Theo-24 Dosage
Generic name: THEOPHYLLINE ANHYDROUS 100mg
Dosage form: capsule, extended release
Drug class: Methylxanthines
Medically reviewed by Drugs.com. Last updated on Jul 8, 2024.
General Considerations:
Theo-24, like other extended-release theophylline products, is intended for patients with relatively continuous or recurring symptoms who have a need to maintain therapeutic serum levels of theophylline. It is not intended for patients experiencing an acute episode of bronchospasm (associated with asthma, chronic bronchitis, or emphysema). Such patients require rapid relief of symptoms and should be treated with an immediate-release or intravenous theophylline preparation (or other bronchodilators) and not with extended-release products.
Patients who metabolize theophylline at a normal or slow rate are reasonable candidates for once-daily dosing with Theo-24. Patients who metabolize theophylline rapidly (e.g., the young, smokers, and some nonsmoking adults) and who have symptoms repeatedly at the end of a dosing interval, will require either increased doses given once a day or preferably, are likely to be better controlled by a schedule of twice-daily dosing. Those patients who require increased daily doses are more likely to experience relatively wide peak-trough differences and may be candidates for twice-a-day dosing with Theo-24.
Patients should be instructed to take this medication each morning at approximately the same time and not to exceed the prescribed dose.
Recent studies suggest that dosing of extended-release theophylline products at night (after the evening meal) results in serum concentrations of theophylline which are not identical to those recorded during waking hours and may be characterized by early trough and delayed peak levels. This appears to occur whether the drug is given as an immediate-release, extended-release, or intravenous product. To avoid this phenomenon when two doses per day are prescribed, it is recommended that the second dose be given 10 to 12 hours after the morning dose and before the evening meal.
Food and posture, along with changes associated with circadian rhythm, may influence the rate of absorption and/or clearance rates of theophylline from extended-release dosage forms administered at night. The exact relationship of these and other factors to nighttime serum concentrations and the clinical significance of such findings require additional study. Therefore, it is not recommended that Theo-24 (when used as a once-a-day product) be administered at night.
Patients who require a relatively high dose of theophylline (i.e., a dose equal to or greater than 900 mg or 13 mg/kg, whichever is less) should not take Theo-24 less than 1 hour before a high-fat-content meal since this may result in a significant increase in peak serum level and in the extent of absorption of theophylline as compared to administration in the fasted state (see PRECAUTIONS, Drug/Food Interactions).
The steady-state peak serum theophylline concentration is a function of the dose, the dosing interval, and the rate of theophylline absorption and clearance in the individual patient. Because of marked individual differences in the rate of theophylline clearance, the dose required to achieve a peak serum theophylline concentration in the 10 - 20 mcg/mL range varies fourfold among otherwise similar patients in the absence of factors known to alter theophylline clearance (e.g., 400 - 1600 mg/day in adults <60 years old and 10 - 36 mg/kg/day in children 1 - 9 years old). For a given population there is no single theophylline dose that will provide both safe and effective serum concentrations for all patients. Administration of the median theophylline dose required to achieve a therapeutic serum theophylline concentration in a given population may result in either sub-therapeutic or potentially toxic serum theophylline concentrations in individual patients. For example, at a dose of 900 mg/day in adults <60 years or 22 mg/kg/day in children 1-9 years, the steady-state peak serum theophylline concentration will be <10 mcg/mL in about 30% of patients, 10 - 20 mcg/mL in about 50% and 20 - 30 mcg/mL in about 20% of patients. The dose of theophylline must be individualized on the basis of peak serum theophylline concentration measurements in order to achieve a dose that will provide maximum potential benefit with minimal risk of adverse effects.
Transient caffeine-like adverse effects and excessive serum concentrations in slow metabolizers can be avoided in most patients by starting with a sufficiently low dose and slowly increasing the dose, if judged to be clinically indicated, in small increments (See Table V). Dose increases should only be made if the previous dosage is well tolerated and at intervals of no less than 3 days to allow serum theophylline concentrations to reach the new steady state. Dosage adjustment should be guided by serum theophylline concentration measurement (see PRECAUTIONS, Laboratory Tests and DOSAGE AND ADMINISTRATION, Table VI). Health care providers should instruct patients and care givers to discontinue any dosage that causes adverse effects, to withhold the medication until these symptoms are gone and to then resume therapy at a lower, previously tolerated dosage (see WARNINGS).
If the patient's symptoms are well controlled, there are no apparent adverse effects, and no intervening factors that might alter dosage requirements (see WARNINGS and PRECAUTIONS), serum theophylline concentrations should be monitored at 6 month intervals for rapidly growing children and at yearly intervals for all others. In acutely ill patients, serum theophylline concentrations should be monitored at frequent intervals, e.g., every 24 hours.
Theophylline distributes poorly into body fat, therefore, mg/kg dose should be calculated on the basis of ideal body weight.
Table V contains theophylline dosing titration schema recommended for patients in various age groups and clinical circumstances. Table VI contains recommendations for theophylline dosage adjustment based upon serum theophylline concentrations. Application of these general dosing recommendations to individual patients must take into account the unique clinical characteristics of each patient. In general, these recommendations should serve as the upper limit for dosage adjustments in order to decrease the risk of potentially serious adverse events associated with unexpected large increases in serum theophylline concentration.
| * Patients with more rapid metabolism, clinically identified by higher than average dose requirements, should receive a smaller dose more frequently to prevent breakthrough symptoms resulting from low trough concentrations before the next dose. A reliably absorbed slow-release formulation will decrease fluctuations and permit longer dosing intervals. |
|||
| A. | Children (12-15 years) and adults (16-60 years) without risk factors for impaired clearance. | ||
| Titration Step | Children <45 kg | Children >45 kg and adults | |
| 1. | Starting Dosage | 12 - 14 mg/kg/day up to a maximum of 300 mg/day divided Q 24 hrs* |
300 - 400 mg/day1 divided Q 24 hrs* |
| 2. | After 3 days, if tolerated, increase dose to: |
16 mg/kg/day up to a maximum of 400 mg/day divided Q 24 hrs* |
400 - 600 mg/day1 divided Q 24 hrs* |
| 3. | After 3 more days, if tolerated and if needed, increase dose to: |
20 mg/kg/day up to a maximum of 600 mg/day divided Q 24 hrs* |
As with all theophylline products, doses greater than 600 mg should be titrated according to blood level (see Table VI) |
| 1 | If caffeine-like adverse effects occur, then consideration should be given to a lower dose and titrating the dose more slowly (see ADVERSE REACTIONS). |
||
| B. | Patients with risk factors for impaired clearance, the elderly (>60 Years), and those in whom it is not feasible to monitor serum theophylline concentrations: In children 12-15 years of age, the final theophylline dose should not exceed 16 mg/kg/day up to a maximum of 400 mg/day in the presence of risk factors for reduced theophylline clearance (see WARNINGS) or if it is not feasible to monitor serum theophylline concentrations. In adolescents ≥16 years and adults, including the elderly, the final theophylline dose should not exceed 400 mg/day in the presence of risk factors for reduced theophylline clearance (see WARNINGS) or if it is not feasible to monitor serum theophylline concentrations. |
||
| Peak Serum Concentration |
Dosage Adjustment |
|---|---|
| * Dose reduction and/or serum theophylline concentration measurement is indicated whenever adverse effects are present, physiologic abnormalities that can reduce theophylline clearance occur (e.g., sustained fever), or a drug that interacts with theophylline is added or discontinued (see WARNINGS). |
|
| <9.9 mcg/mL | If symptoms are not controlled and current dosage is tolerated, increase dose about 25%. Recheck serum concentration after three days for further dosage adjustment. |
| 10 - 14.9 mcg/mL | If symptoms are controlled and current dosage is tolerated, maintain dose and recheck serum concentration at 6-12 month intervals.* If symptoms are not controlled and current dosage is tolerated consider adding additional medication(s) to treatment regimen. |
| 15 - 19.9 mcg/mL | Consider 10% decrease in dose to provide greater margin of safety even if current dosage is tolerated. * |
| 20 - 24.9 mcg/mL | Decrease dose by 25% even if no adverse effects are present. Recheck serum concentration after 3 days to guide further dosage adjustment. |
| 25 - 30 mcg/mL | Skip next dose and decrease subsequent doses at least 25% even if no adverse effects are present. Recheck serum concentration after 3 days to guide further dosage adjustment. If symptomatic, consider whether overdosage treatment is indicated (see recommendations for chronic overdosage). |
| >30 mcg/mL | Treat overdose as indicated (see recommendations for chronic overdosage). If theophylline is subsequently resumed, decrease dose by at least 50% and recheck serum concentration after 3 days to guide further dosage adjustment. |
More about Theo-24 (theophylline)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (2)
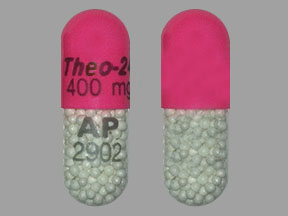
- Drug images
- Side effects
- During pregnancy
- Drug class: methylxanthines
- Breastfeeding
- En español
Patient resources
Other brands
Theo-Dur, Elixophyllin, Quibron-T/SR, Theochron, ... +5 more
Professional resources
Other brands
Related treatment guides
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.