Type 1 Diabetes Management for Adolescents
Medically reviewed by Drugs.com. Last updated on Dec 2, 2024.
AMBULATORY CARE:
What you need to know about managing type 1 diabetes:
As you get older, you will be able to manage your own health. You may be away from home more often. You may spend more time with your friends or be involved in sports. When you manage your blood sugar levels, you will feel well and be able to enjoy your activities. Your diabetes care team providers can show you how to fit diabetes care into your schedule. Adults, such as your parents and care team providers, are available to help you as you become more active in your diabetes care.
Have someone call your local emergency number (911 in the US) if:
- You cannot be woken.
- You have signs of diabetic ketoacidosis:
- confusion, fatigue
- vomiting
- rapid heartbeat
- fruity smelling breath
- extreme thirst
- dry mouth and skin
Call your doctor or diabetes care team provider if:
- You have a sore or wound that will not heal.
- You have a change in the amount you urinate.
- Your blood sugar levels are higher than your target goals.
- You often have lower blood sugar levels than your target goals.
- Your skin is red, dry, warm, or swollen.
- You have trouble coping with diabetes, or you feel anxious or depressed.
- You have questions or concerns about your condition or care.
Why you may still need diabetes education:
Your needs and wants change as you get older. Diabetes education will help you continue to manage type 1 diabetes, make changes to your plan, and prevent complications. As you get older, you may be able to do diabetes education on your phone or computer. Diabetes education can help you continue learning about the following:
- About your blood sugar level: You will be given information on when and how to check your blood sugar level. You will learn what your blood sugar level should be and what to do if it is too high or too low. Write down the times of your checks and your levels. Take them to all follow-up appointments.
- A glucose meter is a device that uses a test strip to check your blood sugar level. You put a small drop of blood from a finger on the test strip. The strip is put into the device. The device then figures out how much sugar is in your blood.

- A continuous glucose monitor (CGM) uses a sensor to check your blood sugar level. The sensor is placed on your abdomen or arm. A transmitter on the sensor gets a glucose reading. CGM data may be linked to an insulin pump.

- A glucose meter is a device that uses a test strip to check your blood sugar level. You put a small drop of blood from a finger on the test strip. The strip is put into the device. The device then figures out how much sugar is in your blood.
- About insulin: You will need insulin every day. You will learn how much insulin you need and when to use it. You will also be taught how to match insulin with blood sugar levels, activity, and carbohydrates. Insulin may be given through a pump or pen, or injected. You and your care team will discuss the best method for you:
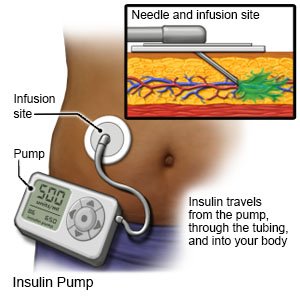
- An insulin pump is a wearable medical device that gives continuous insulin. An insulin pump prevents the need for multiple insulin injections in a day.
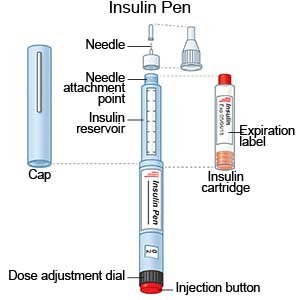
- An insulin pen is a device prefilled with insulin. Most insulin pens are disposable. You throw the pen away after it is empty or used for a certain amount of time. Some pens have a replaceable cartridge filled with insulin. You keep the pen and only throw away the cartridge.
- Insulin injections are given with a needle and syringe. You and your family members will be taught how to draw up and give insulin if this is the best method for you. You will also be taught how to dispose of used needles and syringes.
- An insulin pump is a wearable medical device that gives continuous insulin. An insulin pump prevents the need for multiple insulin injections in a day.
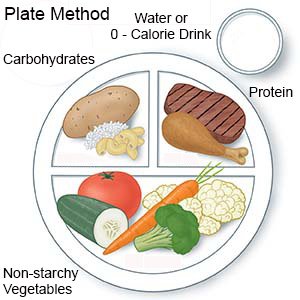
- About nutrition: A dietitian will help you make meal plans to keep your blood sugar level steady. You will learn how certain foods affect your blood sugar levels. You will also learn to keep track of sugar and starchy foods (carbs). Do not skip meals. Blood sugar levels may drop too low if you have had insulin and do not eat. You may need to check in with the dietitian at least 1 time per year.
- About physical activity and diabetes: You will learn why physical activity, such as exercise, is important. A plan will be made for you to get at least 60 minutes of moderate to intense aerobic activity every day. Examples of physical activity include brisk walking, dancing, running, and jumping rope. The plan will also include flexibility and resistance training, such as yoga and lifting weights, 3 days each week. You may need to have a snack before activity to prevent low blood sugar levels. Do not exercise if your blood sugar level is 350 mg/dL or higher. You may need to check your level before, during, and after exercise.

- About complications of diabetes: You will learn about complications, such as diabetic ketoacidosis (DKA), neuropathy, and retinopathy. You will learn how to prevent and recognize some of these complications. You will also learn about conditions that may happen with diabetes, such as high blood pressure and high cholesterol.
What you need to know about high blood sugar levels:
High blood sugar levels may not cause any symptoms. You may feel more thirsty than usual or urinate more often than usual. You may need to check for ketones in your urine or blood if your level is higher than directed. Ask your care team provider when and how to check for ketones. High blood sugar levels that are not controlled can lead to diabetic ketoacidosis (DKA). This is a serious condition that can become life-threatening.
- A lower dose of insulin or a late dose can raise your blood sugar level. There is not enough time for your insulin to work as it should if you take it late. When you take a lower dose of insulin, there is not enough insulin needed to lower your blood sugar level.
- Large meals or large amounts of carbs at one time can raise your blood sugar level. You may need to adjust your insulin dose to handle these changes.
- Decreased physical activity can raise your blood sugar level. For example, your blood sugar level can increase if you stop playing a sport or getting regular physical activity. Do not sit for longer than 90 minutes at a time.
- Stress can raise your blood sugar level. Ask your parents or care team provider for help if you are having trouble managing stress.
- Illness can raise your blood sugar level. This can happen even if you eat less than usual while you are sick. Work with your care team provider and parents to develop a sick day plan. This is a plan that helps you manage your blood sugar levels while you are sick.
What you need to know about low blood sugar levels:
You can prevent symptoms such as shakiness, dizziness, irritability, or confusion by preventing your blood sugar level from going too low.
- Treat low blood sugar levels right away. Eat 15 grams of carbohydrate. This amount can be found in 4 ounces (½ cup) of fruit juice or 4 ounces of regular soft drink. Other examples are 2 tablespoons of raisins or 1 tube of glucose gel.
Check your blood sugar level again 10 to 15 minutes later. When it goes back to normal, eat a meal or snack to prevent another decrease in blood sugar. Left untreated, low blood sugar levels can lead to other serious conditions, such as seizures. It can become life-threatening.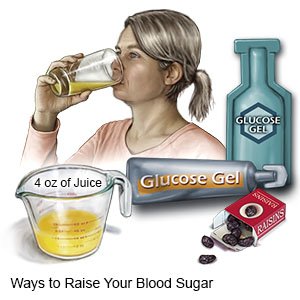
- Your blood sugar level can drop too low if you take insulin and do not eat enough food. Eat a snack in the evening to prevent low blood sugar levels at night. Do not skip meals.
- More physical activity can cause low blood sugar levels. Check your blood sugar level before your activity. If it is below 100 mg/dL, eat 15 grams of carbohydrate. If you will be active for more than 1 hour, check your blood sugar level every 30 minutes. You may need to adjust your insulin before activity and have a carbohydrate snack during activity.
What you can do to manage your blood sugar levels:
- Know what your blood sugar levels should be. Before meals , your blood sugar should be between 90 and 130 mg/dL. At bedtime , it should be between 90 and 150 mg/dL.
- Check your blood sugar level as directed and as needed.
- Look at your schedule. Make a plan for how you will check your blood sugar levels throughout the day.
- Check more often if you think your blood sugar is too high or too low. This will allow you to take care of any low or high blood sugar levels so they do not interfere with your activities.
- Rotate the sites where you do fingersticks. This will help make the checks less painful, and make fingerstick sites less noticeable.
- Write down your blood sugar levels so you can show them to your care team provider during your visits. Talk to your provider if you are having trouble keeping your blood sugar at the recommended levels.

- Take your insulin as directed. Your care team provider will teach you how and when to give yourself insulin injections or use an insulin pump or pen. Your provider can also teach you how to adjust your insulin dose.
More ways to manage type 1 diabetes:
- Wear medical alert jewelry or carry a card that says you have diabetes. Ask your care team provider where to get these items.

- Tell a friend or 2 that you have diabetes. Teach them what to do and who to call if you have problems.
- Make healthy food choices. Healthy foods can give you energy to learn and be active. They can also help you keep your blood sugar level in balance, and manage or lose weight safely. Work with a dietitian to develop a meal plan that works for you and your schedule. A dietitian can help you learn how to eat the right amount of carbs during your meals and snacks. Carbs can raise your blood sugar level if you eat too many at one time. Some foods that contain carbs include breads, cereals, French fries, chips, sweets, soft drinks, and juice.
- Be safe when you learn to drive. Check your blood sugar level before you drive. If your blood sugar is low, have 15 grams of carbohydrate and wait for it to go back to normal. Keep snacks that contain carbs in the car. If you feel like your blood sugar level is low, pull over and check it. Treat a low blood sugar level before you start driving again, if needed.
- Do not drink alcohol or use tobacco products, such as cigarettes. Alcohol affects your blood sugar level. You may not be aware of low blood sugar when you drink alcohol. Nicotine in tobacco products can damage blood vessels. Do not use e-cigarettes or smokeless tobacco in place of cigarettes or to help you quit. They still contain nicotine. Ask your diabetes care team provider for information if you currently smoke and need help quitting.
- Have screenings for complications of diabetes and other conditions that can happen with diabetes. You will need to be screened for kidney problems, high cholesterol, high blood pressure, blood vessel problems, eye problems, and eating disorders. Some screenings may begin right away and some may happen within the first 5 years of diagnosis. You will need to continue screenings through your lifetime. Keep your follow-up appointments with all providers.
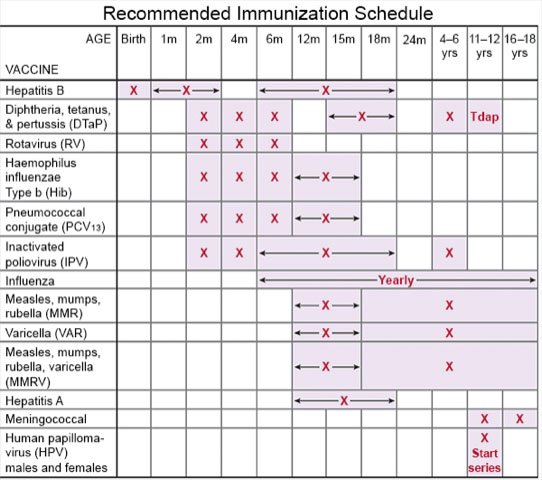
- Ask about vaccines you may need. You have a higher risk for serious illness if you get the flu, pneumonia, COVID-19, or hepatitis. Ask if you should get vaccines to prevent these or other diseases, and when to get the vaccines.
What you need to know about diabetes and pregnancy:
If you are female, talk to your care team provider about how to prevent an unplanned pregnancy. While you can have a safe pregnancy with diabetes, it is important to plan your pregnancy. Healthcare providers can help you have a healthy pregnancy and baby. Tell your care team provider immediately if you are pregnant or think you are pregnant.
Follow up with your care team providers as directed:
You may need to return to have your A1c every 3 months. An A1c test shows the average amount of sugar in your blood over the past 2 to 3 months. Your A1c should be less than 7.5%. You may also need to return at least 1 time each year to have your feet checked. Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2024 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Type 1 Diabetes Management for Adolescents
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
