Selpercatinib Dosage
Medically reviewed by Drugs.com. Last updated on Jul 2, 2024.
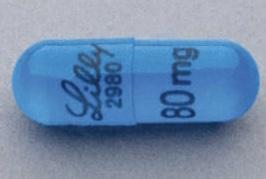
Applies to the following strengths: 80 mg; 40 mg; 160 mg; 120 mg
Usual Adult Dose for:
Usual Pediatric Dose for:
Additional dosage information:
Usual Adult Dose for Non-Small Cell Lung Cancer
Less than 50 kg: 120 mg orally twice a day
50 kg or greater: 160 mg orally twice a day
Duration of therapy: Until disease progression or unacceptable toxicity
Comments:
- Select patients for treatment based on the presence of a rearranged during transfection (RET) gene fusion or specific gene mutation in tumor specimens, as detected by an FDA-approved test.
Uses:
- For the treatment of locally advanced or metastatic non-small cell lung cancer (NSCLC) with a RET gene fusion
- For the treatment of advanced or metastatic medullary thyroid cancer (MTC) with a RET mutation requiring systemic therapy
- For the treatment of advanced or metastatic thyroid cancer with a RET gene fusion requiring systemic therapy and is radioactive iodine-refractory (if radioactive iodine is appropriate)
- For the treatment of locally advanced or metastatic solid tumors with a RET gene fusion that have progressed on or following prior systemic treatment, or have no satisfactory alternative treatment options
Usual Adult Dose for Solid Tumors
Less than 50 kg: 120 mg orally twice a day
50 kg or greater: 160 mg orally twice a day
Duration of therapy: Until disease progression or unacceptable toxicity
Comments:
- Select patients for treatment based on the presence of a rearranged during transfection (RET) gene fusion or specific gene mutation in tumor specimens, as detected by an FDA-approved test.
Uses:
- For the treatment of locally advanced or metastatic non-small cell lung cancer (NSCLC) with a RET gene fusion
- For the treatment of advanced or metastatic medullary thyroid cancer (MTC) with a RET mutation requiring systemic therapy
- For the treatment of advanced or metastatic thyroid cancer with a RET gene fusion requiring systemic therapy and is radioactive iodine-refractory (if radioactive iodine is appropriate)
- For the treatment of locally advanced or metastatic solid tumors with a RET gene fusion that have progressed on or following prior systemic treatment, or have no satisfactory alternative treatment options
Usual Adult Dose for Thyroid Cancer
Less than 50 kg: 120 mg orally twice a day
50 kg or greater: 160 mg orally twice a day
Duration of therapy: Until disease progression or unacceptable toxicity
Comments:
- Select patients for treatment based on the presence of a rearranged during transfection (RET) gene fusion or specific gene mutation in tumor specimens, as detected by an FDA-approved test.
Uses:
- For the treatment of locally advanced or metastatic non-small cell lung cancer (NSCLC) with a RET gene fusion
- For the treatment of advanced or metastatic medullary thyroid cancer (MTC) with a RET mutation requiring systemic therapy
- For the treatment of advanced or metastatic thyroid cancer with a RET gene fusion requiring systemic therapy and is radioactive iodine-refractory (if radioactive iodine is appropriate)
- For the treatment of locally advanced or metastatic solid tumors with a RET gene fusion that have progressed on or following prior systemic treatment, or have no satisfactory alternative treatment options
Usual Pediatric Dose for Solid Tumors
2 to less than 12 years:
- BSA 0.33 to 0.65 m2: 40 mg orally 3 times a day
- BSA 0.66 to 1.08 m2: 80 mg orally twice a day
- BSA 1.09 to 1.52 m2: 120 mg orally twice a day
- BSA 1.53 m2 or greater: 160 mg orally twice a day
12 years and older:
- Less than 50 kg: 120 mg orally twice a day
- 50 kg or greater: 160 mg orally twice a day
Comments:
- It is not recommended to dose pediatric patients with BSA less than 0.33 m2.
- Duration of therapy: Until disease progression or unacceptable toxicity.
- Select patients for treatment based on the presence of a RET gene fusion or specific gene mutation in tumor specimens, as detected by an FDA-approved test.
Uses:
- For the treatment of advanced or metastatic MTC with a RET mutation requiring systemic therapy
- For the treatment of advanced or metastatic thyroid cancer with a RET gene fusion requiring systemic therapy and is radioactive iodine-refractory (if radioactive iodine is appropriate)
- For the treatment of locally advanced or metastatic solid tumors with a RET gene fusion that have progressed on or following prior systemic treatment, or have no satisfactory alternative treatment options
Usual Pediatric Dose for Thyroid Cancer
2 to less than 12 years:
- BSA 0.33 to 0.65 m2: 40 mg orally 3 times a day
- BSA 0.66 to 1.08 m2: 80 mg orally twice a day
- BSA 1.09 to 1.52 m2: 120 mg orally twice a day
- BSA 1.53 m2 or greater: 160 mg orally twice a day
12 years and older:
- Less than 50 kg: 120 mg orally twice a day
- 50 kg or greater: 160 mg orally twice a day
Comments:
- It is not recommended to dose pediatric patients with BSA less than 0.33 m2.
- Duration of therapy: Until disease progression or unacceptable toxicity.
- Select patients for treatment based on the presence of a RET gene fusion or specific gene mutation in tumor specimens, as detected by an FDA-approved test.
Uses:
- For the treatment of advanced or metastatic MTC with a RET mutation requiring systemic therapy
- For the treatment of advanced or metastatic thyroid cancer with a RET gene fusion requiring systemic therapy and is radioactive iodine-refractory (if radioactive iodine is appropriate)
- For the treatment of locally advanced or metastatic solid tumors with a RET gene fusion that have progressed on or following prior systemic treatment, or have no satisfactory alternative treatment options
Renal Dose Adjustments
Mild, moderate, or severe renal dysfunction (estimated GFR 15 to 89 mL/min): No dose adjustment recommended
End-stage renal disease (estimated GFR less than 15 mL/min): Data not available
Liver Dose Adjustments
LIVER DYSFUNCTION:
- Mild Liver Dysfunction (total bilirubin at the upper limit of normal [1 x ULN] or less with AST greater than 1 x ULN, or total bilirubin greater than 1 to 1.5 x ULN with any AST): No dose adjustment recommended
- Moderate Liver Dysfunction (total bilirubin greater than 1.5 to 3 x ULN and any AST): No dose adjustment recommended
- Severe Liver Dysfunction (total bilirubin greater than 3 to 10 x ULN): Dose reduction as follows:
- Current dose - 40 mg 3 times a day: Reduce to 40 mg orally twice a day
- Current dose - 80 mg twice a day: Reduce to 40 mg orally twice a day
- Current dose - 120 mg twice a day: Reduce to 80 mg orally twice a day
- Current dose - 160 mg twice a day: Reduce to 80 mg orally twice a day
HEPATOTOXICITY (Grade 3 or 4):
- Withhold therapy and monitor AST/ALT once weekly until resolution to grade 1 or baseline.
- Resume therapy at a dose reduced by 2 dosing levels and monitor AST and ALT once weekly until 4 weeks after reaching the dose taken prior to onset of reaction.
- Increase dose by 1 dose level after a minimum of 2 weeks without reaction recurrence and then increase to dose taken prior to onset of reaction after a minimum of 4 weeks without recurrence.
Dose Adjustments
DOSE REDUCTION REGIMEN FOR ADVERSE REACTIONS:
Current Dose - 40 mg 3 times a day:
- First dose reduction: 40 mg orally twice a day
- Second dose reduction: 40 mg orally once a day
- Third dose reduction: Permanently discontinue therapy
Current Dose - 80 mg twice a day:
- First dose reduction: 40 mg orally twice a day
- Second dose reduction: 40 mg orally once a day
- Third dose reduction: Permanently discontinue therapy
Current Dose - 120 mg twice a day:
- First dose reduction: 80 mg orally twice a day
- Second dose reduction: 40 mg orally twice a day
- Third dose reduction: 40 mg orally once a day
- Fourth dose reduction: Permanently discontinue therapy
Current Dose - 160 mg twice a day:
- First dose reduction: 120 mg orally twice a day
- Second dose reduction: 80 mg orally twice a day
- Third dose reduction: 40 mg orally twice a day
- Fourth dose reduction: Permanently discontinue therapy
DOSAGE MODIFICATIONS FOR ADVERSE REACTIONS:
Interstitial Lung Disease (ILD)/Pneumonitis:
- Grade 2: Withhold until resolution; then, resume at a reduced dose. Discontinue for recurrence.
- Grade 3 or 4: Discontinue for confirmed ILD/pneumonitis.
Hypertension:
- Grade 3: Withhold for grade 3 hypertension that persists despite optimal antihypertensive therapy. Resume at a reduced dose when hypertension is controlled.
- Grade 4: Discontinue therapy.
QT Interval Prolongation:
- Grade 3: Withhold until recovery to baseline, or grade 1 or 0; then, resume at a reduced dose or permanently discontinue therapy.
- Grade 4: Discontinue therapy
Hemorrhagic Events:
- Grade 3 or 4: Withhold until recovery to baseline, or grade 1 or 0; discontinue therapy for severe or life-threatening events.
Hypersensitivity (all grades):
- Withhold until resolution of event; initiate corticosteroids.
- Resume at a dose reduced by 3 dosing levels while continuing corticosteroids. Increase by 1 dosing level each week until reaching dose taken prior to onset of reaction, then taper corticosteroids.
Hypothyroidism:
- Grade 3 or 4: Withhold until resolution to grade 1 or baseline. Discontinue therapy based on severity.
Other Adverse Reactions:
- Grade 3 or 4: Withhold until recovery to baseline, or grade 0 or 1; then, resume at a reduced dose.
CONCOMITANT USE OF STRONG AND MODERATE CYP450 3A INDUCERS: Avoid coadministration.
CONCOMITANT USE OF STRONG AND MODERATE CYP450 3A INHIBITORS: Avoid coadministration. If concomitant use cannot be avoided, reduce the dose of this drug. After inhibitor has been discontinued for 3 to 5 half-lives, resume therapy at the dose taken prior to initiating the CYP450 3A inhibitor.
Current Dose - 40 mg 3 times a day:
- Moderate CYP450 3A inhibitor: Reduce dose to 40 mg orally once a day
- Strong CYP450 3A inhibitor: Reduce dose to 40 mg orally once a day
Current Dose - 80 mg twice a day:
- Moderate CYP450 3A inhibitor: Reduce dose to 40 mg orally twice a day
- Strong CYP450 3A inhibitor: Reduce dose to 40 mg orally twice a day
Current Dose - 120 mg twice a day:
- Moderate CYP450 3A inhibitor: Reduce dose to 80 mg orally twice a day
- Strong CYP450 3A inhibitor: Reduce dose to 40 mg orally twice a day
Current Dose - 160 mg twice a day:
- Moderate CYP450 3A inhibitor: Reduce dose to 120 mg orally twice a day
- Strong CYP450 3A inhibitor: Reduce dose to 80 mg orally twice a day
Precautions
CONTRAINDICATIONS: None
Safety and efficacy have not been established in patients younger than 18 years (for NSCLC), or in patients young than 2 years (for MTC, thyroid cancer, or solid tumors).
Consult WARNINGS section for additional precautions.
Dialysis
Data not available
Other Comments
Administration advice:
- For oral use
- Administer this drug with or without food.
- Swallow capsules or tablets whole; do not crush or chew.
- This drug should not be given to pediatric patients who are unable to swallow a capsule.
- If concomitant use with a proton-pump inhibitors (PPI), histamine-2 (H2) receptor antagonist, or antacid cannot be avoided, then administer as follows:
- Use with PPI: Take this drug with food.
- Use with H2-receptor antagonist: Take this drug 2 hours before or 10 hours after H2-receptor antagonist.
- Use with locally acting antacid: Take this drug 2 hours before or 2 hours after antacid administration.
- If vomiting occurs after administration, do not administer an additional dose; continue to the next scheduled dosing time.
- Do not take a missed dose unless it is more than 6 hours until the next scheduled dose.
Storage requirements:
- Store at 20C to 25C (68F to 77F); excursions between 15C and 30C (59F to 86F) are permitted.
General:
- Select patients for treatment based on the presence of a RET gene fusion (NSCLC, thyroid cancer, or other solid tumors) or specific RET gene mutation (MTC) in tumor specimens.
- Information on FDA-approved test(s) for the detection of RET gene fusions/mutations is available at: http://www.fda.gov/CompanionDiagnostics; an FDA-approved diagnostic test for plasma is not available.
- Ensure electrolyte disturbances are corrected prior to (or during) therapy.
- Do not initiate treatment in patients with uncontrolled hypertension.
Monitoring:
- Cardiovascular: QT interval (at baseline and periodically during therapy, or more frequently with risk factors or concomitant use of CYP450 3A inhibitors); blood pressure (after 1 week, at least monthly during therapy, and as clinically indicated); for QTc prolongation, especially in at-risk patients (during therapy)
- Endocrine: Thyroid function (at baseline and periodically during therapy)
- Hepatic: AST and ALT (at baseline, every 2 weeks during the first 3 months, then monthly during therapy or as clinically indicated)
- Metabolic: Electrolytes (at baseline and periodically during therapy); for signs/symptoms of tumor lysis syndrome in at-risk patients (during therapy)
- Musculoskeletal: For abnormalities in open growth plates (pediatric patients during therapy)
- Respiratory: For pulmonary symptoms indicative of ILD/pneumonitis (during therapy)
Patient advice:
- Read the US FDA-approved patient labeling (Patient Information).
- Contact your health care provider for signs/symptoms of: QTc interval prolongation (syncope), bleeding, hepatotoxicity, increased blood pressure, new or worsening cough or shortness of breath, tumor lysis syndrome, impaired wound healing, hypothyroidism, or epiphysiolysis.
- Monitor for signs and symptoms of hypersensitivity reactions, especially during the first month of therapy.
- Female patients (and males with female partners) of childbearing potential: This drug may harm a developing fetus. Inform your health care provider of a known or suspected pregnancy.
- Use effective contraception during therapy and for 1 week after the last dose.
- Breastfeeding is not recommended during treatment and for 1 week after the last dose.
More about selpercatinib
- Check interactions
- Compare alternatives
- Reviews (5)
- Side effects
- During pregnancy
- Drug class: multikinase inhibitors
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.