses. Closely monitor patients receiving a daily dosage of 400 mg.
Patients who initially benefit from amantadine may experience a decrease in effectiveness after a few months of therapy. If loss of effectiveness occurs, benefit may be regained by increasing the dosage to 300 mg daily. Alternatively, temporary discontinuation of the drug for several weeks, followed by reinstitution of amantadine therapy may result in regained benefit in some patients. The use of other antiparkinsonian agents may be necessary. If amantadine and levodopa therapy are initiated concurrently, the manufacturer recommends that amantadine hydrochloride dosage be continued at 100 mg once or twice daily while the daily dosage of levodopa is gradually increased to optimal benefit.
Usual dosage may need to be reduced in patients with CHF, peripheral edema, orthostatic hypotension, or impaired renal function.
Extended-release Capsules
OralFor treatment of dyskinesia or "off" episodes in patients with parkinson disease receiving levodopa-based therapy, recommended initial dosage is 137 mg once daily at bedtime. Increase dosage after 1 week to recommended dosage of 274 mg (given as two 137-mg capsules) once daily at bedtime.
When discontinuing therapy in patients who have been receiving the drug for more than 4 weeks, reduce dose by half, if possible, during the final week of dosing.
If a dose is missed, the next dose should be taken at the regularly scheduled time.
Drug-induced Extrapyramidal Reactions
Conventional (Immediate-release) Preparations
OralUsual dosage is 100 mg twice daily.
Occasionally, patients with a suboptimal response at a dosage of 200 mg daily may benefit from a dosage increase to 300 mg daily in divided doses.
Usual dosage may need to be reduced in patients with CHF, peripheral edema, orthostatic hypotension, or impaired renal function.
Special Populations
Hepatic Impairment
Manufacturers make no dosage adjustment recommendations for patients with hepatic impairment.
Renal Impairment
Conventional preparations:Patients with Clcr 30–50 mL/minute per 1.73 m2 should receive 200 mg on the first day, followed by 100 mg daily; patients with Clcr 15–29 mL/minute per 1.73 m2 should receive 200 mg on the first day, followed by 100 mg on alternate days. Patients with Clcr <15 mL/minute per 1.73 m2 and hemodialysis patients should receive 200 mg every 7 days.
Extended-release capsules: Dosage adjustment not required in patients with mild renal impairment (Clcr 60–89 mL/minute per 1.73 m2). In patients with moderate renal impairment (Clcr 30–59 mL/minute per 1.73 m2), reduce initial dosage to 68.5 mg once daily at bedtime; if needed, may increase dosage in 1 week to maximum of 137 mg once daily. In patients with severe renal impairment (Clcr 15–29 mL/minute per 1.73 m2), recommended dosage is 68.5 mg once daily at bedtime. Contraindicated in patients with end-stage renal disease (Clcr <15 mL/minute per 1.73 m2).
Closely monitor patients with any degree of renal impairment for adverse reactions; further dosage reductions may be necessary.
Geriatric Patients
Reduce dosage of amantadine conventional preparations in geriatric patients ≥65 years of age.
Manufacturer of extended-release capsule states no dosage adjustment required based on age; however, select dosage with caution and monitor renal function in elderly patients.
Cautions for Amantadine Hydrochloride (Antiparkinson)
Contraindications
-
Patients with known hypersensitivity to amantadine hydrochloride or any ingredients in the formulations.
Warnings/Precautions
Deaths from Overdosage
Deaths from overdosage have occurred. Acute toxicity may be attributed to the anticholinergic effects of the drug.
Overdosage also reported in patients with renal impairment who were prescribed higher than recommended doses.
Suicidality and Depression
Suicide attempts (sometimes resulting in death) and suicidal ideation reported; in many cases, patients received short courses of the drug for influenza prophylaxis or treatment.
Monitor patients for depression, including suicidal ideation and behavior.
Weigh risks versus benefits of treatment in patients with a history of suicidality or depression.
Hallucinations and Psychotic Behavior
Hallucinations and other psychiatric symptoms (e.g., confusion, psychosis, personality changes, agitation, aggressive behavior, paranoia) reported.
Monitor patients for these effects, particularly after initiation of therapy and when dosage is increased or decreased.
Use of amantadine generally not advised in patients with major psychotic disorders because of risk of exacerbating psychosis.
CNS Effects
Possible increased seizure frequency in patients with active seizure disorders. Seizures also reported in patients with renal impairment and in geriatric individuals.
Observe patients with a history of seizures closely for possible increased seizure activity.
May impair ability to perform hazardous activities requiring mental alertness or physical coordination such as operating machinery or driving a motor vehicle.
Falling Asleep During Activities of Daily Living
Episodes of falling asleep while engaged in activities of daily living (e.g., driving) reported; sometimes resulting in accidents.
Some patients perceived no warning signs (e.g., excessive drowsiness) and believed they were alert immediately prior to the event.
Patients may not acknowledge drowsiness or sleepiness until directly questioned about such adverse effects during specific activities. Ask patients about any factors that may increase the risk of somnolence (e.g., concomitant sedating drugs or alcohol, presence of sleep disorders).
In general, discontinue therapy if a patient develops daytime sleepiness or episodes of falling asleep during activities that require active participation (e.g., conversations, eating). If the drug is continued, advise patient not to drive and to avoid other potentially dangerous activities. Insufficient information to establish whether dosage reduction will eliminate this adverse event.
Dizziness and Orthostatic Hypotension
Dizziness and orthostatic hypotension reported.
Monitor patients for signs and symptoms of orthostatic hypotension, particularly after initiation of therapy and when dosage is increased.
Withdrawal-Emergent Hyperpyrexia and Confusion
A symptom complex resembling possible neuroleptic malignant syndrome (NMS; characterized by fever, muscular rigidity, altered consciousness, autonomic instability) reported with drugs that increase central dopaminergic tone; observed with rapid dosage reduction or withdrawal of drug.
Observe patients carefully when dosage is reduced abruptly or treatment is discontinued.
Impulse Control and Compulsive Behaviors
Intense urges (e.g., urge to gamble, increased sexual urges, binge eating, uncontrolled spending, other intense urges) and inability to control these urges reported with drugs that increase central dopaminergic tone.
Consider reducing dosage or discontinuing therapy if a patient develops such urges.
Melanoma
Melanoma observed more frequently in patients with parkinson disease than in the general population.
Monitor for melanoma on a frequent and regular basis. Periodic dermatologic screening is recommended by some manufacturers.
Specific Populations
Pregnancy
Embryotoxic/teratogenic effects observed in animal studies. No adequate and well-controlled studies in pregnant women. Use during pregnancy only when potential benefits outweigh possible risks to fetus.
Lactation
Distributed into human milk; some manufacturers state that the drug should not be used in nursing women.
Pediatric Use
Safety and efficacy not established in pediatric patients; the majority of individuals with parkinson disease are ≥65 years of age.
When used in children, amantadine has caused CNS symptoms, which resolved when the drug was discontinued.
Increased incidence of seizures reported in children with an underlying seizure disorder receiving amantadine.
Geriatric Use
Majority of individuals with parkinson disease are ≥65 years of age. Geriatric patients may have renal decline; reduced dosages may therefore be needed.
Hepatic Impairment
Use care when administering amantadine to patients with liver disease. Rare cases of reversible elevation of liver enzymes reported.
Renal Impairment
Mainly excreted in the urine; drug accumulation may occur when renal function declines. Reduced dosages recommended in patients with renal impairment.
Common Adverse Effects
Most common adverse effects (5–10%) with conventional (immediate-release) preparations: nausea, dizziness, insomnia.
Most common adverse effects (>10%) with extended-release capsules: hallucination, dizziness, dry mouth, peripheral edema, constipation, fall, orthostatic hypotension.
Drug Interactions
Does not significantly inhibit CYP isoenzymes 1A2, 2B6, 2C19, 2C8, 2C9, 2D6, 2E1, 3A4, and 3A5.
Negligible or no inhibitory activity against transporters (P-gp, BCRP, MATE2-K, OAT1, OAT3, OATP1B1, and OATP1B3).
Drugs with Anticholinergic Activity
Concomitant use with other drugs with anticholinergic activity may result in increased adverse anticholinergic effects; reduce dosage of the anticholinergic agent or amantadine if atropine-like effects occur when these drugs are used concomitantly.
Drugs Affecting Urinary pH
Excretion rate of amantadine increases rapidly when the urine is acidic; administration of urine acidifying drugs may increase elimination of the drug.
Alterations of urine pH towards alkaline condition may lead to drug accumulation, possibly increasing adverse reactions.
Monitor for efficacy or adverse reactions of amantadine in situations where urine pH may be altered to a more acidic or alkaline state, respectively.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Alcohol |
Potential for increased risk of CNS effects |
Concomitant use not recommended |
|
CNS stimulants |
Possible additive CNS stimulant effects |
Administer amantadine with caution in patients receiving other CNS stimulant drugs |
|
Co-trimoxazole |
Toxic delirium has occurred following initiation of co-trimoxazole in at least one patient who had been stabilized on amantadine |
|
|
Influenza virus vaccine |
Amantadine may interfere with the efficacy of live attenuated influenza vaccines |
Live vaccines are not recommended during treatment with amatadine Inactivated influenza vaccines may be used, as appropriate |
|
Quinine or quinidine |
May reduce the renal clearance of amantadine |
|
|
Thioridazine |
Worsened tremor in geriatric patients with parkinsonian syndrome reported; not known whether similar effect could occur with other phenothiazines |
|
|
Triamterene and hydrochlorothiazide |
Increased plasma concentrations of amantadine reported; however, it is not known which component of the combination preparation may have been responsible for the interaction |
Amantadine Hydrochloride (Antiparkinson) Pharmacokinetics
Absorption
Bioavailability
Well absorbed from the GI tract.
While peak plasma concentrations are directly related to dosages up to 200 mg daily, higher dosages may result in a greater than proportional increases in peak plasma concentration.
Following oral administration of extended-release capsules, dose-proportional pharmacokinetics observed over dose range of 68.5–274 mg. Time to peak plasma concentrations after a single dose is approximately 12 hours.
Food
Food does not affect pharmacokinetics when given as the extended-release capsules; administration of capsule contents with applesauce also did not affect pharmacokinetics of the drug.
Distribution
Protein Binding
Approximately 67% bound to plasma proteins.
Elimination
Elimination Route
Principally excreted unchanged in urine by glomerular filtration and tubular secretion; at least 8 metabolites have been identified in urine.
Not appreciably removed by dialysis.
Half-life
9–37 hours, with an average of 24 hours or less.
Stability
Storage
Oral
Conventional Preparations
20–25°C (excursions permitted between 15–30°C); dispense in tight, light-resistant container.
Extended-release Capsules
20–25°C (excursions permitted between 15–30°C); dispense in tight container.
Actions
-
Synthetic adamantane derivative.
-
Exact mechanism of action not known.
-
Weak uncompetitive antagonist of the NMDA receptor; may have direct and indirect effect on the dopaminergic system.
Advice to Patients
-
Advise the patient to read the FDA-approved patient labeling (Patient Information).
-
Instruct patients on proper administration of the specific dosage form of amantadine prescribed.
-
Advise patients that sleepiness and fatigue have been reported with amantadine and patients treated with parkinson disease drugs have reported falling asleep while engaged in activities of daily living. These adverse reactions may affect the ability to drive and operate machinery safely.
-
Advise patients that blurry vision and/or impaired mental acuity may occur.
-
Advise patients to gradually increase physical activity as the symptoms of parkinson disease improve.
-
Inform patients and caregivers that hallucinations and paranoia can occur while taking amantadine. Advise patients to report unreal visions, sounds, or sensations or other psychotic behavior to their healthcare provider promptly should they develop.
-
Inform patients of the potential for experiencing intense urges to gamble, increased sexual urges, intense urges to spend money, binge eating, and other intense urges and the inability to control these urges while taking one or more drugs that increase central dopaminergic tone.
-
Advise patients to contact their healthcare provider before stopping amantadine. Advise patients to inform their healthcare provider if they develop withdrawal symptoms such as fever, confusion, or severe muscle stiffness.
-
Advise patients to avoid excessive alcohol usage, since it may increase the potential for CNS effects such as dizziness, confusion, lightheadedness, and orthostatic hypotension.
-
Advise patients to avoid getting up suddenly from a sitting or lying position. If dizziness or lightheadedness occurs, notify a physician.
-
Instruct patients, family members, and caregivers to notify their healthcare provider if depressed mood, depression, changes in behavior or thinking, and suicidal ideation or behavior develop during treatment.
-
Advise patients to not take more medication than prescribed because of the risk of overdose. If there is no improvement in a few days, or if the drug appears less effective after a few weeks, discuss with a physician. Advise patients to seek medical attention immediately if a suspected overdosage has occurred.
-
Advise patients to inform their clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as any concomitant illnesses.
-
Advise women to inform their clinician if they are or plan to become pregnant or plan to breast-feed.
-
Inform patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules |
100 mg* |
Amantadine Hydrochloride Capsules |
|
|
Capsules, extended-release |
68.5 mg (of amantadine) |
Gocovri |
Adamas |
|
|
137 mg (of amantadine) |
Gocovri |
Adamas |
||
|
Solution |
50 mg/5 mL* |
Amantadine Hydrochloride Solution |
||
|
Tablets |
100 mg* |
Amantadine Hydrochloride Tablets |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions September 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Frequently asked questions
- What is the difference between Osmolex ER and Gocovri?
- What is Gocovri used to treat?
- Why should you not discontinue amantadine?
- How long does it take for amantadine to start working?
- Why was amantadine discontinued for flu?
- What symptoms does amantadine treat?
- What is Gocovri (amantadine) and how does it work?
More about amantadine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (54)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: adamantane antivirals
- Breastfeeding
- En español
Patient resources
Professional resources
- Amantadine Hydrochloride (Antiviral) monograph
- Amantadine (FDA)
- Amantadine Oral Solution USP (FDA)
- Amantadine Syrup (FDA)
- Amantadine Tablets (FDA)