Thoracentesis
Medically reviewed by Drugs.com. Last updated on Apr 6, 2025.
What is a thoracentesis?
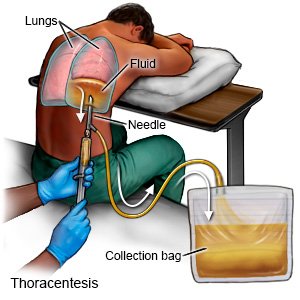
A thoracentesis is a procedure to remove extra fluid or air from between your lungs and your inner chest wall. Air or fluid buildup may make it hard for you to breathe. A thoracentesis allows your lungs to expand fully so you can breathe more easily.
How do I prepare for a thoracentesis?
- Your healthcare provider will tell you how to prepare for your procedure. You may need tests to check how well your blood clots. Tell your provider about all medicines you are taking, including blood thinners. You may need to stop taking certain medicines before the procedure. Your provider will tell you if you need to stop any medicines, and when to stop them. He or she will also tell you when to start taking them again after your procedure.
- Tell your healthcare provider if you have ever had an allergic reaction to anesthesia or a numbing medicine. Also tell your provider about any lung conditions you have, such as COPD.
- If you will be getting sedation, arrange to have someone drive you home after the procedure and stay with you. The person will need to watch for any reaction to the medicine.
- Your provider will talk to you about what to expect during the procedure. You may feel some pressure in your chest as the fluid or air is being removed. You will be asked not to cough or take a deep breath during the procedure. This is to help prevent a lung injury. A thoracentesis usually only takes about 15 minutes. Tell your provider if you have any concerns about being able to stay still and breathe as directed during the procedure.
Drugs used to treat this and similar conditions
Ozempic
Learn about Ozempic (semaglutide) for type 2 diabetes treatment, weight management, cardiovascular ...
Sterile talc
Sterile Talc Drug Information from Drugs.com. Includes side effects, interactions, indications
What will happen during a thoracentesis?
- You will be asked to sit in a chair and rest your arms on a table in front of you. Local anesthesia will be given to numb the area where the needle will be inserted. Your healthcare provider will insert the needle and move it between your ribs. He or she may use an ultrasound to help guide the needle.
- If your procedure is done to collect fluid for tests, a small amount of fluid is removed. Then the needle is removed and a dressing is placed over the area.
- If more fluid needs to be drained, a small plastic tube will be placed and the needle removed. The tube will be connected to a collection device and the fluid will slowly drain out. A device may be used to measure the pressure inside your chest. This will help your healthcare provider check if enough fluid has been drained. When enough fluid has drained out, the tube will be removed and the area will be covered with a bandage.
 |
What should I expect after a thoracentesis?
A chest x-ray may be needed to check that your lungs were not damaged during the procedure. You may also need any of the following after your procedure:
- A chest tube may be placed into your chest to drain extra fluid. The chest tube is attached to a container to collect the fluid.
- You may need extra oxygen if your blood oxygen level is lower than it should be. You may get oxygen through a mask placed over your nose and mouth or through small tubes placed in your nostrils. Ask your healthcare provider before you take off the mask or oxygen tubing.
- Pain medicine may be given.
- Antibiotics help fight or prevent an infection.
- Breathing treatments may help open your airways so you can breathe easier. A machine is used to change liquid medicine into a mist. You will breathe the mist into your lungs through tubing and a mouthpiece. Inhaled mist medicines act quickly on your airways and lungs to relieve your symptoms.
What are the risks of a thoracentesis?
Your lung may be punctured by the needle and collapse. You may bleed more than expected or get an infection from the procedure. You may also have chest pain, a cough, nausea, or feel lightheaded. Nerves, blood vessels, and nearby organs, such as your liver and spleen, may get damaged. Even after your procedure, the air or fluid in your chest may not drain completely. The air or fluid may build up again and you may need another thoracentesis.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
