Zolmitriptan Disease Interactions
There are 4 disease interactions with zolmitriptan.
5-HT1 agonists (applies to zolmitriptan) CAD risk factors
Major Potential Hazard, High plausibility. Applicable conditions: Diabetes Mellitus, History (Familial) - Ischemic Heart Disease, Hyperlipidemia, Menopausal Disorder, Obesity, Smoking
The group of drugs known as 5-hydroxytryptamine1 receptor (5-HT1) agonists can cause vasospastic reactions, including coronary vasospasm, peripheral vascular ischemia, and colonic ischemia. Rarely, serious adverse cardiac events including acute myocardial infarction, arrhythmia, cardiac arrest, and death have been reported within a few hours following the administration of 5-HT1 agonists, in some cases even in patients with no prior history or findings of coronary artery disease (CAD). Significant elevation in blood pressure, including hypertensive crisis, has also been reported on rare occasions in patients with and without a history of hypertension, as have transient increases in blood pressure and peripheral vascular resistance. In general, patients with potentially unrecognized CAD as predicted by the presence of risk factors (e.g., hypertension, hypercholesterolemia, tobacco use, obesity, diabetes, strong family history of CAD, female with surgical or physiological menopause, or male over 40 years of age) should not be administered 5-HT1 agonists unless a cardiovascular evaluation provides satisfactory clinical evidence indicating the lack of CAD, ischemic heart disease, or other significant underlying cardiovascular disease. As a precaution, the manufacturers recommend that the first dose be administered under medical surveillance in such patients, and that electrocardiographic monitoring be considered during the interval immediately following administration to help detect any asymptomatic cardiac ischemia that may occur. Periodic cardiovascular evaluations should be performed during intermittent, long-term use.
5-HT1 agonists (applies to zolmitriptan) cardiovascular disease
Major Potential Hazard, High plausibility. Applicable conditions: History - Myocardial Infarction, Cerebral Vascular Disorder, History - Cerebrovascular Disease, Heart Disease, Angina Pectoris, Prinzmetal's Angina, Ischemic Heart Disease
The use of 5-hydroxytryptamine receptor (5-HT1) agonists is contraindicated in patients with a history or current symptoms or signs of ischemic coronary artery disease (CAD), coronary artery vasospasm (including Prinzmetal's angina), cerebrovascular syndromes (stroke or TIA), peripheral vascular disease (including ischemic bowel disease), uncontrolled hypertension, and any other significant underlying cardiovascular disease. 5-HT1 agonists can cause vasospastic reactions, including coronary vasospasm, peripheral vascular ischemia, and colonic ischemia. Some serious adverse cardiac events including acute myocardial infarction, arrhythmia, cardiac arrest, and death have been reported within a few hours following the administration of 5-HT1 agonists, in some cases even in patients with no prior history or findings of CAD. Significant elevation in blood pressure, including hypertensive crisis, has also been reported on rare occasions in patients with and without a history of hypertension, as have transient increases in blood pressure and peripheral vascular resistance. Cerebrovascular events have included cerebral hemorrhage, subarachnoid hemorrhage, and stroke, some resulting in fatalities. However, the relationship to 5-HT1 agonists is uncertain and, in a number of cases, the cerebrovascular events may have been primary where symptoms were mistaken to be migraine.
Zolmitriptan (applies to zolmitriptan) liver disease
Major Potential Hazard, High plausibility.
Zolmitriptan is primarily metabolized by the liver. Following oral administration in patients with severe hepatic impairment, plasma concentrations of zolmitriptan were significantly increased (up to several-fold) compared to healthy controls. Some patients experienced 20 to 80 mm Hg elevations in systolic and/or diastolic blood pressure after a 10 mg dose, presumably due to drug accumulation. Therapy with zolmitriptan should be administered cautiously in patients with impaired hepatic function. Lower dosages, no more than 2.5 mg, as well as blood pressure monitoring should be considered in patients with moderate or severe hepatic impairment.
Zolmitriptan (applies to zolmitriptan) renal dysfunction
Moderate Potential Hazard, High plausibility.
Zolmitriptan is excreted in the urine primarily as metabolites but also as unchanged drug. Following oral administration in patients with renal impairment, the clearance of zolmitriptan was not significantly altered in patients with moderate impairment (CrCl = 26 to 50 mL/min) but was reduced by 25% in patients with severe impairment (CrCl = 5 to 25 mL/min) compared to healthy controls. Therapy with rizatriptan should be administered cautiously in patients with significantly impaired renal function. A lower initial dosage may be appropriate.
Switch to professional interaction data
Zolmitriptan drug interactions
There are 160 drug interactions with zolmitriptan.
Zolmitriptan alcohol/food interactions
There are 3 alcohol/food interactions with zolmitriptan.
More about zolmitriptan
- zolmitriptan consumer information
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (164)
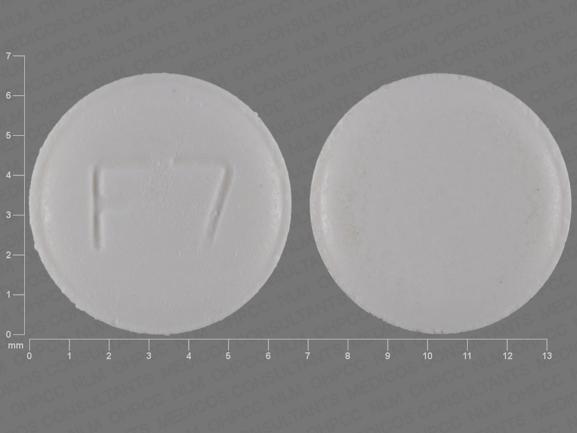
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: antimigraine agents
- Breastfeeding
Related treatment guides
Drug Interaction Classification
| Highly clinically significant. Avoid combinations; the risk of the interaction outweighs the benefit. | |
| Moderately clinically significant. Usually avoid combinations; use it only under special circumstances. | |
| Minimally clinically significant. Minimize risk; assess risk and consider an alternative drug, take steps to circumvent the interaction risk and/or institute a monitoring plan. | |
| No interaction information available. |
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.