Chlorpromazine Dosage
Medically reviewed by Drugs.com. Last updated on Jul 24, 2023.
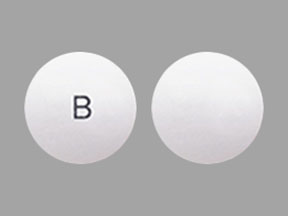
Applies to the following strengths: 30 mg/mL; 100 mg/mL; 25 mg/mL; 30 mg; 75 mg; 150 mg; 25 mg; 100 mg; 10 mg/5 mL; 10 mg; 50 mg; 200 mg
Usual Adult Dose for:
Usual Pediatric Dose for:
Additional dosage information:
Usual Adult Dose for Mania
HOSPITALIZED PATIENTS:
Acute Schizophrenia/Manic States:
Oral: 500 mg orally per day
- Maximum dose: 2000 mg/day
Parenteral: 25 mg IM once, with a subsequent 25 to 50 mg injection in 1 hour if necessary
- Maintenance dose: 400 mg IM every 4 to 6 hours until the patient is controlled
Prompt Control of Severe Symptoms:
Parenteral: 25 mg IV once, repeated in 1 hour if necessary
Oral: After an initial IM dose, 25 to 50 mg orally 3 times a day
Less Acutely Disturbed:
Oral:
- Initial dose: 25 mg orally 3 times a day
- Maintenance dose: 400 mg orally per day
OUTPATIENTS:
Oral: 10 mg orally 3 to 4 times a day OR 25 mg orally 2 to 3 times a day
More Severe Cases:
Oral: 25 mg orally 3 times a day, increasing by 20 to 50 mg at semiweekly intervals until the patient is calm and cooperative
Comments:
- Patients have experienced little therapeutic gain with doses over 1000 mg/day given for extended periods.
- Patients usually become quiet and cooperative within 24 and 48 hours.
- The dosage should be increased gradually until symptom improvement occurs; this dose should be continued for 2 weeks, and then gradually reduced to the lowest effective dose.
- Maximum improvement with oral formulations may take weeks to months.
Uses:
- Management of manifestations of psychotic disorders
- Treatment of schizophrenia
- To control the manifestations of the manic type of manic-depressive illness
Usual Adult Dose for Psychosis
HOSPITALIZED PATIENTS:
Acute Schizophrenia/Manic States:
Oral: 500 mg orally per day
- Maximum dose: 2000 mg/day
Parenteral: 25 mg IM once, with a subsequent 25 to 50 mg injection in 1 hour if necessary
- Maintenance dose: 400 mg IM every 4 to 6 hours until the patient is controlled
Prompt Control of Severe Symptoms:
Parenteral: 25 mg IV once, repeated in 1 hour if necessary
Oral: After an initial IM dose, 25 to 50 mg orally 3 times a day
Less Acutely Disturbed:
Oral:
- Initial dose: 25 mg orally 3 times a day
- Maintenance dose: 400 mg orally per day
OUTPATIENTS:
Oral: 10 mg orally 3 to 4 times a day OR 25 mg orally 2 to 3 times a day
More Severe Cases:
Oral: 25 mg orally 3 times a day, increasing by 20 to 50 mg at semiweekly intervals until the patient is calm and cooperative
Comments:
- Patients have experienced little therapeutic gain with doses over 1000 mg/day given for extended periods.
- Patients usually become quiet and cooperative within 24 and 48 hours.
- The dosage should be increased gradually until symptom improvement occurs; this dose should be continued for 2 weeks, and then gradually reduced to the lowest effective dose.
- Maximum improvement with oral formulations may take weeks to months.
Uses:
- Management of manifestations of psychotic disorders
- Treatment of schizophrenia
- To control the manifestations of the manic type of manic-depressive illness
Usual Adult Dose for Schizophrenia
HOSPITALIZED PATIENTS:
Acute Schizophrenia/Manic States:
Oral: 500 mg orally per day
- Maximum dose: 2000 mg/day
Parenteral: 25 mg IM once, with a subsequent 25 to 50 mg injection in 1 hour if necessary
- Maintenance dose: 400 mg IM every 4 to 6 hours until the patient is controlled
Prompt Control of Severe Symptoms:
Parenteral: 25 mg IV once, repeated in 1 hour if necessary
Oral: After an initial IM dose, 25 to 50 mg orally 3 times a day
Less Acutely Disturbed:
Oral:
- Initial dose: 25 mg orally 3 times a day
- Maintenance dose: 400 mg orally per day
OUTPATIENTS:
Oral: 10 mg orally 3 to 4 times a day OR 25 mg orally 2 to 3 times a day
More Severe Cases:
Oral: 25 mg orally 3 times a day, increasing by 20 to 50 mg at semiweekly intervals until the patient is calm and cooperative
Comments:
- Patients have experienced little therapeutic gain with doses over 1000 mg/day given for extended periods.
- Patients usually become quiet and cooperative within 24 and 48 hours.
- The dosage should be increased gradually until symptom improvement occurs; this dose should be continued for 2 weeks, and then gradually reduced to the lowest effective dose.
- Maximum improvement with oral formulations may take weeks to months.
Uses:
- Management of manifestations of psychotic disorders
- Treatment of schizophrenia
- To control the manifestations of the manic type of manic-depressive illness
Usual Adult Dose for Nausea/Vomiting
Oral: 10 to 25 mg orally every 4 to 6 hours as needed for nausea/vomiting
Parenteral: 25 mg IM once.
- If hypotension does not occur, give 25 to 50 mg IM every 3 to 4 hours as needed until vomiting stops, and then patients should be switched to oral formulations.
Nausea/Vomiting During Surgery:
IM: 12.5 mg IM, repeated in 30 minutes as needed AND in the absence of hypotension
IV: 2 mg IV every 2 minutes, diluted to 1 mg/mL
- Maximum IV dose: 25 mg
Comment: The frequency of dosing in the oral formulations may be increased if necessary.
Use: To control nausea and vomiting
Usual Adult Dose for Light Sedation
Oral: 25 to 50 mg orally 2 to 3 hours before the operation
Parenteral: 12.5 to 25 mg IM 1 to 2 hours before the operation
Use: Relief of restlessness and apprehension before surgery
Usual Adult Dose for Hiccups
Oral: 25 to 50 mg orally 3 to 4 times a day
Parenteral:
- Symptoms persist after 2 to 3 days with oral therapy: 25 to 50 mg IM once
- Symptoms that persist after IM administration: 25 to 50 mg slow IV infusion in 500 to 1000 mL of saline
Comments:
- If symptoms persist after 2 to 3 days with oral formulations, parenteral therapy should be started.
- Slow IV infusions should be administered to patients who are lying flat in bed, and blood pressure should be monitored closely.
Use: For relief of intractable hiccups
Usual Adult Dose for Porphyria
Oral: 25 to 50 mg orally 3 to 4 times a day
Parenteral: 25 mg IM 3 to 4 times a day, continued until the patient is able to take oral formulations
Comments:
- Patients usually may discontinue treatment after several weeks; however, some may require maintenance therapy.
- Parenteral formulations: Patients should lay down prior to and at least 30 minutes after administration.
Use: Acute intermittent porphyria
Usual Adult Dose for Tetanus
Parenteral:
IM: 25 to 50 mg IM 3 to 4 times a day, usually with barbiturates
IV: 25 to 50 mg IV, diluted to at least 1 mg/mL and given at a rate of 1 mg/min
Comments:
- Patients should be started on low IM doses; subsequent dosing and frequency should be determined by patient response.
- IM doses should be given slowly.
- Patients should lay down prior to and at least 30 minutes after administration.
Use: Adjunct to the treatment of tetanus
Usual Pediatric Dose for Aggressive Behavior
6 months to 12 years:
INPATIENTS:
Severe Behavior Disorders: 50 to 100 mg/day orally or IM (younger patients); at least 200 mg/day orally or IM (older patients)
- Maximum IM dose: 40 mg/day (up to 5 years OR 22.7 kg); 75 mg/day (5 to 12 years OR 22.7 to 45.5 kg)
OUTPATIENTS:
Oral: 0.55 mg/kg orally every 4 to 6 hours as needed
Parenteral: 0.55 mg/kg IM every 6 to 8 hours as needed
Comments:
- Route of administration should be determined by the condition of the patient.
- Patients with mental disabilities who are disturbed have experienced little therapeutic gain with doses over 500 mg/day.
Uses:
- Treatment of severe behavioral problems marked by combativeness and/or explosive hyperexcitable behavior (out of proportion to immediate provocation)
- Short-term treatment of hyperactive children with excessive motor activity and accompanying conduct disorders marked by impulsivity, difficulty sustaining attention, aggressiveness, mood lability, and/or poor frustration tolerance
Usual Pediatric Dose for Nausea/Vomiting
Oral: 0.55 mg/kg orally every 4 to 6 hours as needed
Parenteral: 0.55 mg/kg IM every 6 to 8 hours as needed
- Maximum dose: 40 mg/day (up to 22.7 kg); 75 mg/day (22.7 to 45.5 kg)
Nausea/Vomiting During Surgery:
IM: 0.275 mg/kg IM, repeated in 30 minutes as needed AND in the absence of hypotension
IV: 1 mg IV every 2 minutes, diluted to 1 mg/mL
- Maximum dose: 40 mg/day (up to 22.7 kg); 75 mg/day (22.7 to 45.5 kg)
Comment: The duration of action for parenteral doses may last up to 12 hours.
Use: To control nausea and vomiting
Usual Pediatric Dose for Light Sedation
Oral: 0.55 mg/kg orally 2 to 3 hours before the operation
Parenteral: 0.55 mg/kg IM 1 to 2 hours before the operation
Use: Relief of restlessness and apprehension before surgery
Usual Pediatric Dose for Tetanus
6 months to 12 years:
Parenteral:
IM: 0.55 mg/kg IM every 6 to 8 hours
- Maximum dose: 40 mg/day (up to 22.7 kg); 75 mg/day (22.7 to 45.5 kg)
IV: 0.55 mg/kg IV, diluted to at least 1 mg/mL and given at a rate of 0.5 mg/min
- Maximum dose: 40 mg/day (up to 22.7 kg); 75 mg/day (22.7 to 45.5 kg)
Comments:
- Patients should be started on low IM doses; subsequent dosing and frequency should be determined by patient response.
- Patients weighing 22.7 to 45.5 kg should not exceed 75 mg/day except in severe cases.
- Patients should lay down prior to and at least 30 minutes after administration.
Use: Adjunct to the treatment of tetanus
Renal Dose Adjustments
Use with caution.
Liver Dose Adjustments
Use with caution.
Dose Adjustments
Parenteral administration: This route should be limited to bedfast patients and/or acute ambulatory situations.
Excessive drowsiness: Patients may decrease the dose if drowsiness is troublesome and/or persists after 2 weeks of initiation.
Patients who are elderly, emaciated, and/or debilitated: Dosing should be lower in the treatment of mania, psychosis, and/or schizophrenia.
Precautions
US BOXED WARNINGS:
INCREASED MORTALITY IN ELDERLY PATIENTS WITH DEMENTIA-RELATED PSYCHOSIS:
- Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Analyses of 17 placebo-controlled trials (modal duration of 10 weeks), largely in patients taking atypical antipsychotic drugs, revealed a risk of death in drug-treated patients of between 1.6 to 1.7 times the risk of death in placebo-treated patients. Over the course of a typical 10-week controlled trial, the rate of death in drug-treated patients was about 4.5%, compared to a rate of about 2.6% in the placebo group.
- Although the causes of death were varied, most of the deaths appeared to be either cardiovascular (e.g., heart failure, sudden death) or infectious (e.g., pneumonia) in nature.
- Observational studies suggest that, similar to atypical antipsychotic drugs, treatment with conventional antipsychotic drugs may increase mortality. The extent to which the findings of increased mortality in observational studies may be attributed to the antipsychotic drug as opposed to some characteristic(s) of the patients is not clear.
- This drug is not approved for the treatment of patients with dementia-related psychosis.
Safety and efficacy have not been established in patients younger than 6 months.
Consult WARNINGS section for additional precautions.
Dialysis
Data not available
Other Comments
Administration advice:
- IM doses should be given deep into the upper outer quadrant of the buttock and/or into the deltoid. If patients require multiple IM doses, injection sites should be rotated to avoid irritation.
- IV formulations should be diluted before administration. Patients who develop irritation with IM formulations may benefit from dilution of the drug with saline or the addition of 2% procaine.
- Tablets should not be crushed.
Storage requirements:
- See manufacturer product information.
Reconstitution/preparation techniques:
- See manufacturer product information.
IV compatibility:
- See manufacturer product information.
General:
- All patients on prolonged treatment should be reassessed regularly to determine whether the dosage could be lowered or treatment discontinued.
- Patients receiving long-term treatment may have a higher risk of developing liver damage, corneal/lenticular deposits, and/or irreversible dyskinesia.
- Treatment has not been effective for the management of behavioral complications in patients with mental impairments.
- Oral syrup formulations are recommended for patients who refuse to take or have difficulty swallowing tablets.
- Healthcare providers administering parenteral formulations should consider using rubber gloves to decrease the risk of developing contact dermatitis.
Monitoring:
- ECG and heart rate monitoring for patients at risk of QT prolongation (e.g., arrhythmias, concurrent QT prolonging drug use)
- Periodic WBC with differential tests, especially in patients with signs/symptoms of infection/sore throat, at increased risk of blood dyscrasias, and/or with a history of low WBCs or drug-induced neutropenia/leukopenia
- Periodic liver function tests, especially in patients with liver dysfunction
- Blood pressure, especially in patients with impaired cardiovascular systems and pediatric patients
- Eye examinations, especially in patients on prolonged treatment
- Blood glucose levels in patients with diabetes mellitus
- Periodic renal function tests, especially in patients on prolonged treatment
- Yearly learning capacity examinations in pediatric patients
- Body temperature measurements, especially in patients at risk of hypothermia
Patient advice:
- Patients should be warned to avoid abrupt discontinuation of this drug.
- Patients should be instructed to immediately report any signs/symptoms of neutropenia/leukopenia, liver toxicity, neuroleptic malignant syndrome, or tardive dyskinesia.
- Inform patients that this drug may cause or impair mental/physical abilities, and they should avoid driving or operating machinery until the full effects of the drug are seen.
- Patients should be advised to speak to a healthcare provider if they are pregnant, intend to become pregnant, or are breastfeeding.
Frequently asked questions
More about chlorpromazine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (70)
- Drug images
- Side effects
- During pregnancy
- Drug class: phenothiazine antiemetics
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
- ChlorproMAZINE monograph
- Chlorpromazine (FDA)
- Chlorpromazine Oral Concentrate (FDA)
- Chlorpromazine Tablets (FDA)
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.