Threatened Miscarriage
Medically reviewed by Drugs.com. Last updated on Apr 6, 2025.
What is a threatened miscarriage?
A threatened miscarriage occurs when you have vaginal bleeding within the first 20 weeks of pregnancy. This means that a miscarriage may happen. A threatened miscarriage may also be called a threatened abortion.
What causes bleeding or spotting during pregnancy?
The cause of your bleeding or spotting may not be known. The following are possible causes of vaginal bleeding during pregnancy:
- Polyps, fibroids, or cysts in the uterus
- Trauma to the cervix from past surgery, sexual intercourse, or an infection
- An infection such as vaginitis or cervicitis
- Problems with the uterus, placenta, or cervix
- Genetic problems in the fetus
- Drinking alcohol, smoking, or using drugs during pregnancy
- An ectopic pregnancy (the fetus grows outside of the uterus)
What are the signs and symptoms of a threatened miscarriage?
- Vaginal spotting or bleeding
- Pain or cramping in your abdomen or lower back
How is a threatened miscarriage diagnosed?
Your healthcare provider will ask about your symptoms and how far along you are in your pregnancy. Tell your provider when your bleeding started and if you have had any trauma to your abdomen. Tell your provider about any medical conditions you have and medicines you take. You may need any of the following:
- Blood and urine tests may show an infection or your pregnancy hormone level.
- A pelvic exam may show the size of your uterus and your cervix for dilation (opening).
- A pelvic ultrasound shows pictures of the fetus and checks for a heartbeat. It also looks at your reproductive organs and monitors the amount of bleeding. A pelvic ultrasound checks to make sure the fetus is not ectopic (outside of the uterus).
How is a threatened miscarriage managed?
Your healthcare provider may recommend any of the following to help decrease your risk for a miscarriage:
- Watchful waiting may be recommended. This means you do not need treatment. You will have regular exams to check for signs and symptoms of a miscarriage. You may need to return for blood tests and one or more ultrasounds.
- Rest as directed Rest will reduce physical strain on your pelvic area and help prevent your uterus from contracting. Rest may also help relief emotional stress.
- Medicines or supplements may be given to support your pregnancy, decrease abdominal pain, or treat an infection.
How can I care for myself?
The following may help you manage your symptoms and decrease your risk for a miscarriage:
- Do not put anything in your vagina. Do not have sex, douche, or use tampons. These actions may increase your risk for infection and miscarriage.
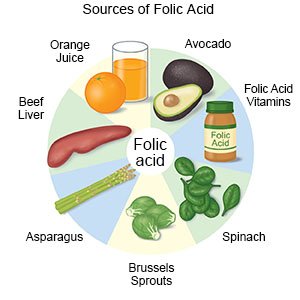
- Eat a variety of healthy foods. Take prenatal vitamins as directed. Healthy foods include fruits, vegetables, whole-grain breads, low-fat dairy products, beans, lean meats, and fish. Avoid raw or undercooked meat and fish. Ask your healthcare provider if you need a special diet.
Prenatal vitamins provide extra vitamins and minerals you need during pregnancy and may help decrease the risk of certain birth defects. You may have started taking prenatal vitamins or folic acid supplements 1 month or more before you became pregnant. Continue taking them for the first 2 to 3 months (8 to 12 weeks) of pregnancy. Always ask your provider before you take vitamins or nutritional supplements.
- Decrease your risk for an infection. Always wash your hands before you prepare or eat meals. Do not spend time with people who are sick. Ask your healthcare provider if you need immunizations such as the flu or hepatitis B vaccine. Immunizations may decrease your risk for infections that could cause a miscarriage.
- Manage your medical conditions. Keep your blood pressure and blood sugar under control. Maintain a healthy weight during pregnancy.
- Do not drink alcohol or use illegal drugs. Alcohol and drugs can increase your risk for a miscarriage or harm your baby.
- Do not smoke. Nicotine and other chemicals in cigarettes and cigars can harm your baby and cause miscarriage or preterm labor. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Do not use these products.
When should I seek immediate care?
- You feel weak, dizzy, or faint.
- You have severe abdominal pain even after you take pain medicine.
- You have vaginal bleeding that soaks 1 pad or more in an hour.
- You pass material that looks like tissue or large clots.
When should I call my doctor?
- You have a fever.
- You have trouble urinating, burning when you urinate, or feel a need to urinate often.
- You have new or worsening vaginal bleeding.
- You have vaginal pain or itching, or vaginal discharge that is yellow, green, or foul-smelling.
- You have extreme sadness or feel anxious and unable to cope.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
