Amlodipine/atorvastatin Disease Interactions
There are 9 disease interactions with amlodipine / atorvastatin.
- Cardiogenic shock/hypotension
- Coronary artery disease
- Liver disease
- Liver disease
- CHF/AMI
- Cognitive impairment
- Diabetes
- Renal disease
- Rhabdomyolysis
CCBs (applies to amlodipine/atorvastatin) cardiogenic shock/hypotension
Major Potential Hazard, High plausibility. Applicable conditions: Aortic Stenosis
In general, calcium channel blockers (CCBs) should not be used in patients with hypotension (systolic pressure < 90 mm Hg) or cardiogenic shock. Due to potential negative inotropic and peripheral vasodilating effects, the use of CCBs may further depress cardiac output and blood pressure, which can be detrimental in these patients. The use of verapamil and diltiazem is specifically contraindicated under these circumstances.
CCBs (applies to amlodipine/atorvastatin) coronary artery disease
Major Potential Hazard, Low plausibility. Applicable conditions: Ischemic Heart Disease
Increased frequency, duration, and/or severity of angina, as well as acute myocardial infarction, have rarely developed during initiation or dosage increase of calcium channel blockers (CCBs), particularly in patients with severe obstructive coronary artery disease and those treated with immediate-release formulations. The mechanism of this effect is not established. Therapy with CCBs should be administered cautiously in patients with significant coronary artery disease.
CCBs (applies to amlodipine/atorvastatin) liver disease
Major Potential Hazard, High plausibility.
Calcium channel blockers (CCBs) are extensively metabolized by the liver. The half-lives of CCBs may be prolonged substantially in patients with severe hepatic impairment, with the potential for significant drug accumulation. In addition, the use of some CCBs has been associated with elevations in serum transaminases, both with and without concomitant elevations in alkaline phosphatase and bilirubin. While these effects may be transient and reversible, some patients have developed cholestasis or hepatocellular injury. Therapy with CCBs should be administered cautiously and often at reduced dosages in patients with significantly impaired hepatic function. Periodic monitoring of liver function is advised.
HMG-CoA reductase inhibitors (applies to amlodipine/atorvastatin) liver disease
Major Potential Hazard, Moderate plausibility. Applicable conditions: Alcoholism
The use of most HMG-CoA reductase inhibitors is contraindicated in patients with active liver disease, decompensated cirrhosis, or unexplained persistent elevations of serum transaminases. HMG-CoA reductase inhibitors are extensively metabolized by the liver. Decreased drug metabolism may lead to accumulation and increased risk of toxicity, including biochemical abnormalities of liver function and, rarely, jaundice, hepatitis, cirrhosis, fatty change in the liver, and fulminant hepatic necrosis. Therapy with HMG-CoA reductase inhibitors should be administered cautiously in patients with a history of liver disease and/or heavy alcohol use. A lower initial dosage may be appropriate, and clinical monitoring of liver transaminase levels according to the individual manufacturer product information is recommended. Patients who develop elevated ALT or AST levels during therapy should be monitored until abnormalities resolve. If an increase above 3 times the upper limit of normal persists, consideration should be given to a reduction in dosage or withdrawal of therapy.
CCBs (applies to amlodipine/atorvastatin) CHF/AMI
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Congestive Heart Failure, Myocardial Infarction
Calcium channel blockers (CCBs) may have varying degrees of negative inotropic effect. Congestive heart failure (CHF), worsening of CHF, and pulmonary edema have occurred in some patients treated with a CCB, primarily verapamil. Some CCBs have also caused mild to moderate peripheral edema due to localized vasodilation of dependent arterioles and small blood vessels, which can be confused with the effects of increasing left ventricular dysfunction. Although some CCBs have been used in the treatment of CHF, therapy with CCBs should be administered cautiously in patients with severe left ventricular dysfunction (e.g., ejection fraction < 30%) or moderate to severe symptoms of cardiac failure and in patients with any degree of ventricular dysfunction if they are receiving a beta-adrenergic blocker. Likewise, caution is advised in patients with acute myocardial infarction and pulmonary congestion documented by X-ray on admission, since associated heart failure may be acutely worsened by administration of a CCB.
HMG-CoA reductase inhibitors (applies to amlodipine/atorvastatin) cognitive impairment
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: CNS Disorder
Cognitive impairment (e.g., memory loss, forgetfulness, amnesia, memory impairment, confusion) have been observed in patients receiving statins. The reports are usually not serious, and reversible upon statin discontinuation. Caution is recommended when using these agents in patients with cognitive impairment.
HMG-CoA reductase inhibitors (applies to amlodipine/atorvastatin) diabetes
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Diabetes Mellitus
Increases in hemoglobin A1c and fasting serum glucose levels have been reported with the use of certain HMG-CoA reductase inhibitors. Caution should be exercised when using these agents in diabetic patients and close monitoring is recommended.
HMG-CoA reductase inhibitors (applies to amlodipine/atorvastatin) renal disease
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Renal Dysfunction
Some HMG-CoA reductase inhibitors (e.g., fluvastatin) have not been studied in patients with severe renal dysfunction or end-stage renal disease. Some others (e.g., pitavastatin, simvastatin) require a dose reduction when used in this group of patients. Caution and close monitoring are advised when using these drugs in patients with renal dysfunction.
HMG-CoA reductase inhibitors (applies to amlodipine/atorvastatin) rhabdomyolysis
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Myopathy, Myoneural Disorder, Hypothyroidism, Renal Dysfunction
HMG-CoA reductase inhibitors may cause myopathy and rhabdomyolysis; acute renal failure secondary to myoglobinuria and rare fatalities have occurred due to rhabdomyolysis in patients treated with statins. The myopathy may be dose-related and is characterized by unexplained muscle weakness, pain, or tenderness accompanied by increases in creatine phosphokinase (CPK) values exceeding 10 times the upper limit of normal. Therapy with HMG-CoA reductase inhibitors should be administered cautiously in patients with preexisting myopathy, in those with predisposing factors for myopathy, or with a history of myoneural disorder, since it may delay the recognition or confound the diagnosis of a drug-induced musculoskeletal effect. Patients should be advised to report promptly any unusual muscle pain, tenderness, or weakness, particularly if accompanied by malaise or fever. Periodic CPK determinations may be considered in some patients, although the value of such monitoring is uncertain. HMG-CoA reductase inhibitor therapy should be withdrawn if markedly elevated CPK levels occur or if drug-related myopathy is diagnosed or suspected.
Switch to professional interaction data
Amlodipine/atorvastatin drug interactions
There are 757 drug interactions with amlodipine / atorvastatin.
Amlodipine/atorvastatin alcohol/food interactions
There are 4 alcohol/food interactions with amlodipine / atorvastatin.
More about amlodipine / atorvastatin
- amlodipine/atorvastatin consumer information
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (6)
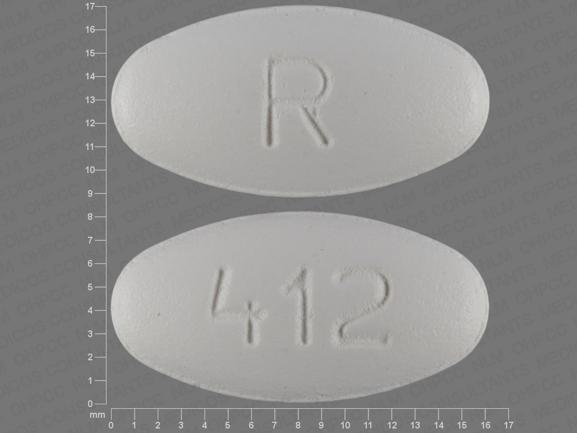
- Drug images
- Latest FDA alerts (2)
- Side effects
- Dosage information
- During pregnancy
- Drug class: antihyperlipidemic combinations
- En español
Related treatment guides
Drug Interaction Classification
| Highly clinically significant. Avoid combinations; the risk of the interaction outweighs the benefit. | |
| Moderately clinically significant. Usually avoid combinations; use it only under special circumstances. | |
| Minimally clinically significant. Minimize risk; assess risk and consider an alternative drug, take steps to circumvent the interaction risk and/or institute a monitoring plan. | |
| No interaction information available. |
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.