Theophylline Dosage
Medically reviewed by Drugs.com. Last updated on Jul 25, 2025.
Applies to the following strengths: 100 mg; 200 mg; 400 mg/24 hours; 600 mg/24 hours; 125 mg; 300 mg; 450 mg; 80 mg/15 mL; 5%-40 mg/100 mL; 800 mcg/mL-D5%; 1.6 mg/mL-D5%; 2 mg/mL-D5%; 4 mg/mL-D5%; 3.2 mg/mL-D5%; 50 mg; 75 mg; 250 mg; 500 mg; 130 mg; 260 mg; 65 mg; 100 mg/24 hours; 200 mg/24 hours; 300 mg/24 hours
Usual Adult Dose for:
Usual Pediatric Dose for:
Additional dosage information:
Usual Adult Dose for Asthma - Maintenance
Oral Liquid:
Adults Without Risk Factors for Impaired Clearance:
Initial dose: 300 mg per day given as evenly divided doses every 6 to 8 hours
After 3 days, if starting dose was tolerated: 400 mg per day given as evenly divided doses every 6 to 8 hours
After 3 more days, if tolerated: 600 mg per day given as evenly divided doses every 6 to 8 hours
Adults With Risk Factors for Impaired Clearance, Elderly Patients Over 60 Years Old, and Those In Whom Serum Theophylline Monitoring Is Not Feasible:
Maximum dose: 400 mg per day
Extended Release Tablets (400 or 600 mg):
Stabilized patients taking immediate or controlled release theophylline: One tablet orally once a day in the morning or evening (on a mg for mg basis with the previous dose)
Comments:
- Theophylline distributes poorly into body fat; mg/kg doses should use ideal body weight for calculations.
- Steady state peak concentrations are a function of dose and dosing interval, absorption, and clearance.
- Because of differences in theophylline clearance, the dose needed to achieve a peak theophylline of 10 to 20 mcg/mL varies up to fourfold (e.g. 400 to 1600 mg orally daily for adults, 10 to 36 mg/kg/day for children).
- There is no single dose that is both safe and effective for all patients.
- Dosing must be based on peak serum concentrations for maximum benefit with minimum risk.
- Slow metabolizers may see transient caffeine-like adverse effects and excessive serum concentrations; this can be avoided in most patients by starting with a low dose and slowly increasing, if clinically indicated, by small amounts.
- High metabolizers (as evidenced by needing higher average doses) should receive smaller doses more frequently to prevent breakthrough symptoms; a reliably absorbed slow release formulation may decrease fluctuations and allow longer dosing intervals.
Use: Treatment of the symptoms and reversible airflow obstruction associated with chronic asthma and other chronic lung diseases (e.g. emphysema, chronic bronchitis)
Usual Adult Dose for Asthma - Acute
Intravenous theophylline in dextrose:
Loading dose, no theophylline in the previous 24 hours: 4.6 mg/kg ideal body weight, intravenously over 30 minutes, results in an average 10 mcg/mL (range 6 to 16) serum theophylline concentration
- Calculate dose based on this formula: Concentration = loading dose / volume of distribution
- Each mg/kg ideal body weight theophylline administered over 30 minutes increases serum theophylline approximately 2 mcg/mL (assuming volume of distribution of 0.5 L/kg)
Loading dose, theophylline received in the previous 24 hours: Dose = (desired concentration - measured concentration) (volume of distribution)
Once a serum concentration of 10 to 15 mcg/mL has been achieved, start a constant infusion
Initial infusion rate after loading dose, otherwise healthy nonsmokers: 0.4 mg/kg ideal body weight/hour
Maximum dose: 900 mg/day, unless serum levels indicate a larger dose is needed
Oral Liquid for Acute Bronchodilation:
No theophylline in the previous 24 hours: A single 5 mg/kg dose produces and average peak serum theophylline concentration of 10 mcg/mL (range 5 to 15 mcg/mL)
Comments:
- Inhaled beta-2 agonists, alone or combined with a systemic corticosteroid, are the most effective treatment for an acute exacerbations of reversible airway obstruction.
- Theophylline, a relatively weak bronchodilator, is less effective than inhaled beta-2 agonists, and does not add benefits in acute bronchospasm.
- If beta agonists are not available, an oral theophylline loading dose can be used as a temporary measure.
- Steady state peak concentrations are a function of dose and dosing interval, absorption, and clearance.
- Because of differences in theophylline clearance, the dose needed to achieve a peak theophylline of 10 to 20 mcg/mL varies up to fourfold (e.g. 400 to 1600 mg orally daily for adults, 10 to 36 mg/kg/day for children).
- There is no single dose that is both safe and effective for all patients.
- Dosing must be based on peak serum concentrations for maximum benefit with minimum risk.
- Slow metabolizers may see transient caffeine-like adverse effects and excessive serum concentrations; this can be avoided in most patients by starting with a low dose and slowly increasing, if clinically indicated, by small amounts.
Use: As an adjunct to inhaled beta-2 selective agonists and systemic corticosteroids for treatment of acute exacerbations of the symptoms and reversible airflow obstruction associated with chronic asthma and other chronic lung diseases (e.g. emphysema, chronic bronchitis)
Usual Pediatric Dose for Asthma - Maintenance
Oral Liquid:
Premature infants (under 1 year old):
Initial dose:
- Post natal age less than 24 days: 1 mg/kg every 12 hours
- Post natal age 24 days and older: 1.5 mg/kg every 12 hours
Full term infants and up to 52 weeks old:
Initial dose: Total daily dose (mg) = [(0.2 x age in weeks)+5] x (kg body weight)
- Up to 26 weeks old: Give as 3 evenly divided doses every 8 hours
- Over 26 weeks old: Give as 4 evenly divided doses every 6 hours
Children 1 year and older without risk factors for impaired clearance:
- Weight under 45 kg:
After 3 days, if starting dose was tolerated: 16 mg/kg/day (max 400 mg) given as evenly divided doses every 4 to 6 hours
After 3 more days, if tolerated: 20 mg/kg/day (max 600 mg) given as evenly divided doses every 4 to 6 hours
- Weight over 45 kg or age 16 years and older:
After 3 days, if starting dose was tolerated: 400 mg per day given as evenly divided doses every 6 to 8 hours
After 3 more days, if tolerated: 600 mg per day given as evenly divided doses every 6 to 8 hours
Extended Release Tablets (400 or 600 mg):
Children 12 and older, stabilized on an immediate- or controlled-release product: Transfer to once a day extended release product on a mg for mg basis
- Peak and trough serum levels may vary from the previous regimen
Comments:
- Steady state peak concentrations are a function of dose and dosing interval, absorption, and clearance.
- Because of differences in theophylline clearance, the dose needed to achieve a peak theophylline of 10 to 20 mcg/mL varies up to fourfold (e.g. 400 to 1600 mg orally daily for adults, 10 to 36 mg/kg/day for children).
- There is no single dose that is both safe and effective for all patients.
- Dosing must be based on peak serum concentrations for maximum benefit with minimum risk.
- Slow metabolizers may see transient caffeine-like adverse effects and excessive serum concentrations; this can be avoided in most patients by starting with a low dose and slowly increasing, if clinically indicated, by small amounts.
- High metabolizers (as evidenced by needing higher average doses) should receive smaller doses more frequently to prevent breakthrough symptoms; a reliably absorbed slow release formulation may decrease fluctuations and allow longer dosing intervals.
Use: Treatment of symptoms of reversible airflow obstruction associated with chronic asthma and other chronic lung diseases (e.g. emphysema, chronic bronchitis)
Usual Pediatric Dose for Asthma - Acute
Intravenous theophylline in dextrose:
Loading dose, no theophylline in the previous 24 hours: 4.6 mg/kg ideal body weight, intravenously over 30 minutes, results in an average 10 mcg/mL (range 6 to 16) serum theophylline concentration
- Calculate dose based on this formula: Concentration = loading dose / volume of distribution
- Each mg/kg ideal body weight theophylline administered over 30 minutes increases serum theophylline approximately 2 mcg/mL (assuming volume of distribution of 0.5 L/kg)
Loading dose, theophylline received in the previous 24 hours: Dose = (desired concentration - measured concentration) (volume of distribution)
Once a serum concentration of 10 to 15 mcg/mL has been achieved, start a constant infusion
Initial infusion rate after loading dose:
Postnatal age up to 24 days: 1 mg/kg ideal body weight/hour every 12 hours
Neonates with postnatal age over 24 days: 1.5 mg/kg ideal body weight/hour every 12 hours
6 to 52 weeks old: mg/kg/hr = (0.008)(age in weeks) + 0.21
1 to 9 years: 0.8 mg/kg ideal body weight/hour
9 to 12 years: 0.7 mg/kg ideal body weight/hour
12 to 16 years, cigarette or marijuana smoker: 0.7 mg/kg ideal body weight/hour
12 to 16 years, nonsmoker: 0.5 mg/kg ideal body weight/hour
16 years and older, otherwise healthy nonsmoker: 0.4 mg/kg ideal body weight/hour
Maximum dose: 900 mg/day, unless serum levels indicate a larger dose is needed
Oral Liquid for Acute Bronchodilation:
No theophylline in the previous 24 hours: A single 5 mg/kg dose produces and average peak serum theophylline concentration of 10 mcg/mL (range 5 to 15 mcg/mL)
Comments:
- Inhaled beta-2 agonists, alone or combined with a systemic corticosteroid, are the most effective treatment for an acute exacerbations of reversible airway obstruction.
- Theophylline, a relatively weak bronchodilator, is less effective than inhaled beta-2 agonists, and does not add benefits in acute bronchospasm.
- If beta agonists are not available, an oral theophylline loading dose can be used as a temporary measure.
- Steady state peak concentrations are a function of dose and dosing interval, absorption, and clearance.
- Because of differences in theophylline clearance, the dose needed to achieve a peak theophylline of 10 to 20 mcg/mL varies up to fourfold (e.g. 400 to 1600 mg orally daily for adults, 10 to 36 mg/kg/day for children).
- There is no single dose that is both safe and effective for all patients.
- Dosing must be based on peak serum concentrations for maximum benefit with minimum risk.
- Slow metabolizers may see transient caffeine-like adverse effects and excessive serum concentrations; this can be avoided in most patients by starting with a low dose and slowly increasing, if clinically indicated, by small amounts.
Use: As an adjunct to inhaled beta-2 selective agonists and systemic corticosteroids for treatment of acute exacerbations of the symptoms and reversible airflow obstruction associated with chronic asthma and other chronic lung diseases (e.g. emphysema, chronic bronchitis)
Renal Dose Adjustments
No adjustment recommended in patients over 3 months of age
- Little theophylline is excreted unchanged in the urine and active metabolites (caffeine, 3-methylxanthine) do not attain clinically significant levels even in end stage renal disease.
- In neonates, the large amounts (50%) of unchanged theophylline and caffeine in the urine requires careful attention to dose adjustment and frequent serum theophylline monitoring in reduced renal function.
Liver Dose Adjustments
Dose adjustment(s) may be required; however, no specific guidelines have been suggested. Caution is recommended.
- Theophylline clearance is decreased 50% or more in hepatic insufficiency (e.g. cirrhosis, acute hepatitis, cholestasis).
- Reduce dose carefully and monitor frequently.
Dose Adjustments
The manufacturer product information should be consulted for formula specific adjustments based on serum concentrations.
Adverse Events:
- Discontinue medication until symptoms resolve.
- Resume therapy at a lower, previously tolerated dose
Oral formulations:
- Only increase dose if the current dose is well tolerated.
- Increase at intervals of no less than 3 days to allow serum concentrations to return to steady state.
- Dose adjustments should be guided by serum theophylline concentrations.
Precautions
NARROW THERAPEUTIC INDEX:
- This drug should be considered a narrow therapeutic index (NTI) drug as small differences in dose or blood concentrations may lead to serious therapeutic failures or adverse drug reactions.
- Generic substitution should be done cautiously, if at all, as current bioequivalence standards are generally insufficient for NTI drugs.
- Additional and/or more frequent monitoring should be done to ensure receipt of an effective dose while avoiding unnecessary toxicities.
CONTRAINDICATIONS:
- Hypersensitivity to any of the ingredients
Consult WARNINGS section for additional precautions.
Dialysis
Data not available
Other Comments
Administration advice:
- Missed oral doses should be skipped; do not attempt to make up for the missed dose.
- Extended release tablets should be taken consistently with or without food (either always with food, or always on an empty stomach).
- Taking extended release tablets with food is recommended.
- Extended release tablets may be taken once a day, either in the morning or evening.
- Do not crush or chew extended release tablets; scored tablets may be split.
- Do not administer intravenous theophylline in dextrose simultaneously with blood in the same infusion set; agglomeration of erythrocytes may occur.
- Theophylline distributes poorly into body fat; mg/kg doses should use ideal body weight for calculations.
Reconstitution/preparation techniques:
- Do not use plastic containers in series connection.
IV compatibility:
- Do not mix additives into intravenous theophylline in dextrose
Monitoring:
- Use serum theophylline concentrations to determine if a dose is appropriate.
- Measure serum theophylline during therapy initiation to guide final dosage after titration.
- Measure serum theophylline to determine if the dose is subtherapeutic prior to dose increases in patients who remain symptomatic.
- Measure serum theophylline whenever symptoms of theophylline toxicity are present.
- Monitor serum theophylline for any new illness, worsening of preexisting illness, or changes in treatment that may affect theophylline clearance.
- Obtain samples at the expected peak; at steady state this is 12 hours after an oral evening dose or 9 hours after an oral morning dose; samples taken later than at these times should be used with caution, as they may not reflect peak concentrations.
- When administered intravenously, patients who have not had theophylline in the prior 24 hours should have theophylline concentrations measured 30 minutes after the end of the infusion; concentrations under 10 mcg/mL indicate an additional loading dose is needed; concentrations over 20 mcg/mL need to delay starting the constant infusion.
- When administered intravenously, patients who have had theophylline in the prior 24 hours should have serum concentrations drawn before giving a loading dose for safety; if no loading dose is indicated (e.g. theophylline concentrations 10 mcg/mL or higher), obtain a second measurement after one expected half-life (the manufacturer product information should be consulted) and compare to determine an appropriate infusion rate.
- Obtain serum theophylline concentrations every 24 hours when giving intravenously; adjust infusion rate based on serum theophylline levels.
- Steady state is reached after 3 days of oral dosing in most patients, assuming no missed or extra doses and doses were taken at even intervals.
- Trough concentrations are not useful and can lead to inappropriate dose increases; peak concentrations can be 2 to 3 times higher than trough.
- Obtain serum theophylline concentrations immediately for signs of toxicity.
- If decreased serum protein binding is suspected (e.g. cirrhosis, third pregnancy trimester), measure unbound theophylline concentration and adjust dose to achieve 6 to 12 mcg/mL unbound theophylline.
- Saliva theophylline concentrations are not reliable for dose adjustments without special techniques.
Patient advice:
- Patients should seek medical advice whenever nausea, vomiting, persistent headache, insomnia, or rapid heartbeat occurs, even if theophylline is not suspected.
- Patients should contact their healthcare provider for new illnesses (especially with persistent fever) or worsening of preexisting conditions, if they stop or start smoking (cigarettes or marijuana), or for new or discontinued concomitant medications.
- Patients taking St. John's Wort should consult their healthcare provider before stopping, as theophylline concentrations may increase, causing toxicity.
- Patients should let all their healthcare providers know they are on theophylline, especially when concomitant medications are started or stopped.
- Do not alter the dose, timing, or frequency of administration without consulting a healthcare provider.
- Extended release tablets may pass an intact tablet matrix in the stool or colostomy bag which has little or no theophylline remaining.
More about theophylline
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (19)
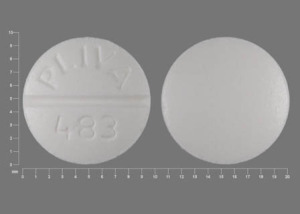
- Drug images
- Side effects
- During pregnancy
- Drug class: methylxanthines
- Breastfeeding
- En español
Patient resources
- Theophylline drug information
- Theophylline (Intravenous) (Advanced Reading)
- Theophylline (Oral) (Advanced Reading)
Other brands
Theo-Dur, Theo-24, Elixophyllin, Quibron-T/SR, ... +6 more
Professional resources
- Theophylline prescribing information
- Theophylline Elixir (FDA)
- Theophylline Oral Solution (FDA)
- Theophylline in Dextrose (FDA)
Other brands
Theo-24, Elixophyllin, Quibron-T/SR
Related treatment guides
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.