Disopyramide Disease Interactions
There are 7 disease interactions with disopyramide.
- Cardiovascular dysfunction
- Anticholinergic activity
- Sinus-AV node dysfunction
- Electrolyte imbalance
- Hepatic dysfunction
- Hypoglycemia
- Renal dysfunction
Antiarrhythmics (applies to disopyramide) cardiovascular dysfunction
Major Potential Hazard, High plausibility. Applicable conditions: Hypotension, Congestive Heart Failure
Antiarrhythmic agents can induce severe hypotension (particularly with IV administration) or induce or worsen congestive heart failure (CHF). Patients with primary cardiomyopathy or inadequately compensated CHF are at increased risk. Antiarrhythmic agents should be administered cautiously and dosage and/or frequency of administration modified in patients with hypotension or adequately compensated CHF. Alternative therapy should be considered unless these conditions are secondary to cardiac arrhythmia.
Disopyramide (applies to disopyramide) anticholinergic activity
Major Potential Hazard, High plausibility. Applicable conditions: Glaucoma/Intraocular Hypertension, Myasthenia Gravis, Urinary Retention
Disopyramide has anticholinergic activity, and therapy with disopyramide should be administered with extreme caution in patients who may be adversely affected by this. Disopyramide should not be used in patients with glaucoma, myasthenia gravis, or urinary retention unless adequate overriding measures are taken.
Disopyramide (applies to disopyramide) sinus-AV node dysfunction
Major Potential Hazard, High plausibility. Applicable conditions: Heart Block, Cardiogenic Shock, Long QT Syndrome
The use of disopyramide is contraindicated in patients with cardiogenic shock, second- or third-degree AV block in the absence of a functional artificial pacemaker, or congenital QT prolongation. Therapy with disopyramide should be administered with extreme caution in patients with sick sinus syndrome (bradycardia-tachycardia), Wolff-Parkinson White syndrome, or bundle-branch block. The effect of disopyramide in these conditions has not been determined.
Antiarrhythmics (applies to disopyramide) electrolyte imbalance
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Hyperkalemia, Hypokalemia, Magnesium Imbalance
Electrolyte imbalance can alter the therapeutic effectiveness of antiarrhythmic agents. Hypokalemia and hypomagnesemia can reduce the effectiveness of antiarrhythmic agents. In some cases, these disorders can exaggerate the degree of QTc prolongation and increase the potential for torsade de pointes. Hyperkalemia can potentiate the toxic effects of antiarrhythmic agents. Electrolyte imbalance should be corrected prior to initiating antiarrhythmic therapy. Clinical monitoring of cardiac function and electrolyte concentrations is recommended.
Disopyramide (applies to disopyramide) hepatic dysfunction
Moderate Potential Hazard, High plausibility. Applicable conditions: Liver Disease
Disopyramide is partially metabolized by the liver. The plasma half-life of disopyramide is prolonged in patients with hepatic dysfunction. Therapy with disopyramide should be administered cautiously and dosages reduced in patients with compromised hepatic function. Clinical monitoring of cardiac function (ECG) and hepatic function is recommended.
Disopyramide (applies to disopyramide) hypoglycemia
Moderate Potential Hazard, Low plausibility. Applicable conditions: Diabetes Mellitus
Rare cases of hypoglycemia have been reported during administration of disopyramide. Therapy with disopyramide should be administered cautiously in patients with diabetes mellitus or other conditions that alter normal glucoregulatory mechanisms such as chronic malnutrition, congestive heart failure, renal or hepatic dysfunction, or drugs (beta blockers).
Disopyramide (applies to disopyramide) renal dysfunction
Moderate Potential Hazard, High plausibility.
Disopyramide is primarily eliminated by the kidney. Approximately 50% of disopyramide is excreted in the urine as unchanged drug. The serum concentration of disopyramide is increased and the elimination half-life is prolonged in patients with renal impairment. Patients with renal impairment may be at increased risk of disopyramide-associated toxicity such as hypotension, conduction disturbances, or worsening of congestive heart failure. Therapy with disopyramide should be administered cautiously and dosage and/or frequency of administration modified in patients with compromised renal function. Clinical monitoring of cardiac function (ECG) and renal function is recommended.
Switch to professional interaction data
Disopyramide drug interactions
There are 590 drug interactions with disopyramide.
Disopyramide alcohol/food interactions
There are 2 alcohol/food interactions with disopyramide.
More about disopyramide
- disopyramide consumer information
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (7)
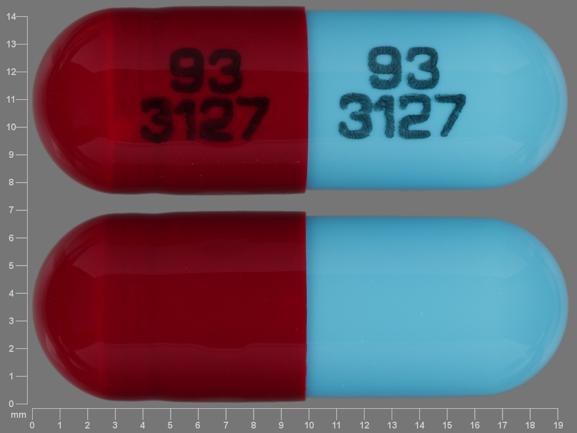
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: group I antiarrhythmics
- Breastfeeding
- En español
Related treatment guides
Drug Interaction Classification
| Highly clinically significant. Avoid combinations; the risk of the interaction outweighs the benefit. | |
| Moderately clinically significant. Usually avoid combinations; use it only under special circumstances. | |
| Minimally clinically significant. Minimize risk; assess risk and consider an alternative drug, take steps to circumvent the interaction risk and/or institute a monitoring plan. | |
| No interaction information available. |
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.