Stroke Prevention
Medically reviewed by Drugs.com. Last updated on Apr 6, 2025.
What do I need to know about stroke prevention?
Stroke prevention includes making lifestyle changes and managing health conditions that can lead to a stroke. Your healthcare provider can help you create a plan that will be specific to your needs.
What increases my risk for a stroke?
You cannot control some risk factors. Examples are being older than 55 or African American, or having a family history of stroke. You can take action for any of the following risk factors:
- A personal history of transient ischemic attack (TIA)
- Diabetes or high cholesterol
- Atrial fibrillation, high blood pressure, or heart disease
- Smoking cigarettes, drinking alcohol, or using drugs such as cocaine
- Obesity or not enough physical activity
- Taking birth control pills, especially if you are older than 35 and use cigarettes
Which medicines are used to help prevent a stroke?
The type of medicine used depends on your stroke risk factors. Your healthcare provider may recommend any of the following:
- Blood thinners help prevent blood clots. Clots can cause strokes, heart attacks, and death. Many types of blood thinners are available. Your healthcare provider will give you specific instructions for the type you are given. The following are general safety guidelines to follow while you are taking a blood thinner:
- Watch for bleeding and bruising. Watch for bleeding from your gums or nose. Watch for blood in your urine and bowel movements. Use a soft washcloth on your skin, and a soft toothbrush to brush your teeth. This can keep your skin and gums from bleeding. If you shave, use an electric shaver. Do not play contact sports.
- Tell your dentist and other healthcare providers that you take a blood thinner. Wear a bracelet or necklace that says you take this medicine.
- Do not start or stop any other medicines or supplements unless your healthcare provider tells you to. Many medicines and supplements cannot be used with blood thinners.
- Take your blood thinner exactly as prescribed by your healthcare provider. Do not skip a dose or take less than prescribed. Tell your provider right away if you forget to take your blood thinner, or if you take too much.
- Blood pressure (BP) medicines may be given to help control hypertension (high BP). Antihypertensives can help lower your BP and keep it within your recommended range.
- Diuretics help decrease extra fluid that collects in your body. This helps lower your BP.
- Cholesterol medicine helps lower your cholesterol level. A low cholesterol level helps prevent heart disease and makes it easier to control your BP.
- Low-dose aspirin may be recommended to prevent blood clots. Your provider will tell you if you should take aspirin, and how much to take each day.
What lifestyle changes can I make to help prevent a stroke?
 |
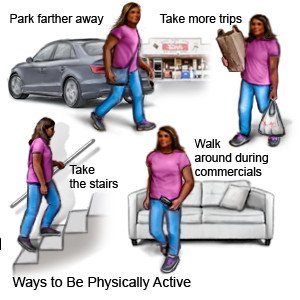
- Be physically active. Aim to get physical activity for at least 30 minutes a day, on most days of the week. You can break activity into 10 minute periods, 3 times during the day. Activity can lower your risk for problems that can lead to a stroke. Activity can control your blood pressure, cholesterol, weight, and blood sugar levels. Find an activity that you enjoy. This will make it easier for you to reach your activity goals.

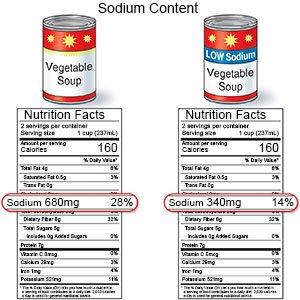
- Limit sodium (salt) as directed. Too much sodium can affect your fluid balance. Check labels to find low-sodium or no-salt-added foods. Some low-sodium foods use potassium salts for flavor. Too much potassium can also cause health problems. Your healthcare provider will tell you how much sodium and potassium are safe for you to have in a day. Your provider may recommend that you limit sodium to 2,300 mg a day.
- Follow the meal plan recommended by your provider. A dietitian or your provider can give you more information on low-sodium plans or the DASH (Dietary Approaches to Stop Hypertension) eating plan. The DASH plan is low in sodium, processed sugar, unhealthy fats, and total fat. It is high in potassium, calcium, and fiber. These can be found in vegetables, fruit, and whole-grain foods.

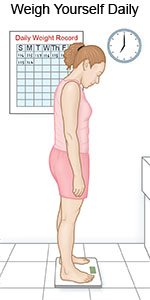
- Maintain a healthy weight. Extra body weight increases your risk for a stroke. Ask your provider what a healthy weight is for you. Your provider can help you create a weight loss plan, if needed.
- Talk to your provider about alcohol. Alcohol can raise your blood pressure. A drink of alcohol is 12 ounces of beer, 5 ounces of wine, or 1½ ounces of liquor. Your provider can help you set limits for the number of drinks you have within 24 hours and within a week. Your provider may recommend that you do not drink any alcohol.
- Do not use tobacco products. Nicotine and other chemicals in cigarettes and cigars can cause lung and heart damage. Heart and lung damage can increase your risk for a stroke. Ask your provider for information if you currently use tobacco products and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your provider before you use these products.
- Do not use illegal drugs. Cocaine and other illegal drugs can cause a stroke. Talk to your provider if you currently use illegal drugs and need help to quit.
- Manage stress. Stress can raise your blood pressure. Find ways to relax, such as deep breathing or listening to music.
How can I manage health conditions that can lead to a stroke?
- Manage your blood pressure (BP):
- Get regular BP screening. Screening can help find high BP early to lower your risk for a stroke. Your healthcare provider will give you directions to lower and control your BP.
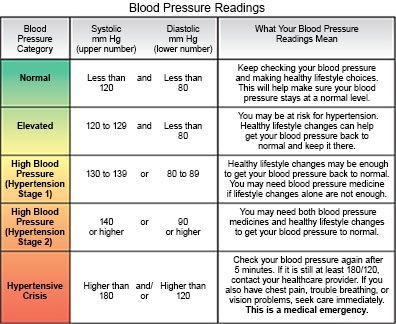
- Check your BP as directed. You can monitor your blood pressure at home. Ask your provider how often to check your blood pressure and what your blood pressure should be. Tell your provider if your blood pressure is higher than recommended. Your provider may need to change your medicine or help you make changes to your nutrition or exercise plan.

- Get regular BP screening. Screening can help find high BP early to lower your risk for a stroke. Your healthcare provider will give you directions to lower and control your BP.
- Manage diabetes. Control of your blood sugar levels may decrease your risk for a stroke. If you take diabetes medicine or insulin, take it as directed. Healthy foods and regular exercise also help lower your blood sugar levels. Monitor your levels as directed. Keep a record of your blood sugar levels and bring them to your appointments. This will help your provider make changes to your medicines. It may also help you find ways to get better control of your diabetes.

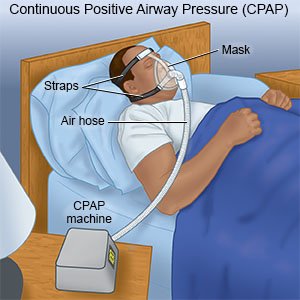
- Manage sleep apnea. Sleep apnea can cause stroke risk factors, such as high blood pressure, heart failure, or heart rhythm problems. Get screened and treated for sleep apnea. Talk to your provider about devices that help prevent complications from sleep apnea. You may need to use a CPAP or BiPAP machine while you sleep. These machines increase your oxygen levels and keep your airway open.
- Manage other medical conditions that increase your risk for a stroke. Atrial fibrillation (a-fib) can cause blood clots. Medicines or procedures may be used to control a-fib. Patent foramen ovale (PFO) can also lead to a stroke. Your provider may recommend you have surgery to close a PFO, if needed. Sickle cell disease, or sickle cell anemia, can cause blockages in blood vessels. The blockages may need to be removed during surgery. Depression and anxiety can stress your heart. Stress may lead to high blood pressure or heart disease. Talk to your provider about treatment for depression or anxiety.
- Talk to your provider about risk factors if you are female. Birth control pills increase your risk, especially if you are older than 35 or use cigarettes. Talk to your provider about other forms of contraception. Premature and early menopause may increase your risk for stroke. Talk to your provider about hormone replacement therapy to reduce your risk for a stroke.
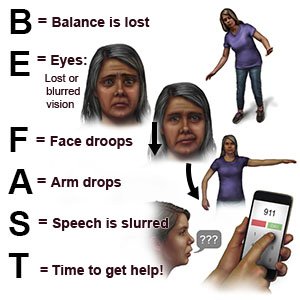
Call your local emergency number (911 in the US) or have someone call if:
- You have any of the following signs of a stroke:
- Numbness or drooping on one side of your face
- Weakness in an arm or leg
- Confusion or difficulty speaking
- Dizziness, a severe headache, or vision loss
- You have chest pain or shortness of breath.
When should I seek immediate care?
- Your arm or leg feels warm, tender, and painful. It may look swollen and red.
When should I call my doctor?
- Your blood sugar level or blood pressure is higher or lower than recommended.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
