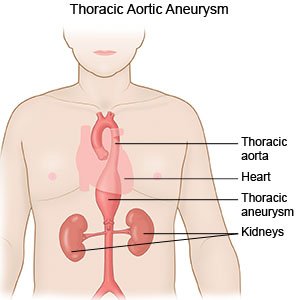
Thoracic Aortic Aneurysm
Medically reviewed by Drugs.com. Last updated on Mar 10, 2025.
What is a thoracic aortic aneurysm (TAA)?
A TAA is a bulge in the upper part of your aorta. The aorta is a large blood vessel that goes from your heart down into your abdomen. The aortic valve opens to let blood flow from your heart into your aorta. The valve then closes to stop blood flowing back into your heart. A TAA can occur if the aorta or its valve is damaged, weakened, or not formed correctly. A TAA may continue to grow and rupture (burst), or it may dissect (tear) suddenly. A TAA that bursts or tears is a life-threatening emergency.
 |
What increases my risk for a TAA?
Your risk is increased if you are male or aged 60 or older. The most common risk factors are high blood pressure (BP), high cholesterol, and atherosclerosis (hard or stiff arteries). Any of the following can also increase your risk for a TAA:
- A genetic condition that affects your heart, aorta, or aortic valve
- A connective tissue disorder such as Marfan syndrome or vascular Ehlers-Danlos syndrome
- A family history of TAA
- Cigarette or cocaine use
- Diabetes
- Excess body weight or obesity
- A history of a tear in or injury to your aorta
What are the signs and symptoms of a TAA?
You may have no signs or symptoms. You may have any of the following if your TAA grows, bursts, or tears:
- Pain in your chest, neck, back, or abdomen
- A cough or wheeze
- Hoarse voice
- Trouble swallowing or pain when you swallow
- Trouble breathing or shortness of breath
- Coughing or vomiting up blood
How is a TAA diagnosed?
A TAA may be diagnosed when you have a test done for another condition. Your healthcare provider will examine you and ask about your medical history. Tell the provider if you have any symptoms and when they started. Tell your provider about any medicines you take. You may need any of the following:
- A CT, PET scan, MRI, or ultrasound may show your TAA or a condition causing your TAA. You may be given contrast liquid before the scan. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid. Do not enter the MRI room with anything metal. Metal can cause serious injury. Tell the healthcare provider if you have any metal in or on your body.
- An echocardiogram uses sound waves to show pictures on a monitor. It is used to check your aorta for a TAA. It may also show how well blood flows through your heart and how well your heart is pumping.
- An x-ray may show a genetic condition that is causing your TAA. It may instead show atherosclerosis or signs of bleeding in your chest.
How is a TAA treated?
- Blood pressure (BP) medicine helps lower your BP to prevent your TAA from growing, tearing, or bursting.
- Cholesterol medicine may be needed to lower your cholesterol level to help prevent atherosclerosis.
- Antiplatelets , such as aspirin, help prevent blood clots. Take your antiplatelet medicine exactly as directed. These medicines make it more likely for you to bleed or bruise. If you are told to take aspirin, do not take acetaminophen or ibuprofen instead.
- Endovascular repair is a procedure that uses a graft to prevent your TAA from tearing or bursting. A graft is a wire mesh tube that can also protect your aorta. You may need more than 1 endovascular repair.
- Surgery may be needed to repair your aorta or remove an aneurysm. You may instead need surgery to replace part of your aorta. Your aortic valve may also be replaced if it is not working well.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
Drugs used to treat this and similar conditions
Metoprolol
Metoprolol is used to treat angina (chest pain) and hypertension (high blood pressure). Learn about ...
How can I manage a TAA?
Your healthcare provider may recommend cardiac rehabilitation (rehab). Cardiac rehab is a program run by a team of specialists who will help you create a management plan. Your plan may include these or other guidelines:
- Manage other health conditions to help prevent your TAA from growing or bursting. Examples are stress, high cholesterol, and high BP. Manage stress by learning new ways to relax, such as listening to music. High cholesterol can increase your risk for atherosclerosis. Take medicine as directed and follow your treatment plan. Check your BP as directed if you have high BP. Your provider will show you how to do this. Check your BP 2 times, 1 minute apart. Check as often as directed each day. Keep a record of your readings and bring it to your follow-up visits.

- Follow the meal plan set by your provider. Talk to your provider or dietitian about a heart-healthy or low-sodium meal plan. Heart-healthy meal plans are low in sodium, processed sugar, and some fats. They are high in potassium, calcium, heart-healthy fats, and fiber. These can be found in vegetables, fruit, and whole-grain foods. A meal plan can help you lower your cholesterol and BP levels. A plan can also help you reach and maintain a healthy weight. Excess weight can cause a TAA or make it grow. Ask your provider what a healthy weight is for you. Ask your provider to help you create a weight loss plan, if needed.

- Follow physical activity directions. Your physical activity plan may include low-intensity activity, such as walking, yoga, or swimming. Regular physical activity can help decrease your BP, cholesterol, and stress levels. You may need to avoid intense physical activity, such as weightlifting or running. Intense activity may raise your BP or put pressure on your aorta. These increase your risk for a tear or rupture. You may also need to avoid contact sports such as football to decrease your risk for a chest injury.
- Know the risks if you choose to drink alcohol. Alcohol can increase your BP. Ask your provider if it is okay for you to drink any alcohol. Your provider can help you set limits for the number of drinks you have in 24 hours and within 1 week. A drink of alcohol is 12 ounces of beer, 5 ounces of wine, or 1½ ounces of liquor.
- Do not use nicotine products or stimulating drugs. Nicotine and drugs such as cocaine increase the risk for your TAA to tear or burst. Ask your provider for information if you currently smoke or use stimulating drugs and need help to quit. E- cigarettes or smokeless tobacco still contain nicotine. Do not use these in place of cigarettes. Avoid secondhand smoke.
- Get vaccines as directed. Some viruses can worsen a TAA. Get an influenza (flu) vaccine as soon as recommended each year, usually in September or October. Get all recommended COVID-19 vaccine doses and boosters. A pneumonia vaccine may also be recommended. Your provider will tell you if you need other vaccines, and when to get them.
What do I need to know about family planning?
- Before you try to get pregnant, talk to your specialist about family planning. Genetic counseling may be needed if your TAA is caused by a condition that can be passed to your baby. You may need counseling if your condition can put you or your pregnancy at risk. You may instead need counseling about the risk of pregnancy making your TAA grow, tear, or burst. You may also need tests to check your TAA. These tests can help you and your provider plan treatment before and during your pregnancy. You may need surgery to protect your aorta and prevent your TAA from growing, tearing, or bursting.
- While you are pregnant, you may have 1 or more specialist caring for you. You may need medicine to help lower your BP. You may need regular tests to check your TAA. You may need other medicines or surgery if your TAA grows, tears, or bursts. Your baby may need to be born early if your aorta tears or bursts. A cesarean section (C-section) may be needed if you have a history of a tear in your aorta. You may need a C-section if you have a high risk for a burst aneurysm or tear.
- After your baby is born, you may need tests to check your TAA. Your risk for a burst aneurysm or tear is high for up to 12 weeks.
What do I need to know about screening for a TAA?
Your healthcare provider can give you specific information about your screening. The following is general information:
- Screening means you are checked 1 time based on family history of TAA and your personal risk factors. You may need a CT, MRI, or echocardiogram to check your aorta. You may also need a blood test to check for a genetic condition that can cause a TAA.
- Your parents, siblings, and children may need screening. More family members may also need screening if 2 or more people in your family had a TAA. Your provider will tell you which family members need screening.
- The benefit of screening is that your provider can diagnose a TAA early. This helps your provider monitor your TAA and start treatment, if needed. This can help prevent your TAA from growing, bursting, or tearing. Screening can also help you plan a healthy pregnancy.
Call your local emergency number (911 in the US) or have someone call if:
- You have any of the following signs of a heart attack:
- Squeezing, pressure, or pain in your chest
- You may also have any of the following:
- Discomfort or pain in your back, neck, jaw, stomach, or arm
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or a sudden cold sweat
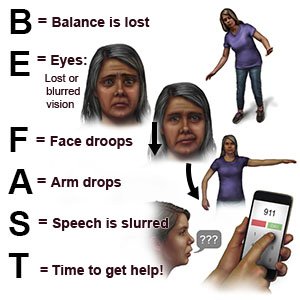
- You have any of the following signs of a stroke:
- Numbness or drooping on one side of your face
- Weakness in an arm or leg
- Confusion or difficulty speaking
- Dizziness, a severe headache, or vision loss
- You have nausea and are vomiting.
- You cough or vomit up blood.
- You cannot feel or move anything from your waist to your toes.
- You have trouble breathing or shortness of breath.
- You have sudden chest, neck, back, or abdominal pain.
- You feel dizzy, faint, or you lose consciousness.
When should I seek immediate care?
- You have a fever.
- You have blood in your urine.
- You are urinating very little or not at all.
- You have at least 1 toe that looks blue or darker than usual.
- You have new symptoms or your symptoms are worse.
- Your skin is pale, sweaty, or clammy.
When should I call my doctor or specialist?
- You want to start family planning.
- You feel anxious or depressed about your condition.
- Your symptoms prevent you from doing your daily activities.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
