Linezolid Disease Interactions
There are 12 disease interactions with linezolid.
- Colitis
- Bone marrow suppression
- Acidosis
- Carcinoid syndrome
- Hemodialysis
- Hypertension
- Hypoglycemia
- Liver disease
- MAOI activity
- Neuropathy
- Renal dysfunction
- Seizures
Antibiotics (applies to linezolid) colitis
Major Potential Hazard, Moderate plausibility. Applicable conditions: Colitis/Enteritis (Noninfectious)
Clostridioides difficile-associated diarrhea (CDAD), formerly pseudomembranous colitis, has been reported with almost all antibacterial drugs and may range from mild diarrhea to fatal colitis. The most common culprits include clindamycin and lincomycin. Antibacterial therapy alters the normal flora of the colon, leading to overgrowth of C difficile, whose toxins A and B contribute to CDAD development. Morbidity and mortality are increased with hypertoxin-producing strains of C difficile; these infections can be resistant to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea after antibacterial use. Since CDAD has been reported to occur more than 2 months after antibacterial use, careful medical history is necessary. Therapy with broad-spectrum antibacterials and other agents with significant antibacterial activity should be administered cautiously in patients with history of gastrointestinal disease, particularly colitis; pseudomembranous colitis (generally characterized by severe, persistent diarrhea and severe abdominal cramps, and sometimes associated with the passage of blood and mucus), if it occurs, may be more severe in these patients and may be associated with flares in underlying disease activity. Antibacterial drugs not directed against C difficile may need to be stopped if CDAD is suspected or confirmed. Appropriate fluid and electrolyte management, protein supplementation, antibacterial treatment of C difficile, and surgical evaluation should be started as clinically indicated.
Linezolid (applies to linezolid) bone marrow suppression
Major Potential Hazard, Moderate plausibility. Applicable conditions: Thrombocytopathy, Bone Marrow Depression/Low Blood Counts
Reversible myelosuppression, including anemia, leukopenia, pancytopenia and thrombocytopenia, has been reported during postmarketing use of linezolid, although a causal relationship has not been established. Thrombocytopenia was also reported in phase 3 comparator-controlled trials at dosages up to and including 600 mg every 12 hours for up to 28 days, and bleeding events were identified in thrombocytopenic patients in a compassionate use program for linezolid. Therapy with linezolid should be administered cautiously in patients with preexisting blood dyscrasias and in patients receiving concomitant medications that may produce myelosuppression. Complete blood counts should be monitored weekly, particularly if linezolid is administered for longer than 2 weeks. Discontinuation of therapy should be considered in patients who develop or have worsening myelosuppression.
Linezolid (applies to linezolid) acidosis
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Vomiting
Cases of lactic acidosis have been reported with the use of linezolid. Patients who develop recurrent nausea or vomiting, unexplained acidosis, or a low bicarbonate level while receiving linezolid should receive immediate medical evaluation.
Linezolid (applies to linezolid) carcinoid syndrome
Moderate Potential Hazard, Moderate plausibility.
Linezolid is a weak, reversible, nonselective monoamine oxidase inhibitor (MAOI). Nonspecific MAOIs inhibit the breakdown of pressor amines, including serotonin, and may exacerbate symptoms of the carcinoid syndrome. While adverse effects related to MAOI activity have not been reported with linezolid, the potential for excessive serotonergic effects should be considered. Therapy with linezolid should be administered cautiously in patients with carcinoid syndrome and in patients receiving serotonergic agents. Clinical data are not available concerning the use of linezolid in these populations.
Linezolid (applies to linezolid) hemodialysis
Moderate Potential Hazard, High plausibility.
Linezolid is partially removed by hemodialysis and should be administered after dialysis.
Linezolid (applies to linezolid) hypertension
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Pheochromocytoma, Thyrotoxicosis
Linezolid should not be administered to patients with uncontrolled hypertension, pheochromocytoma, thyrotoxicosis and/or patients taking any medication that could affect the pressor response unless patients are being monitored for potential increases in blood pressure. Caution and close monitoring are recommended when prescribing this agent to these patients.
Linezolid (applies to linezolid) hypoglycemia
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Diabetes Mellitus
Cases of symptomatic hypoglycemia have been reported in diabetic patients receiving insulin or oral hypoglycemic agents when treated with linezolid. Caution and close monitoring are recommended when prescribing this agent to a patient with diabetes mellitus.
Linezolid (applies to linezolid) liver disease
Moderate Potential Hazard, Moderate plausibility.
Linezolid is primarily metabolized by the liver. The pharmacokinetics of linezolid are not altered in patients with mild to moderate hepatic impairment (Child-Pugh class A or B) and, therefore, no dosage adjustments are necessary. Pharmacokinetic data are not available for patients with severe hepatic impairment. Therapy with linezolid should be administered cautiously in such patients.
Linezolid (applies to linezolid) MAOI activity
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Cerebral Vascular Disorder, Cardiovascular Disease, Pheochromocytoma, Hyperthyroidism
Linezolid is a weak, reversible, nonselective monoamine oxidase inhibitor (MAOI). Nonspecific MAOIs inhibit the breakdown of pressor amines, the accumulation of which can precipitate hypertensive crises. Intracranial hemorrhage and death have been reported with MAOI antidepressants. While adverse effects related to MAOI activity have not been reported with linezolid, the potential for severe hypertension should be considered. Therapy with linezolid should be administered cautiously in patients with cerebro- or cardiovascular disease, pheochromocytoma, or untreated hyperthyroidism. Clinical data are not available concerning the use of linezolid in this population. As a precaution, patients should have their blood pressure monitored during therapy and observed for signs and symptoms of a hypertensive reaction (e.g., occipital headache which may radiate frontally; palpitation; neck stiffness or soreness; nausea or vomiting; perspiration associated with fever or cold, clammy skin; mydriasis; photophobia; constricting chest pain).
Linezolid (applies to linezolid) neuropathy
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Peripheral Neuropathy, Optic Nerve Disorder
Peripheral and optic neuropathies have been reported in patients treated with linezolid. If patients experience symptoms of visual impairment, such as changes in visual acuity, changes in color vision, blurred vision, or visual field defect, prompt ophthalmic evaluation is recommended. Visual function should be monitored in all patients taking linezolid for extended periods and in all patients reporting new visual symptoms regardless of length of therapy with linezolid. If peripheral or optic neuropathy occurs, the continued use of linezolid in these patients should be weighed against the potential risks.
Linezolid (applies to linezolid) renal dysfunction
Moderate Potential Hazard, Moderate plausibility.
Linezolid is primarily metabolized by the liver and subsequently eliminated by the kidney. The pharmacokinetics of the parent drug are not altered in patients with impaired renal function and, therefore, no dosage adjustments are necessary. However, accumulation of the two primary metabolites may occur in such patients, the amount of which increases with the degree of renal impairment. The clinical significance of metabolite accumulation has not been determined. Therapy with linezolid should be administered cautiously in patients with renal impairment and only if benefits outweigh the potential risks.
Linezolid (applies to linezolid) seizures
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Head Injury
Caution is recommended when prescribing linezolid to patients with a history of seizures or risk factors for seizures as convulsions have been reported with the use of this agent. Close monitoring is recommended.
Linezolid drug interactions
There are 519 drug interactions with linezolid.
Linezolid alcohol/food interactions
There are 2 alcohol/food interactions with linezolid.
More about linezolid
- linezolid consumer information
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (32)
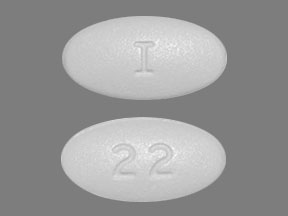
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: oxazolidinone antibiotics
- Breastfeeding
- En español
Related treatment guides
Drug Interaction Classification
| Highly clinically significant. Avoid combinations; the risk of the interaction outweighs the benefit. | |
| Moderately clinically significant. Usually avoid combinations; use it only under special circumstances. | |
| Minimally clinically significant. Minimize risk; assess risk and consider an alternative drug, take steps to circumvent the interaction risk and/or institute a monitoring plan. | |
| No interaction information available. |
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.