Salter-Harris Fracture
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is a Salter-Harris fracture?
A Salter-Harris fracture is a break in your child's bone that goes through a growth plate. Growth plates are tissue that forms new bone on the ends of certain bones to make them longer as your child grows. Examples include thigh bones, forearm bones, and finger bones. When your child is finished growing, the growth plates will harden and become solid bone.
What are the types of Salter-Harris fractures?
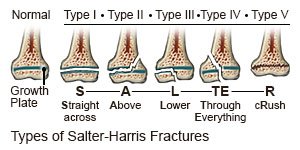 |
- Type 1 fractures are a complete break through the growth plate.
- Type 2 fractures break through the growth plate and crack through part of the bone shaft (long part of the bone).
- Type 3 fractures go through part of the growth plate and crack through part of the bone end.
- Type 4 fractures go through part of the bone shaft, growth plate, and bone end.
- Type 5 fractures occur when the growth plate is crushed.
What increases my child's risk for a Salter-Harris fracture?
- Not being fully grown, especially teenaged boys who play sports
- Being a gymnast, basketball player, or football player, or doing hard sports training over time
- A fall from a bike, skateboard, or skis
- The force from a car, motorcycle, or all-terrain vehicle (ATV) accident
- A hard pull or twist to the arm or leg that breaks the growth plate
What are the signs and symptoms of a Salter-Harris fracture?
- Pain and swelling
- Tenderness
- A change in the shape of the injured area that is different than usual
- Not being able to move or put weight on the injured arm or leg
How is a Salter-Harris fracture diagnosed?
Your child's healthcare provider will examine your child and ask when symptoms began. The provider will ask how an injury happened. He or she will gently press on the area to check for swelling and tenderness. He or she will ask your child to show where it hurts and to move the area if possible. X-rays will be used to check for a fracture. CT or MRI pictures may also be needed. Your child may be given contrast liquid to help his or her bones show up better in the pictures. Tell the healthcare provider if your child has ever had an allergic reaction to contrast liquid. Do not let your child enter the MRI room with anything metal. Metal can cause serious injury. Tell the healthcare provider if your child has any metal in or on his or her body.
How is a Salter-Harris fracture treated?
Treatment depends on the type of fracture your child has and how severe it is:
- Prescription pain medicine may be given. Ask your child's healthcare provider how to give this medicine safely. Some prescription pain medicines contain acetaminophen. Do not give your child other medicines that contain acetaminophen without talking to his or her healthcare provider. Too much acetaminophen may cause liver damage. Prescription pain medicine may cause constipation. Ask your child's healthcare provider how to prevent or treat constipation.
- A cast or splint may be used to help prevent movement in the injured area until more treatment is done. Some Salter-Harris fractures take up to 14 days before they can be seen on an x-ray. Your child's injury may need to be put in a cast or splint if a Salter-Harris fracture is known or suspected. This will help prevent more injury to the growth plate and surrounding bone. If the bone is not displaced (moved out of place), your child may get a cast to secure the bone as it heals. Casts are also used after reduction (when the bone is put back into place) or surgery.
- Surgery may be needed to repair certain types of Salter-Harris fractures. Pins or screws will be placed inside the broken bone. These hold the bone pieces together in the correct places.
What can I do to help my child's fracture heal?
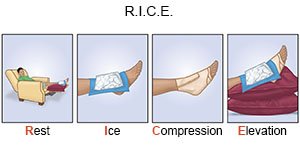 |
- Rest may help your child's fracture heal, and help manage pain. Help your child rest often during the day.
- Elevate the area above the level of your child's heart, as often as possible, for 1 to 3 days. Your child may lie back in a bed or chair and put pillows under an injured leg or foot. Use pillows to prop up the area. Your child should wiggle his or her fingers and toes often to keep blood flowing.
- Ice helps decrease pain and swelling. Put crushed ice in a plastic bag and cover it with a towel. Place the ice over the cast or splint for as long and as often as your child's healthcare provider says you should.
How can sports injuries be prevented?
- Take your child for regular checkups as directed. Ask your child to tell you when he or she is hurt. Regular checkups may catch unknown injuries before they get worse.
- Have your child do different exercises. Your child should not do the same exercises or drills every day.
- Teach your child to play safely. Make sure your child competes with other children of the same size, fitness level, and skill.
- Have your child rest during sports activities as directed. Rest periods are needed during sports training. If your child is injured, he or she may need to avoid contact sports for 4 to 6 months to prevent another injury.
When should I seek immediate care?
- Your child's pain gets worse, even with medicine.
- The skin under your child's cast or splint is tingling or numb.
- Your child can no longer move his or her fingers or toes.
When should I call my child's doctor?
- Your child has a fever.
- Your child says his or her cast or splint feels too tight.
- You see swelling below the splint or cast.
- Your child's cast is cracked or has soft spots.
- You have questions or concerns about your child's condition or care.
Care Agreement
You have the right to help plan your child's care. Learn about your child's health condition and how it may be treated. Discuss treatment options with your child's healthcare providers to decide what care you want for your child. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
