Sirolimus (Oral)
Generic name: sirolimus [ sir-OH-li-mus ]
Brand name: Rapamune
Drug classes: MTOR inhibitors, Selective immunosuppressants
Medically reviewed by Drugs.com. Last updated on Mar 12, 2025.
Increased susceptibility to infection and the possible development of lymphoma and other malignancies may result from immunosuppression
Increased susceptibility to infection and the possible development of lymphoma may result from immunosuppression. Only physicians experienced in immunosuppressive therapy and management of renal transplant patients should use sirolimus for prophylaxis of organ rejection in patients receiving renal transplants. Patients receiving the drug should be managed in facilities equipped and staffed with adequate laboratory and supportive medical resources. The physician responsible for maintenance therapy should have complete information requisite for the follow-up of the patient.
The safety and efficacy of sirolimus as immunosuppressive therapy have not been established in liver or lung transplant patients, and therefore, such use is not recommended.
Liver Transplantation - Excess Mortality, Graft Loss, and Hepatic Artery Thrombosis (HAT)The use of sirolimus in combination with tacrolimus was associated with excess mortality and graft loss in a study in de novo liver transplant patients. Many of these patients had evidence of infection at or near the time of death. In this and another study in de novo liver transplant patients, the use of sirolimus in combination with cyclosporine or tacrolimus was associated with an increase in HAT; most cases of HAT occurred within 30 days post-transplantation and most led to graft loss or death.
Lung Transplantation - Bronchial Anastomotic Dehiscence
Cases of bronchial anastomotic dehiscence, most fatal, have been reported in de novo lung transplant patients when sirolimus has been used as part of an immunosuppressive regimen .
Uses for sirolimus
Sirolimus is used together with other medicines to prevent the body from rejecting a transplanted kidney. It belongs to a group of medicines known as immunosuppressive agents.
When a patient receives an organ transplant, the body's white blood cells will try to get rid of (reject) the transplanted organ. Sirolimus works by preventing the white blood cells from getting rid of the transplanted organ.
Sirolimus is a very strong medicine. It can cause side effects that can be very serious, such as kidney problems. It may also reduce the body's ability to fight infections. You and your doctor should talk about the benefits of this medicine as well as the risks.
Sirolimus is also used to treat lymphangioleiomyomatosis, a rare lung disease that affects predominantly women of childbearing age.
This medicine is available only with your doctor's prescription.
Before using sirolimus
In deciding to use a medicine, the risks of taking the medicine must be weighed against the good it will do. This is a decision you and your doctor will make. For this medicine, the following should be considered:
Allergies
Tell your doctor if you have ever had any unusual or allergic reaction to this medicine or any other medicines. Also tell your health care professional if you have any other types of allergies, such as to foods, dyes, preservatives, or animals. For non-prescription products, read the label or package ingredients carefully.
Pediatric
Appropriate studies have not been performed on the relationship of age to the effects of sirolimus in children younger than 13 years of age or in children considered to be at high immunologic risk for prevention of kidney transplant rejection, and in children for treatment of lymphangioleiomyomatosis. Safety and efficacy have not been established in these age groups.
Geriatric
Appropriate studies performed to date have not demonstrated geriatric-specific problems that would limit the usefulness of sirolimus in the elderly. However, elderly patients are more likely to have liver and heart problems, which may require caution and an adjustment in the dose for patients receiving sirolimus.
Breast Feeding
There are no adequate studies in women for determining infant risk when using this medication during breastfeeding. Weigh the potential benefits against the potential risks before taking this medication while breastfeeding.
Interactions with Medicines
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are taking this medicine, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using this medicine with any of the following medicines is not recommended. Your doctor may decide not to treat you with this medication or change some of the other medicines you take.
- Levoketoconazole
- Mifepristone
- Posaconazole
- Ritonavir
- Voriconazole
Using this medicine with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Abrocitinib
- Adagrasib
- Adenovirus Vaccine Type 4, Live
- Adenovirus Vaccine Type 7, Live
- Alefacept
- Amiodarone
- Asciminib
- Avacopan
- Bacillus of Calmette and Guerin Vaccine, Live
- Belzutifan
- Benazepril
- Berotralstat
- Boceprevir
- Cannabidiol
- Capmatinib
- Captopril
- Ceritinib
- Clarithromycin
- Cobicistat
- Conivaptan
- Crizotinib
- Dabrafenib
- Daridorexant
- Darunavir
- Dengue Tetravalent Vaccine, Live
- Dronedarone
- Duvelisib
- Efavirenz
- Elacestrant
- Eluxadoline
- Enalapril
- Enalaprilat
- Enasidenib
- Enzalutamide
- Erdafitinib
- Etravirine
- Fedratinib
- Fexinidazole
- Fluconazole
- Fosinopril
- Fosnetupitant
- Idelalisib
- Infliximab
- Influenza Virus Vaccine, Live
- Isavuconazonium Sulfate
- Itraconazole
- Ivacaftor
- Ivosidenib
- Ketoconazole
- Lanreotide
- Larotrectinib
- Lasmiditan
- Lefamulin
- Lenacapavir
- Letermovir
- Lisinopril
- Lorlatinib
- Lumacaftor
- Mavacamten
- Measles Virus Vaccine, Live
- Methotrexate
- Metoclopramide
- Micafungin
- Mirabegron
- Mitapivat
- Mitotane
- Mobocertinib
- Moexipril
- Mumps Virus Vaccine, Live
- Neratinib
- Netupitant
- Nirmatrelvir
- Octreotide
- Olutasidenib
- Omaveloxolone
- Pacritinib
- Palbociclib
- Pazopanib
- Perindopril
- Phenobarbital
- Pirtobrutinib
- Poliovirus Vaccine, Live
- Primidone
- Quinapril
- Ramipril
- Ribociclib
- Rifampin
- Ritlecitinib
- Rotavirus Vaccine, Live
- Rubella Virus Vaccine, Live
- Saquinavir
- Selpercatinib
- Simeprevir
- Smallpox Vaccine
- Sotorasib
- Sparsentan
- St John's Wort
- Tacrolimus
- Taurursodiol
- Telaprevir
- Telithromycin
- Tepotinib
- Tocilizumab
- Trandolapril
- Trofinetide
- Tucatinib
- Typhoid Vaccine, Live
- Varicella Virus Vaccine, Live
- Venetoclax
- Verapamil
- Vilazodone
- Voxelotor
- Yellow Fever Vaccine
- Zofenopril
- Zoster Vaccine, Live
Using this medicine with any of the following medicines may cause an increased risk of certain side effects, but using both drugs may be the best treatment for you. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Amprenavir
- Aprepitant
- Cyclosporine
- Diltiazem
- Erythromycin
- Fosphenytoin
- Nevirapine
- Phenytoin
- Rifabutin
- Semaglutide
Interactions with Food/Tobacco/Alcohol
Certain medicines should not be used at or around the time of eating food or eating certain types of food since interactions may occur. Using alcohol or tobacco with certain medicines may also cause interactions to occur. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using this medicine with any of the following may cause an increased risk of certain side effects but may be unavoidable in some cases. If used together, your doctor may change the dose or how often you use this medicine, or give you special instructions about the use of food, alcohol, or tobacco.
- Grapefruit Juice
Other Medical Problems
The presence of other medical problems may affect the use of this medicine. Make sure you tell your doctor if you have any other medical problems, especially:
- Ascites (fluid in the stomach) or
- Blood clotting problems (eg, thrombotic microangiopathy, thrombotic thrombocytopenic purpura) or
- Heart disease (eg, pericardial effusion) or
- Hyperlipidemia (high amount of cholesterol and fats in the blood) or
- Infection (eg, bacteria, fungus, virus) or
- Lung disease (eg, bronchiolitis obliterans organizing pneumonia [BOOP], pleural effusion, pneumonitis, pulmonary fibrosis) or
- Lymphoma (cancer of the lymph glands) or
- Peripheral edema (swelling of the hands, ankles, or feet) or
- Proteinuria (protein in the urine) or
- Skin cancer, history of—Use with caution. May make these conditions worse.
- Liver disease—Use with caution. You may require a smaller dose.
- Liver transplantation or
- Lung transplantation—Use is not recommended in patients with these conditions.
Proper use of sirolimus
Take this medicine only as directed by your doctor. Do not take more of it, do not take it more often, and do not take it for a longer time than your doctor ordered. The exact amount of medicine you need has been carefully worked out. Using too much will increase the risk of side effects, while using too little may lead to rejection of your transplanted kidney.
This medicine usually comes with a Medication Guide and patient instructions. Read them carefully and make sure you understand them before taking this medicine. If you have any questions, ask your doctor.
Take this medicine the same way every day. This means take it at the same time and consistently, either with or without food.
Do not change your dose or stop taking this medicine without checking first with your doctor. You may have to take this medicine for the rest of your life to prevent your body from rejecting the kidney transplant.
Sirolimus is usually used along with a corticosteroid (cortisone-like medicine) and cyclosporine. Sirolimus should be taken 4 hours after cyclosporine modified oral solution or cyclosporine modified capsules (Neoral®). If you have any questions about this, ask your doctor.
If you have been taking sirolimus together with cyclosporine for 2 to 4 months after your transplant, your doctor may want you to stop using cyclosporine and increase the dose of sirolimus. However, some patients (eg, black patients or those with transplant rejection in the past) may need to continue using cyclosporine for up to one year after the transplant. Your doctor will tell you if you need to keep taking cyclosporine.
Swallow the tablet whole. Do not crush, break, or chew it. If you are unable to take the tablet form, your doctor will give you an oral liquid and be given instructions on how to take it.
To use the oral liquid:
- Open the solution bottle and insert the adapter tightly into the bottle.
- Insert the amber syringe that comes with the bottle to draw the right amount of medicine out of the bottle.
- Empty the medicine from the syringe into a glass or plastic cup.
- Mix the medicine with at least 2 ounces (¼ cup or 60 milliliters [mL]) of water or orange juice. Stir the mixture well and drink it immediately.
- Add at least 4 ounces (½ cup or 120 mL) of additional water or orange juice, stir it well, and drink it to make sure that all of the medicine is taken.
- If you have been instructed by your doctor to carry your medicine, you may keep your daily dose of sirolimus in a tightly-capped syringe for a maximum of 24 hours at room temperature or in the refrigerator. Throw away the used syringe after each use.
If this medicine gets into your skin, wash it with soap and water right away. If it gets in your eyes, rinse them with water.
You should not eat grapefruit or drink grapefruit juice while you are taking this medicine. Grapefruit and grapefruit juice may cause higher levels of sirolimus in the body. This could result in more unwanted effects.
Dosing
The dose of this medicine will be different for different patients. Follow your doctor's orders or the directions on the label. The following information includes only the average doses of this medicine. If your dose is different, do not change it unless your doctor tells you to do so.
The amount of medicine that you take depends on the strength of the medicine. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take the medicine depend on the medical problem for which you are using the medicine.
- For oral dosage forms (oral solution or tablets):
- For prevention of kidney transplant rejection:
- Adults and children 13 years of age and older weighing 40 kilograms (kg) or more—2 milligrams (mg) per day after an initial one-time dose of 6 mg. Some patients may require a dose of up to 5 mg per day after an initial one-time dose of 15 mg. However, the dose is usually not more than 40 mg per day.
- Children 13 years of age and older weighing less than 40 kg—Dose is based on body size as determined by your doctor. The dose is 1 milligram (mg) per square meter [m(2)] of body surface area once a day after an initial one-time dose of 3 mg per square meter [m(2)] of body surface area.
- Children younger than 13 years of age—Use and dose must be determined by your doctor.
- For treatment of lymphangioleiomyomatosis:
- Adults—At first, 2 milligrams (mg) per day. Your doctor may adjust your dose as needed.
- Children—Use and dose must be determined by your doctor.
- For prevention of kidney transplant rejection:
Storage
Keep out of the reach of children.
Do not keep outdated medicine or medicine no longer needed.
Ask your healthcare professional how you should dispose of any medicine you do not use.
Store the tablets at room temperature in a closed container, away from heat, moisture, and direct light.
Store the oral liquid in the refrigerator. Protect it from direct light and moisture. Do not freeze. You may store the oral liquid at room temperature for a short period of time (not more than 15 days). If you see a slight haze or cloudiness in the bottle, leave it out at room temperature and shake it until the haze disappears. Throw away any unused medicine after 30 days.
Precautions while using sirolimus
It is very important that your doctor check your or your child's progress at regular visits to make sure that this medicine is working properly. Blood and urine tests may be needed to check for unwanted effects.
Using this medicine while you are pregnant can harm your unborn baby. Use an effective form of birth control to keep from getting pregnant, and keep using it for at least 12 weeks after you stop taking sirolimus. If you think you have become pregnant while using the medicine, tell your doctor right away.
If you are planning to have children, talk with your doctor before using this medicine. Some men and women using this medicine have become infertile (unable to have children).
Using this medicine may increase your risk of getting skin cancer or cancer of the lymph system (lymphoma). Talk to your doctor if you have concerns about this risk.
This medicine may increase your risk of developing infections. Avoid being near people who are sick while you are using this medicine. Wash your hands often. Tell your doctor if you have any kind of infection before you start using this medicine. Tell your doctor if you have ever had an infection that would not go away or an infection that kept coming back.
Sirolimus may cause serious types of allergic reactions, including anaphylaxis,, which can be life-threatening and require immediate medical attention. Call your doctor right away if you or your child has a rash, itching, red, swollen skin, trouble breathing, trouble swallowing, or chest tightness while you are using this medicine.
Sirolimus may cause a serious type of allergic reaction called angioedema. This may occur more often when it is used with certain heart and blood pressure medicines called ACE inhibitors (eg, captopril [Capoten®], enalapril [Vasotec®], fosinopril [Monopril®], quinapril [Accupril®], ramipril [Altace®]). Check with your doctor right away if you have a rash, itching, a large, hive-like swelling on the face, eyelids, lips, tongue, throat, hands, legs, feet, or genitals, trouble breathing, or chest tightness while you are using this medicine.
This medicine may also increase your risk of bleeding and cause delay in wound healing. Stay away from rough sports or other situations where you could be bruised, cut, or injured. Brush and floss your teeth gently. Be careful when using sharp objects, including razors and fingernail clippers. Check with your doctor immediately if you or your child notice any unusual bleeding or bruising, black, tarry stools, blood in the urine or stools, or pinpoint red spots on your skin.
This medicine may increase your cholesterol and fats in the blood. If this condition occurs, your doctor may give you or your child some medicines that can lower the amount of cholesterol and fats in the blood.
This medicine may increase your risk of developing a rare and serious virus infection called BK virus-associated nephropathy (BKVAN). The BK virus may affect how your kidneys work and cause a transplanted kidney to fail. Check with your doctor right away if you or your child has bloody urine, a decreased frequency or amount of urine, increased thirst, loss of appetite, lower back or side pain, nausea, swelling of the face, fingers, or lower legs, trouble breathing, unusual tiredness or weakness, vomiting, or weight gain.
This medicine may cause a serious lung problem called interstitial lung disease or non-infectious pneumonitis. Check with your doctor right away if you have chest pain, chills, cough, fever, or trouble breathing.
This medicine may increase your risk of developing a serious and rare brain infection called progressive multifocal leukoencephalopathy (PML). Check with your doctor right away if you or your child has vision changes, loss of coordination, clumsiness, confusion, memory loss, difficulty speaking or understanding what others say, and weakness in the legs.
This medicine may make your skin more sensitive to sunlight and can increase your risk of having skin cancer. Use a sunscreen when you are outdoors and avoid sunlamps and tanning beds.
While you are being treated with sirolimus, and after you stop treatment with it, it is important to see your doctor about the immunizations (vaccinations) you should receive. Do not get any immunizations (vaccines) without your doctor's approval. Sirolimus may lower your body's resistance and there is a chance you might get the infection the vaccine is meant to prevent. In addition, you should not be around other persons living in your household who receive live virus vaccines because there is a chance they could pass the virus on to you. Some examples of live vaccines include measles, mumps, influenza (nasal flu vaccine), poliovirus (oral form), rotavirus, and rubella. Do not get close to them and do not stay in the same room with them for very long. If you have questions about this, talk to your doctor.
Check with your doctor right away if you notice a new mole, a change in size, shape or color of an existing mole, or a mole that leaks fluid or bleeds.
While you are taking sirolimus, it is important to maintain good dental hygiene and see a dentist regularly for teeth cleaning.
Raw oysters or other shellfish may contain bacteria that can cause serious illness and possibly death. This is more likely to be a problem if these foods are eaten by patients with certain medical conditions. Even eating oysters from “clean” water or good restaurants does not guarantee that the oysters do not contain the bacteria. Eating raw shellfish is not a problem for most healthy people, however, patients with the following conditions may be at greater risk: cancer, immune disorders, organ transplantation, long-term corticosteroid use (as for asthma, arthritis, or organ transplantation), liver disease (including viral hepatitis), excess alcohol intake (2 to 3 drinks or more per day), diabetes, stomach problems (including stomach surgery and low stomach acid), and hemochromatosis (an iron disorder). Do not eat raw oysters or other shellfish while you are taking sirolimus. Be sure oysters and shellfish are fully cooked.
Do not take other medicines unless they have been discussed with your doctor. This includes prescription or nonprescription (over-the-counter [OTC]) medicines and herbal (eg, St. John's wort) or vitamin supplements.
Side Effects of sirolimus
Along with its needed effects, a medicine may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur:
More common
- Accumulation of pus
- anxiousness, unexplained
- backache
- black or red, tarry stools
- bleeding from the gums or nose
- blurred vision
- body aches or pain
- bone pain
- bruising
- burning or stinging of the skin
- burning while urinating
- burning, dry, or itching eyes
- burning, tingling, numbness, or pain in the hands, arms, feet, or legs
- change in mental status
- changes in skin color
- chest pain
- chills
- confusion
- cough
- dark or bloody urine
- deafness
- decreased urine output
- decreased vision
- difficulty with breathing or swallowing
- dilated neck veins
- discharge from the eyes
- dizziness
- drowsiness
- dry mouth
- earache
- excessive tearing
- eye pain
- facial hair growth in females
- faintness or lightheadedness when getting up from lying or sitting position
- fast, slow, or irregular heartbeat
- fever
- flushing or redness of the skin, especially on the face and neck
- general feeling of discomfort or illness
- increased hunger
- increased menstrual flow or vaginal bleeding
- itching, pain, redness, swelling, tenderness, or warmth on the skin
- lack or loss of appetite
- large, flat, blue, or purplish patches in the skin
- loss of sexual ability, desire, drive, or performance
- loss of voice
- muscle pain
- nasal congestion
- nausea or vomiting
- numbness or tingling around the lips, hands, or feet
- pain in the chest, groin, or legs, especially the calves
- painful cold sores or blisters on the lips, nose, eyes, or genitals
- pale skin
- prolonged bleeding from cuts
- rapid heartbeat
- rash
- red or dark brown urine
- redness or swelling in the ear
- redness, pain, or swelling of the eye, eyelid, or inner lining of the eyelid
- ringing in the ears
- runny nose
- seizures
- sensation of pins and needles
- severe constipation
- severe vomiting
- severe, sudden headache
- slurred speech
- sore throat
- sores or white spots on the lips or in the mouth
- stomach cramps, pain, or upset
- sudden decrease in the amount of urine
- sudden loss of coordination
- sudden, severe weakness or numbness in the arm or leg
- sweating
- swollen, painful, or tender lymph glands in the neck, armpit, or groin
- tenderness, pain, swelling, warmth, skin discoloration, and prominent superficial veins over affected area
- tremor
- ulcers on the lips or in the mouth
- unusual tiredness or weakness
- vision changes
- weakness or heaviness of the legs
- white patches in the mouth or on the tongue
- yellow skin and eyes
Less common
- Bloating
- change in size, shape, or color of existing mole
- hoarseness
- mole that leaks fluid or bleeds
- new mole
- pains in the stomach, side or abdomen, possibly radiating to the back
- skin ulcer or sores
Incidence not known
- Abnormal wound healing
- headache
- hives or itching
- large, hive-like swelling on the face, eyelids, lips, tongue, throat, hands, legs, feet, or sex organs
- nails loose or detached
- puffiness or swelling of the eyelids or around the eyes, face, lips, or tongue
- swelling of the arms or legs
- yellow nails lacking a cuticle
Some side effects may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects. Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common
- Abnormal vision
- acne
- belching
- blistering, crusting, irritation, itching, or reddening of the skin
- burning feeling in the chest or stomach
- burning, crawling, itching, numbness, prickling, "pins and needles", or tingling feeling
- constipation
- continuing ringing or buzzing or other unexplained noise in the ears
- cracked, dry, or scaly skin
- crying
- decrease in frequency of urination
- degenerative disease of the joint
- depersonalization
- diarrhea
- difficulty with moving
- difficulty with passing urine (dribbling)
- dysphoria
- ear pain
- enlarged abdomen or stomach
- euphoria
- excess air or gas in the stomach or intestines
- excessive muscle tone, muscle tension or tightness
- fear
- feeling sad or empty
- hearing loss
- heartburn
- inability to have or keep an erection
- increase in heart rate
- increased hair growth, especially on the face
- increased urge to urinate during the night
- indigestion
- irritation in the mouth
- joint pain or swelling
- leg cramps
- loss of bladder control
- loss of energy or weakness
- loss of interest or pleasure
- loss of strength
- lower abdominal or stomach pain
- muscle aches, pain, stiffness, or weakness
- nervousness
- pain in the back, ribs, arms, or legs
- pain or burning in the throat
- pain or tenderness around the eyes and cheekbones
- paranoia
- pelvic pain
- quick to react or overreact emotionally
- rapid breathing
- rapidly changing moods
- inflammation, redness, or swelling of the gums or mouth
- shaking or trembling
- shivering
- sleepiness
- sunken eyes
- swelling
- swelling of the scrotum
- tender or enlarged gums
- tenderness in the stomach area
- thickening of the skin
- trouble concentrating
- trouble sleeping
- waking to urinate at night
Other side effects not listed may also occur in some patients. If you notice any other effects, check with your healthcare professional.
Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
Related/similar drugs
CellCept
Cellcept (mycophenolate mofetil) is used to prevent rejection of a kidney, liver, or heart ...
Omvoh
Omvoh is used to treat moderate to severe ulcerative colitis or Crohn's disease in adults. This ...
Prograf
Prograf is used to prevent your body from rejecting a heart, liver, or kidney transplant. Learn ...
Rapamune
Rapamune (sirolimus) is used to prevent rejection in people who have received a kidney transplant ...
Afinitor
Afinitor prevents the growth of cancer cells and is used to treat advanced kidney cancer. Learn ...
Everolimus
Everolimus (Afinitor, Afinitor Disperz, Zortress) belongs to a class of drugs called kinase ...
Commonly used brand name(s)
In the U.S.
- Rapamune
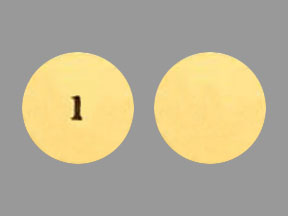
Available Dosage Forms:
- Tablet
- Solution
Therapeutic Class: Immune Suppressant
More about sirolimus
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (7)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: mTOR inhibitors
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.