Labetalol
Generic name: labetalol (oral/injection) [ la-BAY-ta-lol ]
Brand names: Trandate, Normodyne
Dosage forms: intravenous solution (100 mg/100 mL-NaCl 0.72%; 200 mg/200 mL-D5%; 200 mg/200 mL-NaCl 0.72%; 300 mg/300 mL-NaCl 0.72%; 5 mg/mL),
... show all 2 dosage forms
Drug class: Non-cardioselective beta blockers
What is labetalol?
Labetalol is a beta-blocker that is used to treat hypertension (high blood pressure). Labetalol oral is sometimes given with other blood pressure medications.
Labetalol injection is used when hypertension is severe.
Labetalol may also be used for purposes not listed in this medication guide.
Labetalol side effects
Get emergency medical help if you have signs of an allergic reaction: hives; difficulty breathing; swelling of your face, lips, tongue, or throat.
Labetalol may cause serious side effects. Call your doctor at once if you have:
-
a light-headed feeling, like you might pass out;
-
slow heart rate, weak pulse, fainting, slow breathing (breathing may stop);
-
shortness of breath (even with mild exertion), swelling, rapid weight gain;
-
severe headache, blurred vision, pounding in your neck or ears; or
-
liver problems--loss of appetite, stomach pain (upper right side), flu-like symptoms, itching, dark urine, jaundice (yellowing of the skin or eyes).
Severe dizziness or fainting may be more likely in older adults.
Common side effects of labetalol may include:
-
dizziness, drowsiness, tiredness;
-
nausea, vomiting;
-
sudden warmth, skin redness, sweating;
-
numbness; or
-
tingly feeling in your scalp.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Related/similar drugs
Lasix
Lasix is a loop diuretic used to treat fluid retention from heart, liver, or kidney conditions, and ...
Enalapril
Enalapril is used to treat high blood pressure, congestive heart failure and to improve survival ...
Repatha
Repatha (evolocumab) is a PCSK9 inhibitor used to lower high cholesterol alongside dietary changes ...
Bisoprolol
Bisoprolol belongs to a group of drugs called beta-blockers and is used to treat hypertension (high ...
Valsartan
Valsartan is an angiotensin II receptor blocker (ARB) that may be used to treat high blood pressure ...
Atenolol
Atenolol is used to treat angina (chest pain) and hypertension (high blood pressure). Learn about ...
Hydrochlorothiazide
HCTZ (hydrochlorothiazide) used to treat high blood pressure (hypertension) and edema. Includes ...
Propranolol
Propranolol is a beta-blocker that is used to treat tremors, chest pain, high blood pressure, heart ...
Furosemide
Furosemide is a loop diuretic used to treat fluid retention and high blood pressure by increasing ...
Warnings
Use only as directed. Tell your doctor if you use other medicines or have other medical conditions or allergies.
Before taking this medicine
You should not use labetalol if you are allergic to it, or if you have:
-
asthma;
-
"AV block" (2nd or 3rd degree);
-
uncontrolled heart failure;
-
very low blood pressure;
-
slow heartbeats that have caused you to faint; or
-
if your heart cannot pump blood properly.
Tell your doctor if you have ever had:
-
congestive heart failure;
-
angina (chest pain);
-
emphysema, chronic bronchitis, or other breathing problems;
-
pheochromocytoma (tumor of the adrenal gland);
-
diabetes;
-
coronary artery bypass surgery (sometimes called "CABG");
-
kidney disease; or
-
allergies.
Labetalol can affect your pupils. If you need eye surgery, tell the surgeon about your use of labetalol, even if you no longer take it.
Labetalol may cause low blood pressure, low blood sugar, slow heartbeats, or breathing problems in a newborn if the mother uses labetalol during pregnancy. Tell your doctor if you are pregnant or plan to become pregnant.
Ask a doctor if it is safe to breastfeed while using this medicine.
Not approved for use by anyone younger than 18 years old.
How should I use labetalol?
Follow all directions on your prescription label and read all medication guides or instruction sheets. Your doctor may occasionally change your dose. Use the medicine exactly as directed.
Labetalol oral is taken by mouth.
Labetalol injection is given in a vein by a healthcare provider when hypertension is severe. After the injection you may need to remain lying down for up to 3 hours. You may feel light-headed when you first stand up.
Your blood pressure will need to be checked often, and you may need other medical tests. If you have diabetes, check your blood sugar regularly.
Keep using this medicine as directed, even if you feel well. High blood pressure often has no symptoms.
Labetalol can cause false results with certain lab tests of the urine, including a drug-screening urine test. Tell the laboratory staff that you use labetalol.
Tell your doctor if you have a planned surgery.
You should not stop using labetalol suddenly. Stopping suddenly may make your condition worse.
Store at room temperature away from moisture and heat.
What happens if I miss a dose?
Take the medicine as soon as you can, but skip the missed dose if it is almost time for your next dose. Do not take two doses at one time.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222.
Overdose symptoms may include slow heart rate, wheezing, chest tightness, trouble breathing, extreme dizziness, seizure, or fainting.
What should I avoid while using labetalol?
Avoid driving or hazardous activity until you know how labetalol will affect you. Your reactions could be impaired.
Avoid getting up too fast from a sitting or lying position, or you may feel dizzy.
Drinking alcohol can further lower your blood pressure and may increase certain side effects of labetalol.
What other drugs will affect labetalol?
Tell your doctor about all your other medicines, especially:
-
any other blood pressure medicine;
-
heart medication;
-
insulin or oral diabetes medicine;
-
an antidepressant--amitriptyline, doxepin, desipramine, imipramine, nortriptyline, and others; or
-
a bronchodilator--albuterol, formoterol, levalbuterol, metaproterenol, olodaterol, salmeterol, and others.
This list is not complete. Other drugs may affect labetalol, including prescription and over-the-counter medicines, vitamins, and herbal products. Not all possible drug interactions are listed here.
More about labetalol
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (28)
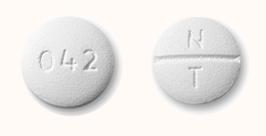
- Drug images
- Latest FDA alerts (3)
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Drug class: non-cardioselective beta blockers
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Related treatment guides
Further information
Remember, keep this and all other medicines out of the reach of children, never share your medicines with others, and use this medication only for the indication prescribed.
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Copyright 1996-2025 Cerner Multum, Inc. Version: 13.01.