Neomycin Disease Interactions
There are 7 disease interactions with neomycin.
- Dehydration
- Neuromuscular disorders
- Ototoxicity
- Renal dysfunction
- Intestinal obstruction
- Colitis
- GI inflammation
Aminoglycosides (applies to neomycin) dehydration
Major Potential Hazard, High plausibility. Applicable conditions: Diarrhea, Vomiting
Adequate hydration is crucial to minimize the risk of oto- and nephrotoxicity associated with the use of aminoglycosides. Dehydration should preferably be corrected prior to initiation of therapy. In patients who may be at risk for dehydration, such as those with severe and/or prolonged diarrhea or vomiting, fluid status should be monitored closely. If signs of renal irritation develop during therapy, hydration should be increased as indicated, accompanied by a reduction in dosage if necessary. Therapy should be withdrawn if urinary output decreases progressively or azotemia increases.
Aminoglycosides (applies to neomycin) neuromuscular disorders
Major Potential Hazard, Moderate plausibility. Applicable conditions: Botulism, Hypocalcemia, Myoneural Disorder, Parkinsonism
Therapy with aminoglycosides should be administered cautiously in patients with neuromuscular disorders (e.g., myasthenia gravis, parkinsonian syndrome, botulism) or hypocalcemia. Aminoglycosides can aggravate muscle weakness because of their potential curare-like effects on the neuromuscular junction, and may cause neuromuscular blockade, respiratory failure, and prolonged respiratory paralysis on these patients. Aminoglycoside- induced neuromuscular blockade is generally self-limiting, it may rarely result in respiratory paralysis. Neomycin is thought to be the most potent neuromuscular blocking agent in the class. However, the risk is greatest with intraperitoneal or intrapleural instillation of large doses or rapid intravenous administration of parenteral aminoglycosides. If signs of respiratory paralysis occur during aminoglycoside therapy, the drug should be discontinued and mechanical respiratory assistance provided if necessary.
Aminoglycosides (applies to neomycin) ototoxicity
Major Potential Hazard, High plausibility. Applicable conditions: Hearing Loss, Tinnitus
Aminoglycosides can cause eighth cranial nerve damage, resulting in vestibular and/or auditory toxicities. Symptoms include dizziness, nystagmus, vertigo, ataxia, tinnitus, and varying degrees of hearing impairment. Permanent hearing loss may occur, including, rarely, total or partial irreversible bilateral deafness after the drug has been discontinued. Therapy with aminoglycosides, particularly if prolonged (> 10 days), should be administered cautiously in patients with preexisting vestibular and/or auditory impairment, since it may delay the recognition or confound the diagnosis of a drug-induced ototoxic effect. To minimize the risk of toxicity, patients should be adequately hydrated, the usual aminoglycoside dosage should not be exceeded, use with other ototoxic agents should be avoided, and peak and trough serum aminoglycoside concentrations should be periodically determined and dosage adjusted to maintain desired levels. Serial audiograms should be obtained in patients old enough to be tested, since loss of high- frequency perception usually precedes clinical hearing loss. The dosage should be reduced or therapy withdrawn promptly if signs and symptoms of toxicity develop.
Aminoglycosides (applies to neomycin) renal dysfunction
Major Potential Hazard, High plausibility.
Aminoglycosides are potentially oto- and nephrotoxic. Eighth cranial nerve damage may manifest as vestibular and/or auditory toxicities, including dizziness, nystagmus, vertigo, ataxia, tinnitus, and varying degrees of hearing impairment. Nephrotoxicity is usually evidenced by tubular necrosis; increases in BUN, nonprotein nitrogen, and serum creatinine concentration; decreases in urine specific gravity and creatinine clearance; proteinuria; and cells or casts in the urine. Rarely, renal electrolyte wasting may occur, resulting in hypocalcemia, hypomagnesemia, and hypokalemia that may be associated with paresthesia, tetany, confusion, and positive Chvostek and Trousseau signs. Although aminoglycoside- induced nephrotoxicity is generally reversible following discontinuation of the drug, death from uremia has occurred rarely. Therapy with aminoglycosides should be administered cautiously at reduced dosages in patients with renal impairment, since they may be at increased risk for oto- and nephrotoxicity due to drug accumulation. To minimize the risk of toxicity, patients should be adequately hydrated, the usual aminoglycoside dosage should not be exceeded, use with other neuro- and nephrotoxic agents should be avoided, and peak and trough serum aminoglycoside concentrations should be periodically determined and dosage adjusted to maintain desired levels. Renal and eighth cranial nerve function should be closely monitored, and the dosage reduced or therapy withdrawn if toxicity develops.
Aminoglycosides (oral) (applies to neomycin) intestinal obstruction
Major Potential Hazard, High plausibility.
The use of oral aminoglycosides is contraindicated in patients with intestinal obstruction. Orally administered aminoglycosides are poorly absorbed from the gastrointestinal tract and primarily eliminated unchanged in the feces. Drug retention and enhanced systemic absorption may occur in the presence of intestinal obstruction, increasing the risk of oto- and nephrotoxicity associated with these drugs.
Antibiotics (applies to neomycin) colitis
Major Potential Hazard, Moderate plausibility. Applicable conditions: Colitis/Enteritis (Noninfectious)
Clostridioides difficile-associated diarrhea (CDAD), formerly pseudomembranous colitis, has been reported with almost all antibacterial drugs and may range from mild diarrhea to fatal colitis. The most common culprits include clindamycin and lincomycin. Antibacterial therapy alters the normal flora of the colon, leading to overgrowth of C difficile, whose toxins A and B contribute to CDAD development. Morbidity and mortality are increased with hypertoxin-producing strains of C difficile; these infections can be resistant to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea after antibacterial use. Since CDAD has been reported to occur more than 2 months after antibacterial use, careful medical history is necessary. Therapy with broad-spectrum antibacterials and other agents with significant antibacterial activity should be administered cautiously in patients with history of gastrointestinal disease, particularly colitis; pseudomembranous colitis (generally characterized by severe, persistent diarrhea and severe abdominal cramps, and sometimes associated with the passage of blood and mucus), if it occurs, may be more severe in these patients and may be associated with flares in underlying disease activity. Antibacterial drugs not directed against C difficile may need to be stopped if CDAD is suspected or confirmed. Appropriate fluid and electrolyte management, protein supplementation, antibacterial treatment of C difficile, and surgical evaluation should be started as clinically indicated.
Neomycin (oral solution) (applies to neomycin) GI inflammation
Major Potential Hazard, High plausibility. Applicable conditions: Colitis/Enteritis (Noninfectious), Colonic Ulceration
The use of neomycin oral solution is contraindicated in patients with inflammatory or ulcerative gastrointestinal diseases because of the potential for enhanced absorption of neomycin. Like other aminoglycosides, neomycin is potentially oto- and nephrotoxic, and systemic exposure should be avoided if possible.
Neomycin drug interactions
There are 160 drug interactions with neomycin.
More about neomycin
- neomycin consumer information
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (1)
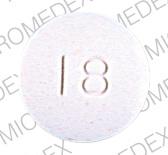
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Support group
- Drug class: aminoglycosides
- Breastfeeding
- En español
Related treatment guides
Drug Interaction Classification
| Highly clinically significant. Avoid combinations; the risk of the interaction outweighs the benefit. | |
| Moderately clinically significant. Usually avoid combinations; use it only under special circumstances. | |
| Minimally clinically significant. Minimize risk; assess risk and consider an alternative drug, take steps to circumvent the interaction risk and/or institute a monitoring plan. | |
| No interaction information available. |
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.